- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Respiratory examination frequently appears in OSCEs and you’ll be expected to pick up the relevant clinical signs using your examination skills. This respiratory examination OSCE guide provides a clear step-by-step approach to examining the respiratory system, with an included video demonstration.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language.
Gain consent to proceed with the examination.
Adjust the head of the bed to a 45° angle.
Adequately expose the patient’s chest for the examination (offer a blanket to allow exposure only when required and if appropriate, inform patients they do not need to remove their bra). Exposure of the patient’s lower legs is also helpful to assess for peripheral oedema.
Ask the patient if they have any pain before proceeding with the clinical examination.
General inspection
Clinical signs
Inspect the patient from the end of the bed whilst at rest, looking for clinical signs suggestive of underlying pathology:
- Age: the patient’s approximate age is helpful when considering the most likely underlying pathology, with younger patients more likely to have diagnoses such as asthma or cystic fibrosis (CF) and older patients more likely to have chronic obstructive pulmonary disease (COPD), interstitial lung disease or malignancy.
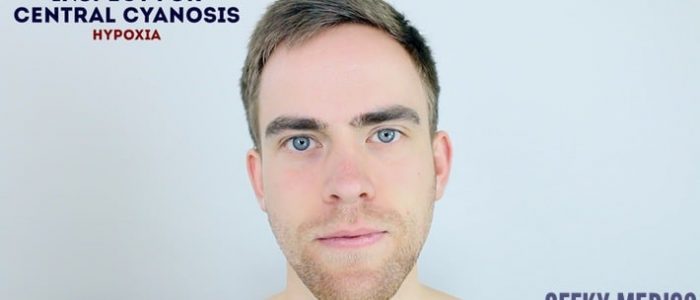
- Cyanosis: bluish discolouration of the skin due to poor circulation (e.g. peripheral vasoconstriction secondary to hypovolaemia) or inadequate oxygenation of the blood (e.g. right-to-left cardiac shunting).
- Shortness of breath: signs may include nasal flaring, pursed lips, use of accessory muscles, intercostal muscle recession and the tripod position (sitting or standing leaning forward and supporting the upper body with hands on knees or other surfaces). Shortness of breath is a common feature of most respiratory pathology, however possible underlying diagnoses in an OSCE could include asthma, pulmonary oedema, pulmonary fibrosis, lung cancer and COPD. The inability to speak in full sentences is an indicator of significant shortness of breath.
- Cough: a productive cough can be associated with several respiratory pathologies including pneumonia, bronchiectasis, COPD and CF. A dry cough may suggest a diagnosis of asthma or interstitial lung disease.
- Wheeze: a continuous, coarse, whistling sound produced in the respiratory airways during breathing. Wheeze is often associated with asthma, COPD and bronchiectasis.
- Stridor: a high-pitched extra-thoracic breath sound resulting from turbulent airflow through narrowed upper airways. Stridor has a wide range of causes, including foreign body inhalation (acute) and subglottic stenosis (chronic).
- Pallor: a pale colour of the skin that can suggest underlying anaemia (e.g. haemorrhage/chronic disease) or poor perfusion (e.g. congestive cardiac failure). It should be noted that healthy individuals may have a pale complexion that mimics pallor.
- Oedema: typically presents with swelling of the limbs (e.g. pedal oedema) or abdomen (i.e. ascites) and is often associated with right ventricular failure. Pulmonary oedema often occurs secondary to left ventricular failure.
- Cachexia: ongoing muscle loss that is not entirely reversed with nutritional supplementation. Cachexia is commonly associated with underlying malignancy (e.g. lung cancer) and other end-stage respiratory diseases (e.g. COPD).
Objects and equipment
Look for objects or equipment on or around the patient that may provide useful insights into their medical history and current clinical status:
- Oxygen delivery devices: note the type of oxygen device (e.g. Venturi mask, non-rebreathing mask, nasal cannulae) and the current flow rate of oxygen (e.g. 2L, 4L, 10L, 15L). Look for other forms of respiratory support such as CPAP or BiPAP.
