- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The purpose of this article is to introduce the concept of ‘determinants’ of health and to understand how different aspects of life experience contribute to an individual’s expected health during their lifetime. Determinants can result in positive or negative impacts on health.
The social determinants of health are the conditions in which we are born, grow up, are educated, work, and live our lives.
Understanding the determinants of health helps us to see that individual decisions play only a small part in what makes someone healthy.
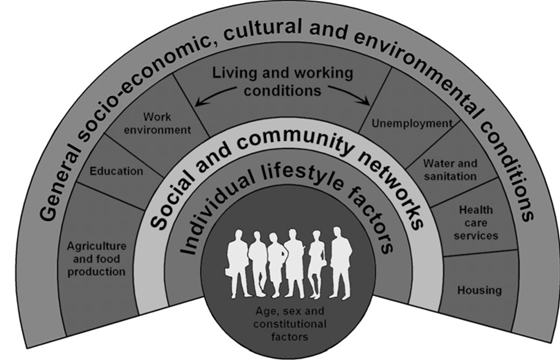
Health can be determined by factors at different levels, which is usefully illustrated by Dahlgren and Whitehead’s well-known ‘rainbow’ model, which divides determinants into layers (Figure 1).1
General socio-economic, cultural and environmental conditions
Political determinants
Particular laws passed, or political parties supported, will benefit some and disadvantage others. Individuals living in countries which are sites of political conflict are more likely to experience poor health, either directly through conflict-related injuries or mental health issues, or indirectly through lack of healthcare provision or difficulty accessing health care facilities for safety reasons.
Commercial determinants
The advertising industry plays a huge part in our health beliefs and behaviours. Adverts targeting young children with fast food or sugary beverages negatively influences their perceptions of healthy foods and can lead to obesity (with its related co-morbidities) and poor dental health, amongst other issues.
Environmental determinants
Living in an area at high risk of natural disaster, high air pollution, or extremes in climate affects the likelihood of developing diseases (e.g. asthma in areas of high air pollution), and forms barriers to accessing health care. Living in an area with a high volume of fast-food outlets, and fewer opportunities to purchase healthy foods will have a subsequent impact on diet.
Cultural determinants
Different cultures’ perceptions of health needs determine whether particular symptoms (for example, auditory hallucinations) are medicalised, or are embraced and considered to have a positive value.3
Living and working conditions
Education
Those who have higher levels of education tend to experience better health. This is through direct factors – they may be better educated about health and wellbeing and thus know when to seek help from their doctor, and indirect factors – a better education is likely to lead to a higher-paying job, which in turn is more likely to have sick pay, and support from colleagues when unwell.
Health care services
The quality of your local health care service, how accessible it is, and how affordable it is, will determine how likely you are to access health care, and how well it will meet your needs and effectively manage your condition.
Work environment
Working a high-stress job, with low autonomy or control, is linked to higher stress levels and less satisfaction at work. This has an impact on mental health, and stress-related physical health conditions, such as hypertension.4
Housing
Those living in poor quality housing are more exposed to cold and damp, with associated mental health, or respiratory conditions. Overcrowding raises the risk of infectious disease spread. Lack of housing (homelessness or rough sleeping) can be both a cause and result of poor physical or mental health.5
Social and community networks
Social networks
Weak social networks are linked to conditions such as depression, hypertension and heart disease. Those with less support are also more likely to participate in health-damaging activities, such as smoking and drinking alcohol.6 Social networks are sources of emotional and practical support.7
Community cohesion
Communities which are grounded in trust, and can exercise control over their circumstances, have better self-rated health, improved access and demand for health care and health food options, and lower rates of neighbourhood violence.8
Individual lifestyle factors
Health behaviours
Factors such as smoking, drinking, hand washing, and diet all play a part in an individual’s risk of developing disease.
Control over health decisions
The decisions that an individual chooses to make are heavily influenced by the conditions they grew up in and the opportunities they have had and play only a small factor in their health.9
Age, sex and constitutional factors
Sex or gender
A person’s sex plays a part in their health risks: women are more at risk of breast cancer, men are at risk of prostate cancer. There are also social factors to consider – women are more likely to experience domestic violence, men are less likely to report physical symptoms to their GP than women.10,11
Age
Many medical conditions are more common at an older age, such as dementia, heart disease, diabetes and cancer. Extremes of age affect an individual’s ability to independently access health care.
Ethnicity
Black and minority ethnic groups in the UK have worse health outcomes than the general population.12 There are particular conditions which are more prevalent in these communities, for example, diabetes or hypercholesterolaemia.13
However, we know that the poorer socio-economic position of some ethnic groups, inequalities of service uptake, and communication issues play a significant role in ethnic health inequalities.14
Genetics
Genetics play a part in determining the likelihood of developing certain diseases, and how long and healthily we can expect to live.15
Conclusion
Although we can use frameworks such as this to consider all the various influences on our patients’ health, the important lesson is that these factors are all interlinked.
Considering the factors that determine our patients’ health not only allows us to build a stronger, more contextually informed relationship with our patients, but also allows us to target health promotion interventions to address particular lifestyle factors or ‘determinants’ of health and disease.
Reviewer
Rebecca Pickup
ST5 Public Health
Editor
Dr Chris Jefferies
References
- Dahlgren G, Whitehead M & World Health Organization. Levelling up (part 2) : a discussion paper on European strategies for tackling social inequities in health. 2006. Available from: [LINK]
- Figure 1. The Dahlgren and Whitehead model of social determinants of health. Licence: [CC BY-NC].
- Psychiatric times. Auditory hallucinations in psychiatric illness. March 2010. Available from: [LINK]
- American psychological association. Occupational stress and employee control. November 2003. Available from: [LINK]
- Homeless link. Homelessness and health campaign. Accessed Feb 2021.
- Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health. Background document to WHO – Strategy paper for Europe. Institute for Futures Studies. September 1991. Available from: [LINK]
- Healthy People.gov. Social cohesion. Available from: [LINK]
- Healthy People.gov. Social cohesion. Available from: [LINK]
- World Health Organisation. Determinants of Health. Published in 2017. Available from: [LINK]
- Women’s aid. Domestic abuse is a gendered crime. Accessed Feb 2021. Available from: [LINK]
- Men’s health forum. Key data: understanding of health and access to services. Accessed Feb 2021. Available from: [LINK]
- Patient Professional. Ethnicity and health. December 2015. Available from: [LINK]
- Diabetes UK. Ethnicity and type 2 diabetes. Accessed Feb 2021. Available from: [LINK]
- Patient Professional. Ethnicity and health. December 2015. Available from: [LINK]
- World Health Organisation. Determinants of health. February 2017. Available from: [LINK]




