- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Retinal vein occlusion (RVO) occurs when a thrombus forms in the retinal veins and obstructs the venous drainage from the retina. The central retinal vein runs through the optic nerve and is responsible for draining retinal capillaries.1,2
RVO is the second most common cause of blindness due to retinal vascular disease. Over 50% of cases occur in patients older than 65.
The overall prevalence of RVO is 0.52%.
Aetiology
Classification
RVO can be classified anatomically based on the location of the occulsion:1
- Branch retinal vein occlusion (BRVO): due to obstruction of one of the four retinal veins
- Central retinal vein occlusion (CRVO): due to obstruction of the main retinal vein, which is responsible for draining all retinal capillaries
RVO typically occurs unilaterally, however, branch RVO occurs bilaterally in 5-10% of cases.
RVO can also be classified as ischaemic or non-ischaemic.
Ischaemic changes are associated with poorer prognosis due to retinal non-perfusion, capillary closure and retinal hypoxia, which increases the risk of neovascularisation.
Pathophysiology
In CRVO, atherosclerotic thickening of the central retinal artery leads to compression of the central retinal vein at an arteriovenous crossover point in the lamina cribosa, resulting in endothelial damage, turbulent blood flow and thrombus formation.
In BRVO, arteriosclerotic changes of a branch retinal arteriole similarly compress and occlude a branched venule.
Both circumstances can lead to retinal tissue ischaemia, infarction, vessel leakage and neovascularisation.
Risk factors
The exact cause of RVO is unknown, however, there are several associated risk factors including:1,3
- Age
- Atherosclerosis: hyperlipidaemia, hypertension and diabetes
- Open-angle glaucoma
- Inflammatory causes: sarcoidosis, Lyme disease
- Hypercoagulable states: smoking, oral contraceptive pill, pregnancy, malignancy, sickle cell disease
- Myeloproliferative disorders
- Systemic vasculitis: Behcet’s disease, polyarteritis nodosa
Clinical features
History
The main symptom is sudden, painless unilateral visual loss. The onset of visual loss is more gradual than with a retinal artery occlusion.
BRVO typically presents with partial visual field defect and metamorphopsia. BRVO can also be asymptomatic if the macula is spared.
It is important to assess for relevant risk factors such as:
- Hypertension
- Diabetes
- Oral contraceptive pill
- Smoking
- Family history of vascular disease
Clinical examination
On examination of the eyes and vision, clinical features of a retinal vein occlusion may include:
- Reduced visual acuity: significantly reduced visual acuity is more suggestive of ischaemia
- Relative afferent pupillary defect (RAPD): suggestive of ischaemia
- Visual field defect
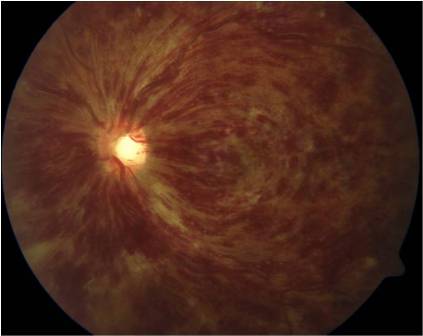
Clinical findings on ophthalmoscopy may include:
- General: dot/blot haemorrhages, vascular dilatation and tortuosity of retinal veins (distribution of these dictates BRVO or CRVO with one, or four vein territories respectively involved)
- Macular oedema: hard exudate
- Evidence of ischaemia: haemorrhages, cotton wool spots, optic disc swelling
- Neovascular complications: neovascularisation and iris rubeosis, vitreous haemorrhage
Raised intraocular pressure is suggestive of neovascular glaucoma.
In BRVO, signs are confined to the area of the retina served by the blocked vein (Figure 1).
Differential diagnoses
See the Geeky Medics guide to sudden painless loss of vision for other causes of sudden visual loss.
Investigations
Retinal vein occlusion is a clinical diagnosis, supported by ophthalmoscopy.
