- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Rheumatoid arthritis (RA) is a chronic, systemic inflammatory disease characterised by inflammation of the synovial joints, with a predilection for the small joints in the hands. It has a variety of extra-articular features.
The peak age of onset for both genders is 30-50 years and affects around 1% of people in the United Kingdom.
Aetiology
The cause of RA remains unknown but is thought to arise due to a combination of genetic (e.g. HLA genes), environmental (e.g. smoking, gut microbiome) and hormonal factors.
RA is an autoimmune disease, with circulating antibodies damaging previously healthy tissue.
These antibodies include cyclic citrullinated peptide (anti-CCP), which is highly sensitive and specific for RA, and rheumatoid factor (RF), an autoantibody targeting the Fc portion of the patient’s IgG antibody. RF lacks specificity for RA and is often seen in other diseases such as Sjogren’s syndrome.
Risk factors
Associations between genetic susceptibility and environmental factors are important risk factors for rheumatoid arthritis. Risk factors include:
- Smoking (strong association and may affect treatment response)
- Obesity
- HLA DR4 and DR1 (genes often present in patients with rheumatoid arthritis)
- Female sex (risk three times greater in pre-menopausal, suggesting oestrogen may have some influence)
Clinical features
History
RA most commonly presents with insidious joint pain, swelling and stiffness over weeks to months. Some patients may present acutely with severe joint pain and systemic features such as fever.
A small number of patients present with palindromic features associated with episodic joint pain that typically lasts 24-48 hours and then completely resolves. This may evolve into more persistent arthritis.
Typical symptoms of rheumatoid arthritis include:
- Symmetrical joint pain and swelling
- Multiple joints affected: usually small joints of hands and feet such as the proximal interphalangeal (PIP) joint, metacarpophalangeal (MCP) joint, wrist, knee, ankle, metatarsophalangeal (MTP) joint, and cervical spine
Associated systemic symptoms may include:
- Fatigue
- Low-grade fever
For more information, see the Geeky Medics OSCE guide to rheumatological history taking.
Rheumatoid arthritis vs osteoarthritis
There are important clinical features used to distinguish between inflammatory arthropathies (e.g. rheumatoid arthritis) and non-inflammatory arthropathies (e.g. osteoarthritis)
Table 1. Rheumatoid arthritis vs osteoarthritis
| Rheumatoid arthritis | Osteoarthritis | |
| Onset | Insidious | Gradual |
| Morning stiffness | >1 hour | <30 minutes |
| Worst time of the day | Morning | As day progresses |
| Effect of activity on symptoms | Lessen with activity | Worsen with activity |
| Systemic symptoms | Prominent, including fatigue | Unusual |
Clinical examination
Patients presenting with joint pain or swelling should undergo a thorough musculoskeletal examination.
The typical clinical presentation of RA is a symmetrical small joint polyarthropathy, with prominent hand and foot involvement. Other affected joints may include shoulders, knees, elbows and hips.
The spine is generally unaffected, but patients can experience cervical spine instability, which can cause atlantoaxial subluxation due to damage to the ligaments.
Rheumatoid arthritis deformities
Typical deformities associated with RA may include:
- Swan neck deformity: hyperextension of the proximal interphalangeal joint (PIP) and flexion of the distal interphalangeal joint (DIP)
- Boutonnière’s deformity: proximal interphalangeal joint (PIP) is flexed, and the distal interphalangeal joint (DIP) is hyperextended
- Z deformities of thumbs
- Ulnar deviation
- Piano key deformity of the wrist
Extra-articular manifestations
Rheumatoid arthritis can also present with systemic and extra-articular manifestations including:
- Eyes: dry eyes, scleritis, episcleritis, uveitis
- Skin: leg ulcers, rashes (pyoderma gangrenosum and cutaneous vasculitis)
- Heart: pericarditis
- Lungs (Caplan’s syndrome): pulmonary nodules, pulmonary fibrosis
- Kidneys: amyloidosis (rare)
- Rheumatoid nodules: commonly found on the extensor surface of the forearm and dorsum of the foot
- Anaemia: usually normocytic or iron deficiency related due to NSAIDs
- Liver: hepatomegaly
- Muscle wasting and tendon rupture
- Nerves: peripheral nerve entrapment, polyneuropathy
- Raynaud’s phenomenon
- Depression
Felty’s syndrome
Felty’s syndrome is a rare extra-articular manifestation of rheumatoid arthritis characterised by the triad of:
- Rheumatoid arthritis
- Splenomegaly
- Neutropenia
Differential diagnoses
Differential diagnoses will depend upon the joints affected and other associated signs and symptoms:
- Viral arthritis (e.g. parvovirus, rubella, hepatitis B)
- Reactive arthritis (secondary to gastrointestinal infection or sexually transmitted infection)
- Seronegative inflammatory arthritis (e.g. psoriatic arthritis, ankylosing spondylitis and enteropathic arthritis)
- Polyarticular gout
- Pseudogout
- Osteoarthritis
- Polymyalgia rheumatica (10% of PMR may progress to RA over time)
- Connective-tissue disease (e.g. systemic lupus erythematosus, scleroderma, Sjogren’s syndrome)
Investigations
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: normochromic, normocytic anaemia
- Inflammatory markers (ESR/CRP): usually raised but may be normal
- Liver function tests: raised ALP and GGT (acute phase reactants)
- Rheumatoid factor (RF): usually positive in 60-70% of patients but non-specific
- Anti-cyclic citrullinated peptide (anti-CCP): more specific than rheumatoid factor and more sensitive in erosive disease
- Antinuclear antibody (ANA): raised in up to 30% of cases (only check if other signs or symptoms could suggest lupus or another connective tissue disease)
- Uric acid/synovial fluid analysis: excludes polyarticular gout
- Urinalysis: microscopic haematuria/proteinuria may suggest connective tissue disease
Patients with either RF or anti-CCP antibodies are referred to as “seropositive”.
