- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This stoma examination guide provides a step-by-step approach to examining a patient’s stoma in an OSCE setting. If there are concerns about gastrointestinal pathology a full abdominal examination should also be performed alongside stoma assessment.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the examination will involve using patient-friendly language.
Gain consent to proceed with the examination.
Adequately expose the patient’s abdomen and stoma.
Position the patient lying flat on the bed.
Ask the patient if they have any pain or if they have had any problems with their stoma (e.g. bleeding, change in output) before proceeding with the clinical examination.
Stoma assessment
Begin by inspecting the stoma, noting its site, the number of lumens, the presence or absence of a spout and the contents of the effluent.
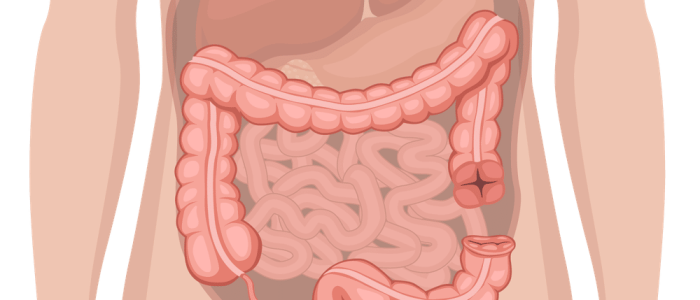
Site
Different types of stomas are typically located in specific sites on the abdomen:
- Colostomies are typically located in the left iliac fossa (LIF).
- Ileostomies and urostomies are typically located in the right iliac fossa (RIF).
Number of lumens
The number of lumens can be a helpful clue when trying to determine the type of stoma:
- 1 lumen located in the RIF: end ileostomy or urostomy
- 1 lumen located in the LIF: end colostomy
- 2 lumens close together located in the RIF: loop ileostomy
- 2 lumens close together located in the LIF: loop colostomy
Spout
The presence or absence of a spout can help to differentiate between ileostomies/urostomies and colostomies:
- Spout present: ileostomy/urostomy
- Spout absent: colostomy
A spout is used for ileostomies to prevent skin irritation from the small bowel contents produced by the stoma. A spout is used for urostomies for similar reasons.
Effluent
Effluent refers to the type of stoma output including faeces and urine. The type and form of the effluent can be useful in determining the type of stoma:
- Colostomies produce solid or semisolid faeces
- Ileostomies produce liquid or mushy small bowel content
- Urostomies produce urine
Surrounding skin
Inspect the surrounding skin for evidence of erythema, tissue breakdown or fistulation.
Stoma complications
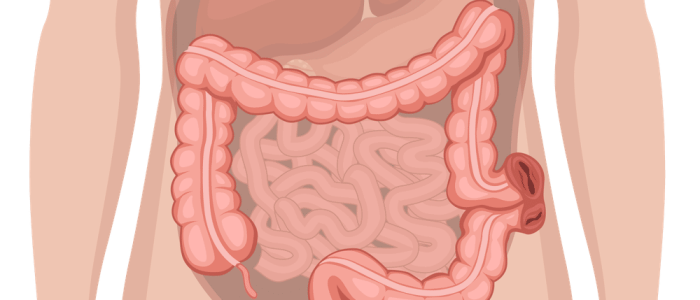
Parastomal hernia
A parastomal hernia is a type of incisional hernia in which abdominal contents protrudes through an abdominal wall defect related to the stoma. A parastomal hernia is more common with colostomies.
Clinical features of parastomal hernia can include:
- Enlargement of the stoma.
- Bulging of an area behind or around the stoma
- Increased size of the hernia when coughing or sneezing.
- A reducible parastomal mass on examination.
In rare cases, a loop of bowel can become trapped and strangulated causing ischaemic injury to the bowel.
Stoma prolapse
Stoma prolapse results in the elongation of the stoma when the patient stands, coughs or strains and reduces when the patient is lying down.
If the stoma remains prolapsed for long periods of time, venous drainage can be impaired resulting in venous congestion and secondary ischaemia.
Stoma retraction
Stoma retraction involves the stoma sinking below the level of the skin. A retracted stoma has a concave, bowl-shaped appearance. Retraction causes a poor stoma bag attachment surface, leading to leakage and frequent peristomal skin complications.
Stoma haemorrhage
A small amount of bleeding from the stomal mucosa is not uncommon and is usually the result of mild trauma during a stoma bag change. More significant or pulsatile bleeding from the stoma requires urgent medical review. Stoma bleeding may also indicate pathology within the gastrointestinal tract such as malignancy.
Stoma ischaemia/infarction
Stoma infarction develops when there is an inadequate arterial blood supply to the exteriorised bowel that forms the stoma. Causes of stoma infarction include operative tissue trauma, accidental ligation of the arterial supply to the stoma and venous outflow obstruction.
Clinical features of stoma infarction can include:
- Pain at the stoma site
- Necrosis of the stoma (appears dusky or black)
To complete the examination…
Explain to the patient that the examination is now finished.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Summarise your findings.
Example summary
“Today I examined Mrs Smith, a 64-year-old female. On general inspection, the patient appeared comfortable at rest. There were no objects or medical equipment around the bed of relevance.”
“Inspection of the abdomen revealed a single lumen stoma with a spout located in the right iliac fossa. The stoma bag contained liquid faeces and there was no evidence of parastomal skin changes or herniation.”
“In summary, these findings are consistent with a healthy end ileostomy.”
“For completeness, I would like to perform the following further assessments and investigations.”
Further assessments and investigations
- A full abdominal examination: if there are any concerns regarding gastrointestinal pathology.
References
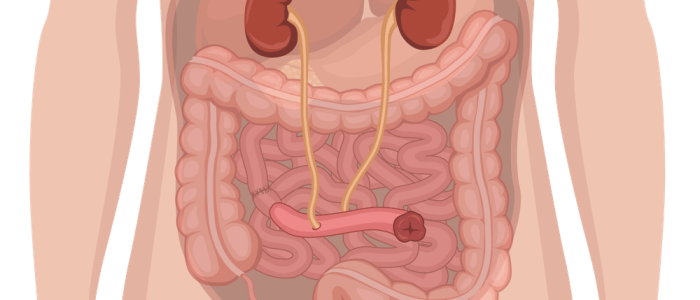
- Salicyna. Adapted by Geeky Medics. Ileostomy. Licence: CC BY-SA.
- Mikael Häggström. Adapted by Geeky Medics. Parastomal hernia. Licence: CC0.