Bedside investigations
Relevant bedside investigations include:
- Blood pressure: hypertension is commonly associated with BRVO
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: to screen for haematological malignancy
- Glucose: to assess for diabetes
- ESR: to look for inflammatory causes
Investigations to screen for less common causes of retinal vein occlusion include:
- Liver function tests
- Thyroid function tests
- CRP
- Serum angiotensin-converting enzyme
- Serum protein electrophoresis
- Thrombophilia screen: SLE auto-antibody, antiphospholipid autoantibody
Ophthalmic imaging
Relevant ophthalmic imaging investigations include:
- Fundal photography: typically wide-field views
- Optical coherence tomography: for assessment of macula oedema
- Fundus fluorescein angiography: helps evaluate retinal capillary non-perfusion, and helps decide if ischaemic/non-ischaemic and need for laser treatment
Imaging
Other relevant imaging investigations may include:
- Chest X-ray: to exclude tumours, vasculitis (rarely required)
Management
Patients with a suspected retinal vein occlusion should be immediately referred to ophthalmology for assessment.
Systemic and general management
A diagnosis of retinal vein occlusion should be explained to the patient with appropriate information and support.
It is fundamental to identify and optimise systemic risk factors to minimise the risk of vein occlusion to the other eye (e.g. control of blood pressure and blood glucose).
Definitive ophthalmic management
There is currently no treatment to reverse the pathology associated with retinal vein occlusion.
Management focuses on treating and preventing complications to control symptoms and prevent further visual loss.
Treatment for macular oedema may include:3
- Anti-VEGF agents (ranibizumab, aflibercept or bevacizumab): may help reduce vessel leakage
- Intravitreal steroid implant (dexamethasone): may also help control oedema and blood leakage
- Macular laser therapy: less common
Treatment for neovascular complications may include pan-retinal photocoagulation (or sectoral in BRVO). This can restore some central vision by resolving macular oedema and prevent further neovascularisation
Follow-up
Ophthalmology follow-up is dependent on disease severity, but can initially be as frequent as every 4-6 weeks.7
Complications
Patients with retinal vein occlusion are at risk of macula oedema, neovascularisation and vitreous haemorrhage (may require vitrectomy and pan-retinal photocoagulation), alongside secondary glaucoma.1,3,7
Prognosis
In non-ischaemic RVO, visual acuity can restore or closely recover in about 50% of patients. Around 50–60% of untreated BRVO cases have visual acuity equal to 6/12 or worse.8
Ischaemic presentation and occlusion complications can reduce this prognosis significantly. Retinal neovascularization occurs in about 5% of cases.
Key points
- Retinal vein occlusion (RVO) refers to obstruction of retinal veins due to thrombus, resulting in retinal vascular changes.
- RVO commonly presents with sudden, painless visual loss.
- RVO is a clinical diagnosis, although other investigations may be utilised to exclude other causes.
- Fundoscopic signs may include dot-and-blot haemorrhages, cotton wool spots, macular oedema and neovascularisation.
- Prompt assessment and referral is essential to prevent further visual loss.
- Management options include laser treatment, anti-VEGF agents and intravitreal steroid use, alongside systemic risk factor control.
Reviewer
Dr Ashley Simpson
ST4 Ophthalmology
Editor
Dr Chris Jefferies
References
- Baldwin A, Goumalatsou C, Hjelde N, Myers G. Oxford Handbook of Clinical Specialities 10th Oxford: Oxford University Press; 2016.
- Rogers S et al. The prevalence of retinal vein occlusion: pooled data from population studies from the United States, Europe, Asia, and Australia. Ophthalmology 2010;117:313–319.
- Bowling B. Kanski’s Clinical Ophthalmology: A systematic approach 8th Ed; Elsevier; 2016.
- EyeWiki. BRVO. License: [CC-BY-NC]
- EyeWiki. NI CRVO. License: [CC-BY-NC]
- EyeWiki. Colour ischaemia. License: [CC-BY-NC]
- Moorfields Eye Hospital. Retinal vein occlusion. Available from: [LINK]
- Sivaprasad S, Amoaku WM, Hykin P et al. The Royal College of Ophthalmologists Guidelines on retinal vein occlusions: executive summary. Eye 2015;29:1633–1638.