Imaging
Relevant imaging investigations include:
- X-ray (first-line radiological examination): affected joints should be imaged and may show RA-related damage such as erosions and can help differentiate from signs of osteoarthritis (e.g. joint space narrowing and subchondral sclerosis)
- Musculoskeletal ultrasound: can demonstrate joint inflammation manifest as grey scale/Doppler positive synovitis or established erosive damage
- MRI: can be useful if X-ray and ultrasound are inconclusive
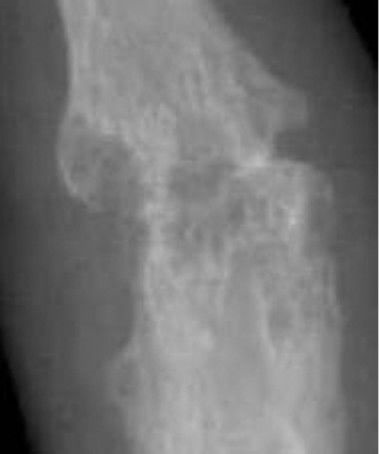
Radiological signs of rheumatoid arthritis: SPADES
SPADES is a mnemonic used to recall rheumatoid arthritis changes which may be seen on X-ray:
- Soft tissue swelling
- Peri-articular osteoporosis
- Absent osteophytes
- Deformity
- Erosions (late feature)
- Subluxation (late feature)
Diagnosis
The 2020 ACR-EULAR rheumatoid arthritis classification criteria are commonly employed to aid diagnosis, with a score of six or more required for the diagnosis of rheumatoid arthritis.
Disease monitoring
The DAS28 is an important tool for monitoring disease activity and response to treatment. The DAS28 score comprises the number of tender or swollen joints involved (total out of 28), ESR or CRP, and the patients ‘assessment of global health’ (0-100).
Management
The early diagnosis of rheumatoid arthritis and prompt treatment with disease-modifying antirheumatic drugs (DMARDs) is essential in reducing joint pain, swelling, stiffness and subsequent damage, thus potentially avoiding permanent disability.
Non-pharmacological management
NICE guidelines recommend patients with rheumatoid arthritis should be managed by a multidisciplinary team (MDT), which can include a rheumatologist, general practitioner, nurse specialist, physiotherapist, occupational therapist, dietician, podiatrist, pharmacist and social worker.
Medical management
Disease-modifying antirheumatic drugs (DMARDs)
Medical management involves one or more DMARDs, with rapid titration of doses to clinical effect. Patients need regular reviews to escalate therapy as required and monitor for side effects.
Common DMARDs include:
- Methotrexate (up to 25mg PO weekly)
- Leflunomide (10-20mg PO daily)
- Sulfasalazine (1g PO twice daily)
- Hydroxychloroquine (200-400mg daily)
All DMARDs except hydroxychloroquine require regular blood monitoring (usually in primary care as per shared care arrangements). Patients should be counselled on the side effects of DMARDs by an experienced member of the rheumatology team.
Biologic drugs
If patients do not respond to DMARDs or are intolerant, and have active disease (DAS28 score >5.1) they are eligible for biologic drugs. These may include:
- Anti-TNF (adalimumab, etanercept, certolizumab, golimumab, infliximab)
- Anti-CD20 (rituximab)
- Anti-IL6 (tocilizumab)
- CD80/86:CD28 co-stimulatory blockage (abatacept)
- JAK-inhibitors (baracitinib, tofacitinib, updacitinib)
Corticosteroids
Corticosteroids can be used at diagnosis or during a disease flare to aid rapid improvement in symptoms.
