- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
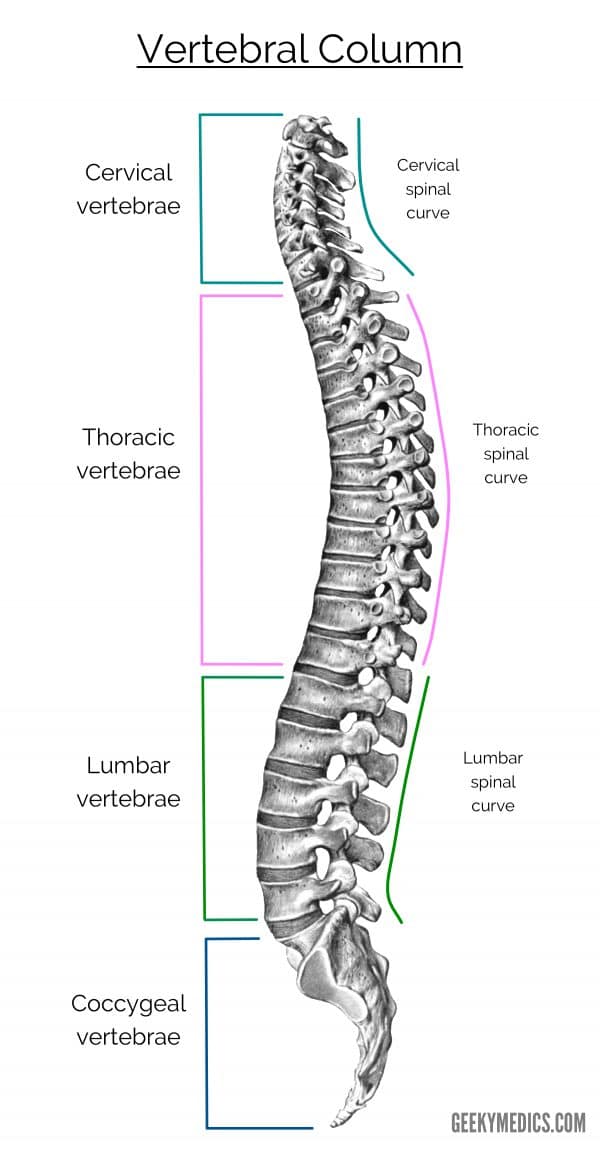
The collection of bones stacked vertically upon one another to form the spine is what we know as the vertebral column. Each of these bones is called a vertebra (plural: vertebrae).
The vertebral column comprises 33 vertebrae, each separated by fibrocartilaginous intervertebral discs.
There are five distinct regions of the vertebral column where vertebrae share distinct characteristics that allow for specific joints to form and movements to be produced. Each of these regions is assigned a letter and a number, as described below.
This article focuses on the osteology of the vertebral column.
Functions
The vertebral column is a rigid, bony structure that serves several important functions:
- Support: carrying the weight of the body above the vertebra and transmitting this through the pelvis to the legs
- Movement: forms the central axis of the body by which the trunk and legs can move
- Protection: contains the spinal canal, forming an osseous cylinder around the spinal cord
- Axis: forms an axis that structures can attach to, such as the ribs and head
Structure
There are five distinct regions of the vertebral column.
From superior to inferior, these are:
- Cervical: 7 vertebrae (C1 = highest; C7 = lowest)
- Thoracic: 12 vertebrae (T1 = highest; T12 = lowest)
- Lumbar: 5 vertebrae (L1 = highest; L5 = lowest)
- Sacral: 5 fused vertebrae (S1 = highest; S5 = lowest)
- Coccygeal: 3-4 fused vertebrae (Co1 = highest; Co3 = lowest)
Before we describe each of these regions and some examples of atypical vertebrae, we will consider the similarities in their basic structure.
Body
Almost all vertebrae in the human vertebral column contain a vertebral body. The vertebral body becomes larger and provides more stability as the vertebral column moves inferiorly from the cervical region. This is, in part, due to the increased mass placed on each vertebral body.
The vertebral body is surrounded by cortical (compact) bone. Within the cortical bone is a dense network of trabecular bone. This trabecular bone is of vital importance to haematopoiesis, or blood cell production, as it contains red bone marrow.
The vertebral bodies of two adjacent vertebrae are connected to intervertebral discs. These discs help to cushion shock as forces are transmitted through the vertebral column and contributes to improving the range of motion between vertebrae.