- Sputum pot: note the volume and colour of the contents (e.g. COPD/bronchiectasis).
- Other medical equipment: ECG leads, medications (e.g. inhalers/nebulisers in asthma/COPD), catheters (note volume/colour of urine) and intravenous access.
- Cigarettes or vaping equipment: smoking is a significant risk factor for lung cancer and chronic lung disease (e.g. COPD).
- Mobility aids: items such as wheelchairs and walking aids give an indication of the patient’s current mobility status.
- Vital signs: charts on which vital signs are recorded will give an indication of the patient’s current clinical status and how their physiological parameters have changed over time.
- Fluid balance: fluid balance charts will give an indication of the patient’s current fluid status which may be relevant if a patient appears fluid overloaded or dehydrated.
- Prescriptions: prescribing charts or personal prescriptions can provide useful information about the patient’s recent medications.
Hands
The hands can provide lots of clinically relevant information and therefore a focused, structured assessment is essential.
Inspection
General observations
Observe the hands and note your findings:
- Colour: cyanosis of the hands may suggest underlying hypoxaemia.
- Tar staining: caused by smoking, a significant risk factor for respiratory disease (e.g. COPD, lung cancer).
- Skin changes: bruising and thinning of the skin can be associated with long-term steroid use (e.g. asthma, COPD, interstitial lung disease).
- Joint swelling or deformity: may be associated with rheumatoid arthritis which has several extra-articular manifestations that affect the respiratory system (e.g. pleural effusions/pulmonary fibrosis).
Finger clubbing
Finger clubbing involves uniform soft tissue swelling of the terminal phalanx of a digit with subsequent loss of the normal angle between the nail and the nail bed. Finger clubbing is associated with several underlying disease processes, but those most likely to appear in a respiratory OSCE station include lung cancer, interstitial lung disease, cystic fibrosis and bronchiectasis.
To assess for finger clubbing:
- Ask the patient to place the nails of their index fingers back to back.
- In a healthy individual, you should be able to observe a small diamond-shaped window (known as Schamroth’s window).
- When finger clubbing develops, this window is lost
Fine tremor
Assess for the presence of a fine tremor:
- Ask the patient to hold out their hands in an outstretched position and observe for a fine tremor which is typically associated with beta-2-agonist use (e.g. salbutamol).
Asterixis (flapping tremor)
Asterixis (also known as ‘flapping tremor’) is a type of negative myoclonus characterised by irregular lapses of posture causing a flapping motion of the hands. In the context of a respiratory examination, the most likely underlying cause is CO2 retention in conditions that result in type 2 respiratory failure (e.g. COPD). Other causes of asterixis include uraemia and hepatic encephalopathy.
- Whilst the patient still has their hands stretched outwards, ask them to cock their hands backwards at the wrist joint and hold the position for 30 seconds.
- Observe for evidence of asterixis during this time period.
Palpation
Temperature
Place the dorsal aspect of your hand onto the patient’s to assess temperature:
- In healthy individuals, the hands should be symmetrically warm, suggesting adequate perfusion.
- Cool hands may suggest poor peripheral perfusion.
- Excessively warm and sweaty hands can be associated with CO2 retention.
Heart rate
Assessing heart rate:
- Palpate the patient’s radial pulse, located at the radial side of the wrist, with the tips of your index and middle fingers aligned longitudinally over the course of the artery.
- Once you have located the radial pulse, assess the rate and rhythm.
Calculating heart rate:
- You can calculate the heart rate in a number of ways, including measuring for 60 seconds, measuring for 30 seconds and multiplying by 2 or measuring for 15 seconds and multiplying by 4. The shorter the interval used, the higher the risk of obtaining an inaccurate result, so wherever possible, you should palpate for a full 60 seconds.
- For irregular rhythms, you should measure the pulse for a full 60 seconds to improve accuracy.
Pulse abnormalities
- Bounding pulse: can be associated with underlying CO2 retention (e.g. type 2 respiratory failure).
