- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Substance misuse disorder is the consumption of substances that leads to the involvement of social, psychological, physical, or legal problems.1
Among people aged 16-59, the most common use substance is cannabis, followed by cocaine and ecstasy.2 On the other hand, alcohol misuse is the fifth biggest risk factor for death across all ages. The alcohol-specific death rate for 2020 was 18.6% higher than in previous years.3
This article will cover alcohol, CNS depressants, CNS stimulants, hallucinogens, and investigations for substance misuse disorder.
Aetiology
Figure 1 shows the subtypes of substance misuse disorder, which include low-risk use, hazardous substance use, harmful substance use, and substance dependence.
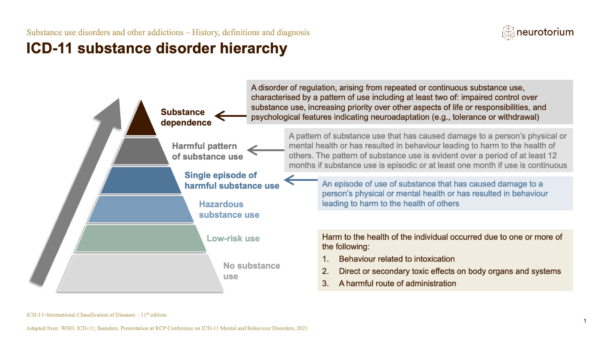
Substance dependence requires at least two of the following:
- Impaired control over substance use
- Increasing priority over other aspects of life or responsibility
- Psychological features suggestive of tolerance and withdrawal
Pathophysiology of addiction
Substance misuse affects different areas of the brain, specifically the basal ganglia, amygdala, and prefrontal cortex. It also affects the neurotransmitters such as the balance between glutamate, GABA and dopamine.
When an individual consumes a substance, this affects the mesolimbic dopamine system in the nucleus accumbens and dorsal striatum in the basal ganglia.4 The release of dopamine gives off pleasurable feelings which trigger the reward system and positively reinforce the behaviour of substance consumption. This process is known as operant conditioning and is the basis of addiction and cravings.
Some substances, such as alcohol and opioids, interact with the inhibitory neurotransmitter GABA, which disrupts the equilibrium between GABA and glutamate. It is believed that the number of natural stimulants (glutamate) and natural sedatives (GABA) are roughly the same. When an individual consumes substances, this disrupts the equilibrium as there are more sedative hormones (GABA).5
When exposed chronically, this results in neuroadaptation. The brain will upregulate the natural stimulants to achieve equilibrium. Withdrawal symptoms occur when there is a sudden drop in GABA, resulting in disrupted homeostasis and too much glutamate. The excess natural stimulants lead to withdrawal symptoms such as anxiety, sweating, and shaking.
Alcohol
According to UK guidance, the threshold for alcohol consumption is 14 units a week spread evenly over three days or more. It is important to discuss the difference between hazardous drinking, harmful drinking, and alcohol dependence.
Hazardous drinking is when an individual consumes more than 14 units of alcohol a week, which may increase their risk of harm. Harmful drinking is when the pattern of alcohol consumption directly causes physiological complications and illnesses as discussed below. Finally, alcohol dependence is characterised by craving and tolerance of alcohol consumption despite the negative complications experienced.6
Clinical features
Alcohol misuse can result in short-term harm including alcohol poisoning and accidents.
It can also affect the liver, causing liver cirrhosis and alcoholic liver disease. Individuals with chronic alcohol misuse can present with bleeding oesophageal varices, hepatic failure, and stigmata of liver diseases. Other chronic physiological consequences are discussed in the section below.
Withdrawal symptoms can be experienced after a few hours of alcohol cessation. Within 6-12 hours, patients can experience tremors, and autonomic arousal (e.g. tachycardia, fever, pupillary dilation, and increased sweating).
Between 12-48 hours of cessation, patients can experience alcohol hallucinosis (typically auditory or tactile). Between 72-96 hours, patients can present with delirium tremens. They may experience altered mental status, agitation, and tactile hallucination.
Investigations
Relevant laboratory investigations in the context of alcohol misuse include:
- Full blood count: raised MCV, raised platelets, anaemia
- Liver function tests: increased GGT, AST:ALT > 2:1
- Haematinics (B12/folate): alcohol can cause folate deficiency
- Thyroid function tests
Screening questionnaires
The AUDIT-C questionnaire is a common screening tool that looks at the risk of dependency of alcohol misuse.7
Other questionnaires include the SAD-Q questionnaire which looks at the severity of alcohol dependence and the CAGE questionnaire. For more information, see the Geeky Medics guide to alcohol history taking.