Short courses of oral prednisolone or intramuscular depo-medrone can be used. The complications of long-term steroid use should always be considered (e.g. osteoporosis, diabetes, hypertension, cataracts, gastric ulceration and weight gain). Corticosteroids should be used for the shortest period possible and at the lowest dose necessary.
Non-steroidal anti-inflammatories (NSAIDs)
NSAIDs (e.g. ibuprofen and naproxen) can also be used for analgesic benefit but do not modify the underlying disease process.
NSAIDs should be used cautiously in older patients and those with hypertension or chronic kidney disease. A proton pump inhibitor such as omeprazole is usually advisable whilst taking steroids or NSAIDs to reduce the risk of gastric ulceration and bleeding.
Surgical management
Surgical management of rheumatoid arthritis by an orthopaedic surgeon should be considered if joint symptoms such as worsening pain and function have not responded to medical management.
Complications
Complications of rheumatoid arthritis include:
- Articular deformities and functional impairment
- Depression (common)
- Vasculitis
- Pulmonary fibrosis
- Pericarditis or myocarditis
- Lymphadenopathy
- Dry eye syndrome
- Neuropathy
- Articular deformities and functional impairment
- Osteoporosis (secondary to active RA or therapies such as corticosteroids)
- Accelerated cardiovascular disease
DMARDS, corticosteroids and biological therapies may also make patients more susceptible to infection. Patients should be advised to seek advice early if they develop infective symptoms. They are advised to attend for COVID-19, influenza and pneumococcal vaccinations.
Prognostic factors
The following features are associated with a worse prognosis:
- High ESR/CRP
- Early erosions on X-rays
- High tender or swollen joint counts
- Positive anti-CCP or rheumatoid factor
Key points
- Rheumatoid arthritis is a systemic inflammatory disease, most common in the middle-aged population
- The cause is thought to be a combination of genetic, environmental and hormonal factors
- A typical clinical presentation is synovial joint inflammation involving multiple joints
- Systemic features may include fatigue, anaemia, interstitial lung disease, pericarditis, ocular disease and rashes
- Key investigations include X-rays for erosions, anti-CCP or rheumatoid factor positivity and inflammatory markers (ESR/CRP)
- Management of rheumatoid arthritis requires the early introduction of DMARDS, often in combination with short courses of steroids, before escalation to biological drugs if disease activity persists
- Complications may include functional impairment, depression and drug-induced osteoporosis.
Reviewer
Dr Stephen McDonald
Consultant Rheumatologist
Editor
Dr Chris Jefferies
References
Text references
- NICE. Rheumatoid arthritis in adults: management. Published in 2020. Available from: [LINK]
- BMJ Best Practice. Rheumatoid Arthritis. Published in 2021. Available from: [LINK]
- Cojocaru, M., Cojocaru, I.M., Silosi, I., Vrabie, C.D. and Tanasescu, R., 2010. Extra-articular manifestations in rheumatoid arthritis. Maedica, 5(4), p.286.
- Šenolt, L., Grassi, W. and Szodoray, P., 2014. Laboratory biomarkers or imaging in the diagnostics of rheumatoid arthritis?. BMC medicine, 12(1), pp.1-6.
- Radiopaedia. Rheumatoid arthritis (musculoskeletal manifestations). Published in 2022. Available from: [LINK]
- Pratt, A.G. and Isaacs, J.D., 2014. Seronegative rheumatoid arthritis: pathogenetic and therapeutic aspects. Best practice & research Clinical rheumatology, 28(4), pp.651-659.
- Kay, J. and Upchurch, K.S., 2012. ACR/EULAR 2010 rheumatoid arthritis classification criteria. Rheumatology, 51(suppl_6), pp.vi5-vi9.
Image references
- Figure 1. David Jones. Adapted by Geeky Medics. Rheumatoid arthritis. Licence: [CC BY 2.0]
- Figure 2. James Heilman, MD. Adapted by Geeky Medics. Rheumatoid arthritis chronic changes. Licence: [CC BY-SA]
- Figure 3. Phoenix119. Adapted by Geeky Medics. Swan neck deformity. Licence: [CC BY-SA]
- Figure 4. Haruko Ideguchi, Shigeru Ohno, Hideaki Hattori, Akiko Senuma and Yoshiaki Ishigatsubo. X-ray of right fourth PIP joint with bone erosions by rheumatoid arthritis. License: [CC BY]