- Pulsus paradoxus: pulse wave volume decreases significantly during the inspiratory phase. This is a late sign of cardiac tamponade, severe acute asthma and severe exacerbations of COPD (therefore it is unlikely to be relevant to most OSCE scenarios).
Respiratory rate
Assessing respiratory rate:
- Whilst still palpating the radial pulse (but no longer counting it), assess the patient’s respiratory rate (palpation of the radial pulse at this stage purely to avoid making the patient aware you are directly observing their breathing, as this can itself alter the respiratory rate).
- Note any asymmetries in the expiratory and inspiratory phases of respiration (e.g. the expiratory phase is often prolonged in asthma exacerbations and in patients with COPD).
Calculating respiratory rate:
- Assess the patient’s respiratory rate for 60 seconds to calculate the number of breaths per minute.
Respiratory rate abnormalities
- In healthy adults, the respiratory rate should be between 12-20 breaths per minute.
- A respiratory rate of fewer than 12 breaths per minute is referred to as bradypnoea (e.g. opiate overdose).
- A respiratory rate of more than 20 breaths per minute is referred to as tachypnoea (e.g. acute asthma).
Jugular venous pressure (JVP)
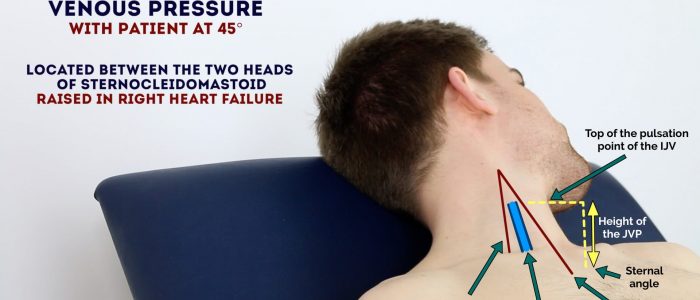
Jugular venous pressure (JVP) provides an indirect measure of central venous pressure. This is possible because the internal jugular vein (IJV) connects to the right atrium without any intervening valves, resulting in a continuous column of blood. The presence of this continuous column of blood means that changes in right atrial pressure are reflected in the IJV (e.g. raised right atrial pressure results in distension of the IJV).
The IJV runs between the medial end of the clavicle and the ear lobe, under the medial aspect of the sternocleidomastoid, making it difficult to visualise (its double waveform pulsation is, however, sometimes visible due to transmission through the sternocleidomastoid muscle).
Because of the inability to easily visualise the IJV, it’s tempting to use the external jugular vein (EJV) as a proxy for assessment of central venous pressure during clinical assessment. However, because the EJV typically branches at a right angle from the subclavian vein (unlike the IJV which sits in a straight line above the right atrium) it is a less reliable indicator of central venous pressure.
See our guide to jugular venous pressure (JVP) for more details.
Measure the JVP
1. Position the patient in a semi-recumbent position (at 45°).
2. Ask the patient to turn their head slightly to the left.
3. Inspect for evidence of the IJV, running between the medial end of the clavicle and the ear lobe, under the medial aspect of the sternocleidomastoid (it may be visible between just above the clavicle between the sternal and clavicular heads of the sternocleidomastoid. The IJV has a double waveform pulsation, which helps to differentiate it from the pulsation of the external carotid artery.
4. Measure the JVP by assessing the vertical distance between the sternal angle and the top of the pulsation point of the IJV (in healthy individuals, this should be no greater than 3 cm).
Respiratory causes of a raised JVP
A raised JVP indicates the presence of venous hypertension. Respiratory causes of a raised JVP include:
- Pulmonary hypertension: causes right-sided heart failure, often occurring due to COPD or interstitial lung disease.
- There are several other causes of a raised JVP that relate to the cardiovascular system (e.g. congestive heart failure, tricuspid regurgitation and constrictive pericarditis).
Hepatojugular reflux test
The hepatojugular reflux test involves the application of pressure to the liver whilst observing for a sustained rise in JVP. See our cardiovascular examination guide for details on how to elicit hepatojugular reflux.