Management
The main intervention for alcohol dependence is alcohol detox. However, this method can cause serious withdrawal symptoms, leading to tremors, seizures, and delirium tremens. Therefore, alcohol detox should be carefully planned, and specialist alcohol services should be involved.
Medications can be used during the detox phase to help with the symptoms of alcohol withdrawal. Chlordiazepoxide (20-40 mg QDS) is often prescribed and monitored over the first few days. An alternative is oxazepam, used in patients with hepatic impairments and the elderly.
Naltrexone is an opiate blocker that makes alcohol less enjoyable and less rewarding. It can be administered as an injection once a month or oral tablets. Common side effects are nausea, vomiting, decreased appetite, pain at the injection site, and increased liver enzymes. It is contraindicated in opiate use and patients with liver failure.
Acamprosate is a medication that increases GABA and decreases excitatory glutamate which reduces cravings. It has a good side effect profile and is generally well tolerated.
Disulfiram inhibits acetaldehyde dehydrogenase which causes the accumulation of acetaldehyde with alcohol. It causes unpleasant symptoms such as flushing, sweating, headache, nausea and vomiting, arrhythmias, and hypotensive collapse. Patients should avoid alcohol for 24 hours before taking disulfiram and 1 week after cessation of the medication. When taking the medication, they must avoid all contact with alcohol. Disulfiram is contraindicated in patients with heart disease, psychosis, and those felt to be at high risk of suicide.
Patients should be offered psychological interventions such as cognitive behavioural therapy. In addition, it is important to prescribe prophylactic oral thiamine, if they are malnourished or in acute withdrawal, or suffer from decompensated liver disease.
Complications
Alcohol misuse can cause multiple physiological complications including:8
- Neurological: ischaemic stroke, encephalopathy, seizures, peripheral neuropathy
- Cardiovascular: increased rate of myocardial infarction and stroke, hypertension, dilated cardiomyopathy
- Hepatology: alcoholic liver disease, liver cirrhosis, liver fibrosis, pancreatitis
- Oncology: increased risk of head and neck cancer, oesophageal cancer, liver cancer, breast cancer, colorectal cancer
- Psychiatric: alcoholic hallucinosis, delirium tremens, Wernicke-Korsakoff syndrome
Wernicke-Korsakoff syndrome
Alcohol prevents the absorption of thiamine by blocking thiamine pyrophosphate synthetase, resulting in thiamine deficiency.
The main symptoms of Wernicke encephalopathy are ataxia, confusion and ophthalmoplegia.
Korsakoff syndrome involves symptoms of Wernicke encephalopathy plus short-term memory loss and hallucinations
The treatment is the intravenous replacement of thiamine (e.g. Pabrinex).
Opioid misuse
Opioid misuse includes the use of morphine, heroin, and codeine. Opioids are central nervous system depressants that slow brain activity and relax muscles.
Clinical features
Opioid misuse can cause multiple physiological and psychological effects:
- Physiological: euphoria and reduced pain, sedation, respiratory depression, miosis, constipation, skin warmth and flushing
- Psychological: apathy, disinhibition, drowsiness, impaired judgment and attention, slurred speech
When withdrawing from opioids, increased sympathetic nervous system activity causes rhinorrhoea, lacrimation, diarrhoea, pupillary dilation, piloerection, tachycardia, and hypertension.
Investigations
Relevant laboratory investigations in the context of opioid misuse include:
- HIV and hepatitis B/C: due to the increased risk of blood-borne infection is greater through needle sharing
- Tuberculosis testing
- Urea & electrolytes
- Liver function tests and clotting screen: to check hepatic function
- Drug levels: to check for drug toxicity
There are several drug screening questionnaires which can be used:9
- Drug abuse screening test (DAST): assess drug use in the past 12 months
- CAGE-AID (adapted to include drugs)
- Addiction severity index (ASI): looks at the effect of the use of substances on law, family, social life, work and mental health
- Clinical opiate withdrawal scale (COWS): rates common signs and symptoms of opiate withdrawal and monitors symptoms
Management
The main intervention for opioid misuse is opioid detox using methadone reduction. An alternative to this is buprenorphine reduction. It can be helpful to refer the patient for counselling and rehabilitation.
Complications
If taken in large doses, opioids can cause death. Of all drugs taken in overdose, opioids have been consistently shown to be the most likely to cause death. For more information, see the Geeky Medics guides to opioid overdose and the acute management of an opioid overdose.
Opioid misuse also increases the risk of blood-borne diseases such as HIV, hepatitis B, and C.
Benzodiazepines
Benzodiazepine misuse includes the use of diazepam, oxazepam and lorazepam. Benzodiazepines are another example of central nervous system depressants.
