- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Temporal arteritis (also known as giant cell arteritis) is a systemic vasculitis that can affect both large and medium-sized vessels. The condition typically affects the extracranial branches of the carotid artery and is a medical emergency which requires prompt management to prevent severe complications such as permanent vision loss.1
Temporal arteritis most commonly affects women aged over 50 and is associated with polymyalgia rheumatica.
Aetiology
The aetiology of temporal arteritis is not fully understood. Different autoimmune, environmental, and genetic components have been implicated in its aetiology.
Temporal arteritis is a chronic vasculitis characterised by granulomatous inflammation of the walls of medium and large arteries. Consequently, the clinical features seen depend on which vessel is affected. The extracranial branches of the carotid artery and the ophthalmic artery are usually affected, however other branches of the aorta can also be involved.
Risk factors
The risk factors for temporal arteritis include:
- Age: patients presenting with temporal arteritis are mostly aged over 50.
- Female sex
- Polymyalgia rheumatica (PMR): approximately 50% of patients with temporal arteritis have PMR.
Clinical features
History
Temporal arteritis can present in several different ways depending on the affected vessel.3
Typical symptoms of temporal arteritis include:
- A subacute onset unilateral headache typically affecting the temporal region.
- Tongue and jaw claudication which can be caused by talking or chewing (due to ischaemia of the masseter muscle).
- Scalp tenderness: this feature is a red flag in a headache history and temporal arteritis should be actively ruled out if this symptom is present. Scalp tenderness may present as pain whilst brushing hair or when the patient rests their head on a pillow.
- Painless complete or partial loss of vision in one or both eyes
- Diplopia
Other important areas to cover in the history include:
- Systemic features: the patient may experience systemic symptoms such as malaise, fatigue, weight loss, fever, anorexia, and depression. All of which can be asked in the review of systems.
- Past medical history: it is important to ask whether the patient has polymyalgia rheumatica (PMR) as approximately 50% of patients will have features of PMR. These features include bilateral shoulder stiffness and pelvic girdle pain, with symptoms typically being worse in the morning.
Clinical examination
Typical clinical findings of temporal arteritis can include:4
- Scalp/temporal artery tenderness.
- Reduced or absent temporal artery pulse.
- Fundoscopy: oedema and pallor of the optic disc.
- Auscultation: axillary, brachial, and carotid bruits may be heard.
- Asymmetrical blood pressure.
Table 1. A summary of the history and examination findings of temporal arteritis.2
| History | Clinical examination |
| Headache: unilateral, subacute course
Tongue/jaw claudication Scalp pain/tenderness Visual symptoms: diplopia, vision loss Systemic features: malaise, weight loss, anorexia, fever, depression. |
Scalp tenderness
Reduced or absent temporal pulse Fundoscopy: pallor, oedema of the optic disc Auscultation: axillary, brachial, and carotid bruits Asymmetric blood pressure |
Investigations
Laboratory, imaging and other investigations for temporal arteritis are discussed below. 5
Laboratory
- Full blood count: normochromic normocytic anaemia and an increased platelet count may be noted.
- C-reactive protein (CRP): CRP is typically increased.
- Erythrocyte sedimentation rate (ESR): an ESR of ≥50mm/hour is considered significant. ESR levels may be lower if the patient has used glucocorticoids prior to testing.
- Liver function tests (LFTs): alkaline phosphatase and transaminases may be mildly elevated.
Imaging
- Temporal artery ultrasound: may show thickening of the wall of the affected blood vessel (known as the ‘Halo sign’).
Other investigations
- Temporal artery biopsy: will demonstrate mononuclear cell infiltration or granulomatous inflammation usually with multinucleated giant cells. Temporal artery biopsy is the definitive test for diagnosing GCA and should be performed on the symptomatic side. The biopsy result can sometimes produce a false negative due to the presence of skip lesions as a result of patchy inflammation.