Face
General
Inspect the face for any signs relevant to the respiratory system:
- Plethoric complexion: a congested red-faced appearance associated with polycythaemia (e.g. COPD) and CO2 retention (e.g. type 2 respiratory failure).
Eyes
Inspect the eyes for signs relevant to the respiratory system:
- Conjunctival pallor: suggestive of underlying anaemia. Ask the patient to gently pull down their lower eyelid to allow you to inspect the conjunctiva.
- Ptosis, miosis and enophthalmos: all features of Horner’s syndrome (anhydrosis is another important sign associated with the syndrome). Horner’s syndrome occurs when the sympathetic trunk is damaged by pathology such as lung cancer affecting the apex of the lung (e.g. Pancoast tumour).
Mouth
Inspect the mouth for signs relevant to the respiratory system:
- Central cyanosis: bluish discolouration of the lips and/or the tongue associated with hypoxaemia.
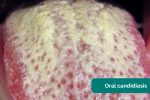
- Oral candidiasis: a fungal infection commonly associated with steroid inhaler use (due to local immunosuppression). It is characterised by pseudomembranous white slough which can be easily wiped away to reveal underlying erythematous mucosa.
Inspection of the chest
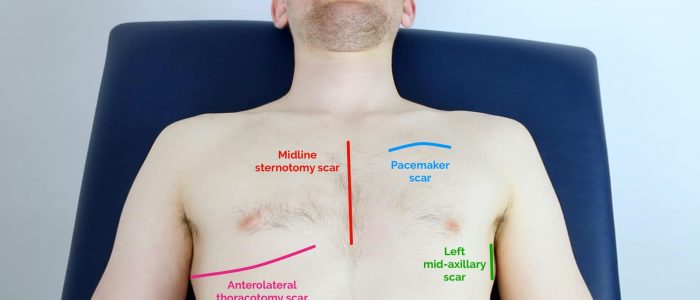
Scars
Closely inspect the chest wall for scars and other abnormalities:
- Median sternotomy scar: located in the midline of the thorax. This surgical approach is used for cardiac valve replacement and coronary artery bypass grafts (CABG).
- Axillary thoracotomy scar: located between the posterior border of the pectoralis major and anterior border of latissimus dorsi muscles, through the 4th or 5th intercostal space. This surgical approach is used for the insertion of chest drains.
- Posterolateral thoracotomy scar: located between the scapula and mid-spinal line, extending laterally to the anterior axillary line. This surgical approach is used for lobectomy, pneumonectomy and oesophageal surgery.
- Infraclavicular scar: located in the infraclavicular region (on either side). This surgical approach is used for pacemaker insertion.
- Radiotherapy-associated skin changes: may be present in patients who have been treated for lung cancer. Clinical features can include xerosis (dry skin), scale, hyperkeratosis (thickened skin), depigmentation and telangiectasia.
Chest wall deformities
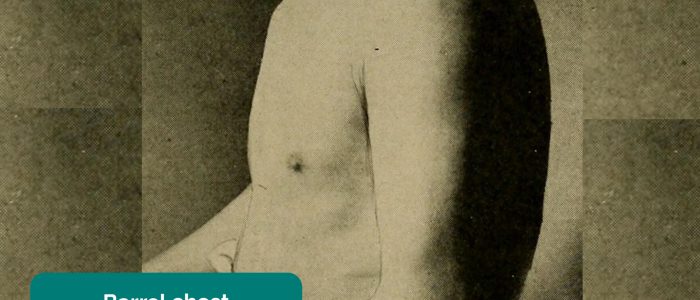
Inspect for evidence of chest wall deformities:
- Asymmetry: typically associated with pneumonectomy (e.g. lung cancer) and thoracoplasty (e.g. tuberculosis).
- Pectus excavatum: a caved-in or sunken appearance of the chest.
- Pectus carinatum: protrusion of the sternum and ribs.
- Hyperexpansion (a.k.a. ‘barrel chest’): chest wall appears wider and taller than normal. Associated with chronic lung diseases such as asthma and COPD.
