- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Temporomandibular dysfunction (TMD) refers to a range of disorders causing pain in the pre-auricular area and muscles of mastication.
It is the most common non-dental cause of orofacial pain and often associated with other chronic pain disorders.
Aetiology
Anatomy
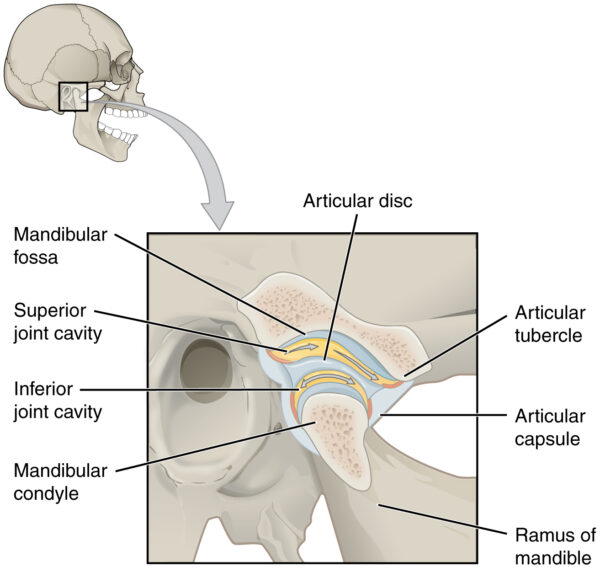
The temporomandibular joint (TMJ) connects the skull to the lower jaw. The TMJ comprises the following structures:
- Mandibular fossa of the temporal bone
- Articular disc
- Mandibular condyle
- Supporting ligaments
The superior compartment of the TMJ is responsible for the translational movement of the joint.
The inferior compartment of the TMJ is responsible for the rotational movements of the joint.
Causes of TMD
TMD involves multifactorial pathophysiology and there is no conclusive theory on the exact cause of the condition. Possible underlying causes include:
- Stress
- Low mood
- Bruxism (tooth grinding)
- Co-morbidities: including chronic pain (e.g. fibromyalgia)
- Trauma to the teeth/face causing malocclusion (an abnormal bite)
Clinical features
History
Typical symptoms of TMD include:
- Pain in the pre-auricular area which can radiate to the jaw and temporal region
- Clicking sounds: due to crepitus of the TMJ joint
- Locking: as a result of the articular disc becoming trapped preventing the jaw from closing
- Trismus: difficulties opening the mouth fully
Clinical examination
Typical clinical signs of TMD include:
- Tenderness on palpation of the TMJ
- Tenderness at the insertion point of masseter and temporalis
- Crepitus of the TMJ during jaw movement
- Trismus
- Locking of the jaw
Examining the TMJ
Begin by inspecting the mouth to look for dental pathology and to assess the patient’s occlusion (bite).
Palpate the TMJs bilaterally and then the muscles of mastication to identify any tenderness.
Ask the patient to open and close their mouth whilst palpating the joint to detect clicking as a result of joint crepitus. Deviation or locking of the jaw may also be observed at this point.
Investigations
In most cases, the diagnosis of TMD is clinical, with no further investigations required.
Relevant investigations which may be performed in a minority of cases include:
- ESR and CRP: to assess for evidence of inflammation (e.g. if considering rheumatological disease)
- X-ray: to identify gross bony pathology
- MRI: provides detailed views of the soft tissues of the TMJ (e.g. intra-articular disc)
Management
The primary goals of treatment are to eliminate pain and restore normal jaw function.
Most cases can be managed conservatively with only a small minority requiring surgical management.
Patient education is important. It is important to reassure patients that most cases of TMD are benign and will improve with conservative management. The British Association of Oral Surgeons has produced a patient information leaflet explaining TMD.
Conservative management
Conservative management of TMD includes:
- Identification of problem habits such as nail-biting and chewing gum
- Jaw exercises to strengthen muscles of mastication
- Analgesia: paracetamol and NSAIDs
- Antidepressants
- Occlusal splint: a bite guard worn over the teeth to help with malocclusion or bruxism
- Physiotherapy: improves joint function through jaw stretch and muscle relaxation
- Acupuncture: may be helpful, although evidence is inconclusive
Surgical management
Surgical management is only considered in a small number of cases when conservative measures have failed to control the patient’s symptoms.
Some examples of surgical intervention include:
- Arthrocentesis
- Arthroplasty
- TMJ replacement surgery (exceedingly rare)
Key points
- Temporomandibular dysfunction (TMD) refers to a range of disorders causing pain in the pre-auricular area and muscles of mastication.
- Typical symptoms of TMD include pain in the pre-auricular area, clicking sounds, locking of the jaw and trismus.
- Typical clinical signs of TMD include tenderness of palpation of the TMJ and muscles of mastication.
- In most cases, the diagnosis of TMD is clinical, with no further investigations required.
- The primary goals of treatment are to eliminate pain and restore normal jaw function.
- Most cases can be managed conservatively with only a small minority requiring surgical management.
- Conservative management involves patient education, identification of problem habits, jaw exercises, analgesia, antidepressants, occlusal splints and physiotherapy.
- Examples of surgical management include arthrocentesis, arthroplasty, and replacement of the TMJ.
References
- Dwonkin SF. The OPPERA study: Act One. J pain 2011; 12: T1-T3
- Durham J, Newton-John TR, Zakrzewska JM. Temporomandibular Disorders. BMJ2015;350:h4154
- Ghurye S, McMillan R. Pain-Related Temporomandibular Disorder – Current Perspectives and Evidence-Based Management. Dental Update 2015; 42 (6): 533-546
- OpenStax. TMJ. License: [CC-BY]