Management
Temporal arteritis is a medical emergency which requires prompt management.6
Initial management
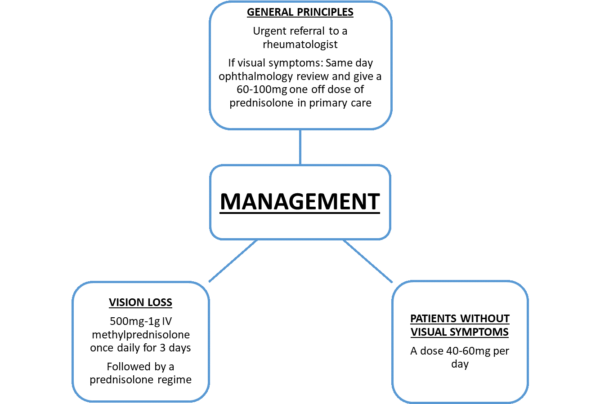
An urgent referral to a rheumatologist should be made on the same working day. If there is temporary or permanent vision loss, a same day ophthalmology review should be arranged.
The patient should be treated with oral prednisolone. NICE guidelines state for patients with visual symptoms, a one-off dose of 60mg – 100mg prednisolone should be administered in primary care prior to same day ophthalmology review. For patients without visual symptoms, a dose of 40 – 60mg of prednisolone per day should be prescribed.
For patients with visual loss, 500mg – 1g of intravenous methylprednisolone once daily is typically administered for 3 consecutive days in secondary care followed by an oral prednisolone regime.
Ongoing management
Current NICE guidelines recommend the following ongoing management of temporal arteritis:
- Gradually taper the dose of prednisolone down to zero over a period of 12-18 months.
- The patient should be monitored regularly after diagnosis. Current guidelines suggest reviewing the patient at least every 2-8 weeks for the first 6 months. In the first 2 weeks of starting prednisolone, the patient should be assessed for hypertension and hyperglycaemia.
- The side effects of prednisolone should also be mitigated. Consider starting a proton pump inhibitor (PPI) in patients who are at risk of gastrointestinal bleeding. In patients with a risk of developing osteoporosis, prophylaxis should be considered.
Complications
The complications of temporal arteritis include:3
- Irreversible vision loss
- Aortic dissections, aortic aneurysms, and large artery stenosis
- Cardiovascular events (e.g. stroke and myocardial infarction) are more common in patients with temporal arteritis.
Complications arising from steroid treatment of temporal arteritis include bruising, diabetes, hypertension, and osteoporosis.
Key points
- Temporal arteritis is a form of vasculitis affecting medium and large vessels.
- When taking a headache history, make sure to ask about scalp tenderness, temporal headache, jaw claudication and visual loss.
- Prompt management with steroids is key to preventing complications such as irreversible vision loss.
- An urgent same-day ophthalmology referral is required for patients presenting with visual loss.
Reviewer
Dr Adrian Tang
Consultant Radiologist
Editor
Dr Chris Jefferies
References
- Ahmad Al-Sukaini & Mohsin Azam, Ash Samanta. Rheumatology: A clinical handbook. Published in 2014.
- Dejaco, C., Duftner, C., Buttgereit, F., Matteson, E. and Dasgupta, B., 2016. The spectrum of giant cell arteritis and polymyalgia rheumatica: revisiting the concept of the disease. Rheumatology, p.kew273. [LINK]
- Patient.info. Giant Cell Arteritis. Last updated 2016. Available from: [LINK]
- Bongartz T. Matteson E. Large vessel involvement in Giant Cell Arteritis. Published in 2006. Available from: [LINK]
- National Institute of Health and Care Excellence CKS. Temporal arteritis Management. Last revised 2020. Available from: [LINK]
- Mackie, S.L., Dejaco, C. and Appenzeller, S. et al. 2020. British Society for Rheumatology guideline on diagnosis and treatment of giant cell arteritis. Rheumatology 59(3), e1-e23. Available from: [LINK]