Trachea and cricosternal distance
Assess tracheal position
Gently assess the position of the trachea, which should be central in healthy individuals (this can be uncomfortable, so warn the patient in advance):
1. Ensure patient’s neck musculature is relaxed by asking them to position their chin slightly downwards.
2. Dip your index finger into the thorax beside the trachea.
3. Gently apply side pressure to locate the border of the trachea.
4. Compare this space to the other side of the trachea using the same process.
5. A difference in the amount of space between the sides suggests the presence of tracheal deviation.
Causes of tracheal deviation
- The trachea deviates away from tension pneumothorax and large pleural effusions.
- The trachea deviates towards lobar collapse and pneumonectomy.
- Palpation of the trachea can be uncomfortable, so warn the patient and apply a gentle technique
Assess cricosternal distance
Cricosternal distance is the distance between the inferior border of the cricoid cartilage and the suprasternal notch:
1. Measure the distance between the suprasternal notch and cricoid cartilage using your fingers.
2. In healthy individuals, the distance should be 3-4 fingers.
Cricosternal distance is actually based on the size of the patient’s fingers so if their fingers are significantly different in size from your own, it may be worth using their fingers for the assessment.
Causes of abnormal cricosternal distance
A distance of fewer than 3 fingers suggests underlying lung hyperinflation (e.g. asthma, COPD).
Palpation of the chest
Palpate the apex beat
1. Palpate the apex beat with your fingers placed horizontally across the chest.
2. In healthy individuals, it is typically located in the 5th intercostal space in the midclavicular line.
Causes of a displaced apex beat
Respiratory causes of a displaced apex beat:
- Right ventricular hypertrophy (e.g. pulmonary hypertension, COPD, interstitial lung disease)
- Large pleural effusion
- Tension pneumothorax
Assess chest expansion
1. Place your hands on the patient’s chest, inferior to the nipples.
2. Wrap your fingers around either side of the chest.
3. Bring your thumbs together in the midline, so that they touch.
4. Ask the patient to take a deep breath in.
5. Observe the movement of your thumbs (in healthy individuals they should move symmetrically upwards/outwards during inspiration and symmetrically downwards/inwards during expiration ).
6. Reduced movement of one of your thumbs indicates reduced chest expansion on that side.
Respiratory causes of reduced chest expansion
- Symmetrical: pulmonary fibrosis reduces lung elasticity, restricting overall chest expansion.
- Asymmetrical: pneumothorax, pneumonia and pleural effusion would all cause ipsilateral reduced chest expansion.
Percussion of the chest
Percussion of the chest involves listening to the volume and pitch of percussion notes across the chest to identify underlying pathology. Correct technique is essential to generating effective percussion notes.
Percussion technique
1. Place your non-dominant hand on the patient’s chest wall.
2. Position your middle finger over the area you want to percuss, firmly pressed against the chest wall.
3. With your dominant hand’s middle finger, strike the middle phalanx of your non-dominant hand’s middle finger using a swinging movement of the wrist.
4. The striking finger should be removed quickly, otherwise, you may muffle the resulting percussion note.
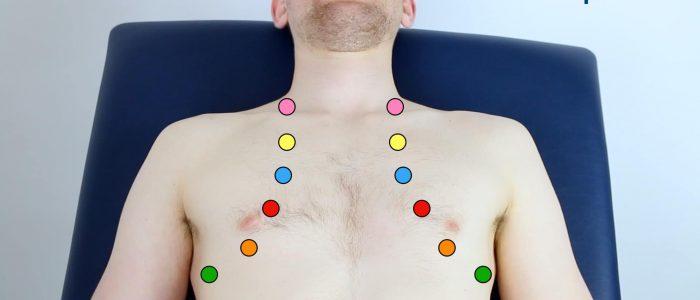
Areas to percuss
Percuss the following areas of the chest, comparing side to side as you progress (see image example below):
- Supraclavicular region: lung apices
- Infraclavicular region
- Chest wall: percuss over 3-4 locations bilaterally
- Axilla
Types of percussion note
- Resonant: a normal finding (listen to the example in the video demonstration).