Clinical features
The clinical features of benzodiazepine misuse include:
- Physiological effects: altered mental status, slurred speech, ataxia, respiratory distress, hypothermia, and coma if overdosed
- Psychological effects: euphoria, disinhibition, apathy, aggression, anterograde amnesia, labile mood
Withdrawal from benzodiazepines may result in a wide range of clinical features including tremor, nausea & vomiting, tachycardia, postural hypotension, headache, agitation, malaise, transient illusions or hallucinations, paranoid ideation and seizures.
Investigations
The clinical institute withdrawal assessment scale – benzodiazepines (CIWA-B) can be used to determine the severity of withdrawal from the substance.
Management
The main intervention for benzodiazepine misuse is assisted withdrawal and supportive treatments.
Central nervous system stimulants
Amphetamine use (e.g. Adderall and methylphenidate) and cocaine are central nervous system (CNS) stimulants.
Clinical features
CNS stimulants activate the sympathetic nervous system which causes symptoms such as tachycardia, hypertension, and mydriasis.
Patients using cocaine may develop tactile hallucinations and chest pain.
Clinical features of CNS stimulant withdrawal include dysphoria, lethargy, psychomotor agitation, craving, increased appetite, insomnia, and bizarre dreams.
Investigations
Screening tools used for CNS stimulants are the drug abuse screening test (DAST), CAGE-AID (adapted to include drugs) and addiction severity index (ASI).
Management
There is no specific drug treatment available for CNS stimulant use. Treatment is supportive and aimed at managing withdrawal symptoms.
Hallucinogens
Hallucinogens include lysergic acid diethylamide (LSD – ‘acid’), marijuana, ecstasy and phencyclidine or phenylcyclohexyl piperidine (PCP). When consumed, they can cause euphoria, visual and auditory hallucinations and psychosis.
Clinical features
Hallucinogens mainly cause visual or auditory hallucinations and the feeling of euphoria.
Specific clinical features depend on the substance used:
- LSD: lethargy, psychomotor agitation, craving, insomnia, and unpleasant dreams
- Marijuana: increased appetite and conjunctival injection
- Ecstasy: bruxism, hyperthermia, hyponatremia, and hepatotoxicity
- PCP: loss of painful stimuli, vertical nystagmus, psychosis with hallucination, violence, and agitation
Investigations
Screening tools used for hallucinogens are the drug abuse screening test (DAST), CAGE-AID (adapted to include drugs) and addiction severity index (ASI).
Management
There are no specific interventions for hallucinogen misuse, and the mainstay treatment is supportive. This includes medically supervised detox by slowly tapering the dose, referral to a rehabilitation centre, cognitive behavioural therapy, and treatment of withdrawal symptoms.
Key points
- Substance misuse disorder is the consumption of substances that leads to the involvement of social, psychological, physical, or legal problems
- A common screening tool for alcohol misuse is the AUDIT-C questionnaire
- Opioid and benzodiazepine misuse cause sympathetic depression resulting in drowsiness, respiratory depression, and lethargy
- CNS stimulants can cause sympathetic stimulation, causing tachycardia, hypertension, and mydriasis
- Hallucinogens can cause euphoria, visual and auditory hallucinations, and psychosis
- Most treatments for substance misuse disorder are supportive and aim to reduce withdrawal symptoms
Reviewer
Dr Rana Moharam
Consultant in Child and Adolescent Psychiatry
Editor
Dr Chris Jefferies
References
- NICE. Overview: Drug use disorders in adults: Quality standards NICE. Available from: [LINK]
- Office, H. (2011) Drug misuse declared: Findings from the 2010/11 British Crime Survey, England and Wales, UK. GOV.UK. Available from: [LINK]
- John, A.B.and E. (2021) Alcohol-specific deaths in the UK: Registered in 2020, Alcohol-specific deaths in the UK – Office for National Statistics. Office for National Statistics. Available from: [LINK]
- Neurotorium. Substance use disorders and other addictions – history, definitions and diagnosis (2022). Available from: [LINK]
- U.S. Department of Health and Human Services. The Neurobiology of Substance Use, misuse, and addiction – NCBI bookshelf. Available from: [LINK]
- NICE. Alcohol problem drinking, NICE. Available from: [LINK]
- Alcohol Rehab Guide. Alcohol detox (2022). Available from: [LINK]
- U.S. Department of Health and Human Services. Alcohol’s effects on the body National Institute on Alcohol Abuse and Alcoholism. Available from: [LINK]
- SMART. Screening and assessment tools for drug and alcohol use (2015). Available from: [LINK]