- Dullness: suggests increased tissue density (e.g. cardiac dullness, consolidation, tumour, lobar collapse).
- Stony dullness: typically caused by an underlying pleural effusion.
- Hyper-resonance: the opposite of dullness, suggestive of decreased tissue density (e.g. pneumothorax).
Tactile vocal fremitus
Assessing tactile vocal fremitus involves palpating over different areas of the chest wall whilst the patient repeats a word or number consistently (e.g. “ninety-nine”). The presence of increased tissue density or fluid affects the strength at which the patient’s speech is transmitted as vibrations through the chest wall to the examiner’s hands.
Technique
1. Ask the patient to say “99” repeatedly at the same volume and in the same tone.
2. Palpate the chest wall on both sides, using the ulnar border of your hand.
3. Cover all major regions of the chest wall, comparing each side at each location.
Abnormal tactile vocal fremitus
- Increased vibration over an area suggests increased tissue density (e.g. consolidation, tumour, lobar collapse).
- Decreased vibration over an area suggests the presence of fluid or air outside of the lung (e.g. pleural effusion, pneumothorax).
An alternative method of assessment
Vocal resonance (see below) is an alternative method of assessing the conduction of sound through lung tissue and involves auscultating over different areas of the chest wall whilst the patient repeats a word or number consistently. The presence of increased tissue density or fluid affects the volume at which the patient’s speech is transmitted to the diaphragm of the stethoscope. Given both tests assess the same thing, there is no reason to perform both vocal resonance and tactile vocal fremitus in the same examination.
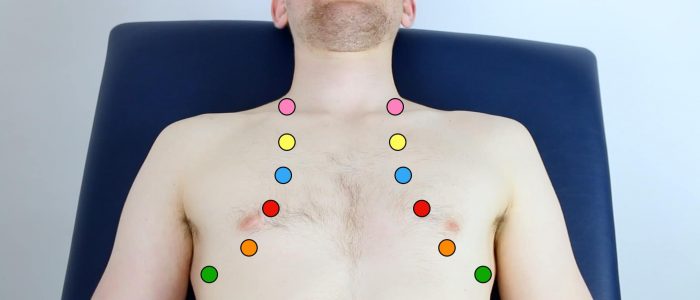
Auscultation of the chest
When auscultating the chest, it is important that you have a systematic approach that allows you to compare each area on both the left and the right as you progress.
Auscultate the chest
Technique
1. Ask the patient to relax and breathe deeply in and out through their mouth (prolonged deep breathing should, however, be avoided).
2. Position the diaphragm of the stethoscope over each of the relevant locations on the chest wall to ensure all lung regions have been assessed and listen to the breathing sounds during inspiration and expiration. Assess the quality and volume of breath sounds and note any added sounds.
3. Auscultate each side of the chest at each location to allow for direct comparison and increased sensitivity at detecting local abnormalities.
Quality of breath sounds
- Vesicular: the normal quality of breath sounds in healthy individuals.
- Bronchial: harsh-sounding (similar to auscultating over the trachea), inspiration and expiration are equal and there is a pause between. This type of breath sound is associated with consolidation.
Volume of breath sounds
- Quiet breath sounds: suggest reduced air entry into that region of the lung (e.g pleural effusion, pneumothorax).
- When presenting your findings, state ‘reduced breath sounds’, rather than ‘reduced air entry’.
Added sounds
- Wheeze: a continuous, coarse, whistling sound produced in the respiratory airways during breathing. Wheeze is often associated with asthma, COPD and bronchiectasis.
- Stridor: a high-pitched extra-thoracic breath sound resulting from turbulent airflow through narrowed upper airways. Stridor has a wide range of causes, including foreign body inhalation (acute) and subglottic stenosis (chronic).
- Coarse crackles: discontinuous, brief, popping lung sounds typically associated with pneumonia, bronchiectasis and pulmonary oedema.
- Fine end-inspiratory crackles: often described as sounding similar to the noise generated when separating velcro. Fine end-inspiratory crackles are associated with pulmonary fibrosis.
Assess vocal resonance
Assessing vocal resonance involves auscultating over different areas of the chest wall whilst the patient repeats a word or number consistently. The presence of increased tissue density or fluid affects the volume at which the patient’s speech is transmitted to the diaphragm of the stethoscope.
Technique
1. Ask the patient to say “99” repeatedly at the same volume and in the same tone.
2. Auscultate all major regions of the anterior chest wall, comparing each side at each location.
Abnormal vocal resonance
- Increased volume over an area suggests increased tissue density (e.g. consolidation, tumour, lobar collapse).
- Decreased volume over an area suggests the presence of fluid or air outside of the lung (e.g. pleural effusion, pneumothorax).
An alternative method of assessment
Tactile vocal fremitus is an alternative method of assessing the conduction of sound through lung tissue and involves feeling for sound vibrations on the chest wall with your hands as the patient speaks. Given both tests assess the same thing, there is no reason to perform both vocal resonance and tactile vocal fremitus in the same examination.
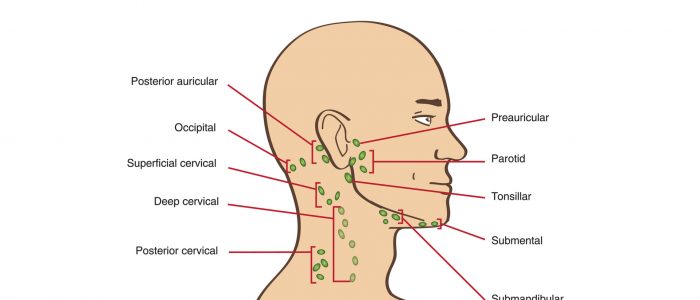
Lymph nodes
Palpate the patient’s lymph nodes
1. Position the patient sitting upright and examine from behind if possible. Ask the patient to tilt their chin slightly downwards to relax the muscles of the neck and aid palpation of lymph nodes. You should also ask them to relax their hands in their lap.
2. Inspect for any evidence of lymphadenopathy or irregularity of the neck.
3. Stand behind the patient and use both hands to start palpating the neck.
4. Use the pads of the second, third and fourth fingers to press and roll the lymph nodes over the surrounding tissue to assess the various characteristics of the lymph nodes. By using both hands (one for each side) you can note any asymmetry in size, consistency and mobility of lymph nodes.
5. Start in the submental area and progress through the various lymph node chains. Any order of examination can be used, but a systematic approach will ensure no areas are missed:
- Submental
- Submandibular
- Pre-auricular
- Post-auricular
- Superficial cervical
- Deep cervical
- Posterior cervical
- Supraclavicular – left supraclavicular region is where Virchow’s node may be noted (associated with upper gastrointestinal malignancy)
Take caution when examining the anterior cervical chain that you do not compromise cerebral blood flow (due to carotid artery compression). It may be best to examine one side at a time here.
A common mistake is a “piano-playing” or “spider’s legs” technique with the fingertips over the skin rather than correctly using the pads of the second, third and fourth fingers to press and roll the lymph nodes over the surrounding tissue.
Example of logical systematic examination of the lymph nodes
1. Start under the chin (submental lymph nodes), then move posteriorly palpating beneath the mandible (submandibular), turn upwards at the angle of the mandible and feel anterior (preauricular lymph nodes) and posterior to the ears (posterior auricular lymph nodes).
2. Follow the anterior border of the sternocleidomastoid muscle (anterior cervical chain) down to the clavicle, then palpate up behind the posterior border of the sternocleidomastoid (posterior cervical chain) to the mastoid process.
3. Ask the patient to tilt their head (bring their ear towards their shoulder) each side in turn, and palpate behind the posterior border of the clavicle in the supraclavicular fossa (supraclavicular and infraclavicular lymph nodes).
Respiratory causes of lymphadenopathy
- Lung cancer with metastases
- Tuberculosis
- Sarcoidosis
Posterior chest assessment
With the patient still sitting forwards, ask them to fold their arms across their chest so that their hands are touching the opposite shoulder. This results in rotation of the scapulae to better expose the underlying chest wall for assessment.
Assess the posterior chest including inspection, chest expansion, percussion, tactile vocal fremitus (or vocal resonance) and auscultation.
Allocate adequate time to assessing the posterior aspect of the chest as this is where you are most likely to identify clinical signs.
Final steps
Assess for evidence of pitting sacral and pedal oedema (e.g. congestive heart failure).
Assess the calves for signs of deep vein thrombosis (e.g. swelling, increased temperature, erythema, visible superficial veins) as the patient may have shortness of breath secondary to pulmonary embolism.
Inspect for evidence of erythema nodosum, which can be associated with sarcoidosis.
To complete the examination…
Explain to the patient that the examination is now finished.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I examined Mrs Smith, a 64-year-old female. On general inspection, the patient appeared comfortable at rest, with no evidence of shortness of breath. There were no objects or medical equipment around the bed of relevance.”
“The hands had no peripheral stigmata of respiratory disease and were symmetrically warm. There was no evidence of a fine tremor or asterixis.”
“The pulse was regular at 70 beats per minute and the respiratory rate was 16 breaths per minute.”
“On inspection of the face, there were no stigmata of respiratory disease.”
“Assessment of the JVP did not reveal any abnormalities. The trachea was centrally located and the cricosternal distance was within the normal range.”
“Closer inspection of the chest did not reveal any scars or chest wall deformities. The apex beat was palpable in the 5th intercostal space, in the mid-clavicular line and chest expansion was equal.”
“Percussion of the chest revealed normal resonance throughout all lung fields.”
“Auscultation of the chest revealed normal vesicular breath sounds, with no added sounds. Vocal resonance was also normal.”
“There was no lymphadenopathy on assessment.”
“There was no evidence of peripheral oedema and the calves were soft and non-tender.”
“In summary, these findings are consistent with a normal respiratory examination.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
Suggest further assessments and investigations to the examiner:
- Check oxygen saturation (SpO2) and provide supplemental oxygen if indicated.
- Check other vital signs including temperature and blood pressure.
- Take a sputum sample.
- Perform peak flow assessment if relevant (e.g. asthma)
- Request a chest X-ray (if abnormalities were noted on examination)
- Take an arterial blood gas if indicated (also see ABG interpretation)
- Perform a full cardiovascular examination if indicated (e.g. cor pulmonale)
Reviewer
Dr Gareth Hynes
Respiratory Registrar
References
- Respiratory sounds. Provided by EasyAuscultation and Andy Howes.
- Adapted by Geeky Medics. James Heilman, MD. Cyanosis. Licence: CC BY-SA.
- Adapted by Geeky Medics. James Heilman, MD. Peripheral pallor. Licence: CC BY-SA.
- Adapted by Geeky Medics. James Heilman, MD. Tar staining. Licence: CC BY-SA.
- Adapted by Geeky Medics. Desherinka. Finger clubbing. Licence: CC BY-SA.
- Adapted by Geeky Medics. Waster. Horner’s syndrome. Licence: CC BY.
- Adapted by Geeky Medics. Ankit Jain, MBBS, corresponding author Anuradha Patel, MD, FRCA and Ian C. Hoppe, MD. Central cyanosis. Licence: CC BY-SA.
- Adapted by Geeky Medics. James Heilman, MD. Oral candidiasis. Licence: CC BY-SA.
- Adapted by Geeky Medics. Aurora Bakalli, Tefik Bekteshi, Merita Basha, Afrim Gashi, Afërdita Bakalli and Petrit Ademaj. Pectus excavatum. Licence: CC BY-SA.
- Adapted by Geeky Medics. Jprealini. Pectus carinatum. Licence: CC BY-SA.
- Adapted by Geeky Medics. Coronation Dental Specialty Group. Lymphadenopathy. Licence: CC BY-SA.
- Adapted by Geeky Medics. James Heilman, MD. Pedal oedema. Licence: CC BY-SA.
- Adapted by Geeky Medics. Singhai A et al. Journal of Dr. NTR University of Health Sciences. Methemoglobinaemia. Licence: CC BY-SA.