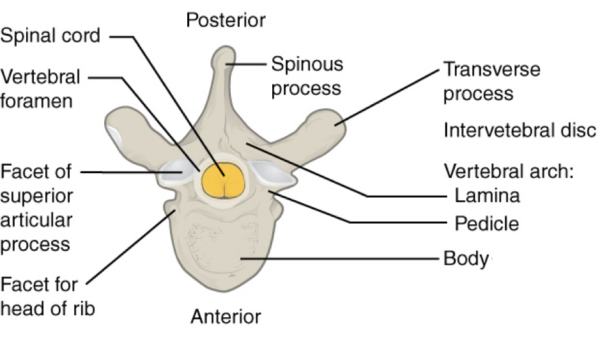
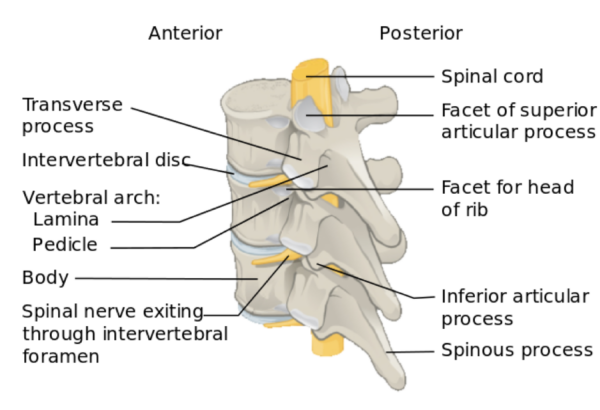
Two projections exit either side of a vertebra posteriorly: the pedicles.
Pedicles
With a name derived from the Latin pediculus, meaning “little foot,” the pedicles are two small posterior projections of the vertebral body.
They help to form the lateral margin of the spinal canal, and give rise to four important structures:
- Lamina (posteriorly)
- Articular processes (superiorly and inferiorly)
- Transverse processes (laterally)
- Lamina
The vertebral arch refers to the semicircular ring of bone that connects the two vertebral pedicles.
The vertebral arch forms the posterior margin of the spinal canal. When the lamina and pedicles are referred to collectively, they are known as the vertebral arch.
The laminae have a postero-inferior extension known as the spinous process.
Articular processes
The articular processes are small protrusions of bone extending from the junction between the pedicles and laminae. This process can extend superiorly to form the superior articular process, or inferiorly to form the inferior articular process.
At the tips of these articular processes are articular facets, which form a (zygapophyseal) joint with adjacent vertebrae to improve stability within the vertebral column.
Transverse processes
The transverse processes of the vertebral column are projections of bone that arise from the same place as the articular processes and travel laterally.
They serve different purposes in different regions of the spine, such as carrying blood vessels or forming attachment sites for the ribs.
Spinous processes
The spinous processes are postero-inferior projections of bone that exit the vertebral arch posteriorly from the midline. They assist in limiting movements in certain regions of the spine and are a site for many ligaments to attach to.
Joints
Before introducing each vertebral region, we will explore the different joints in the vertebral column. Here, we focus on the joints common to each region.
There are three major joints in each vertebra:
- Intervertebral joint (1 per vertebra)
- Superior articular joints (2 per vertebra: left and right)
- Inferior articular joints (2 per vertebra: left and right)
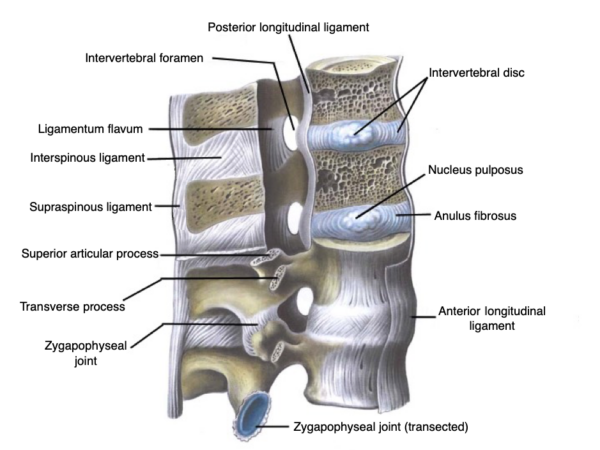
The inferior surface of a vertebral body is attached to an intervertebral disc, which then attaches to the superior surface of a vertebral body beneath it.
Intervertebral discs have two components:
- Peripheral annulus fibrosis: dense types I and II collagen providing structural integrity and osseous attachments.
- Central nuclear pulposus: high proteoglycan content to absorb water. A major shock absorber and pressure distributor. Becomes flatter proportional to time spent erect or standing.
On each vertebra, there are two superior articular processes with facets and two inferior articular processes with facets. These form the zygapophyseal, or facet, joints of the vertebral column.
The orientation of the articular facets dictates the movements allowed in each vertebral region.
For example, the thoracic spine has an anterior-posterior orientation of the facets, allowing lateral movement but limiting flexion and extension.
Ligaments
Anterior and posterior longitudinal ligaments
The anterior and posterior longitudinal ligaments form a long line, running from the cervical region to the sacrum. They attach to the anterior and posterior surfaces of the vertebral bodies, respectively. Their function is to limit excessive extension and flexion of the vertebral column, respectively
Ligamentum flavum (yellow or golden ligament)
Ligamentum flavum attaches between the laminae of each vertebra. This is very thick and strong ligament which limits excessive flexion of the vertebral column.
Interspinal ligament
This ligament runs between spinous processes of adjacent vertebrae. It limits excessive flexion of the vertebral column.
Supraspinous ligament
The supraspinous ligament runs from spinous process to spinous process, in a line down the vertebral column. It limits excessive flexion of the vertebral column.
Vertebral regions
Now that we have covered the common features of most typical vertebrae, we will discuss each vertebral region and highlight some characteristics that make bones in that region specifically identifiable. As we go, refer to these three images of the cervical, thoracic and lumbar spines to see the differences we discuss.
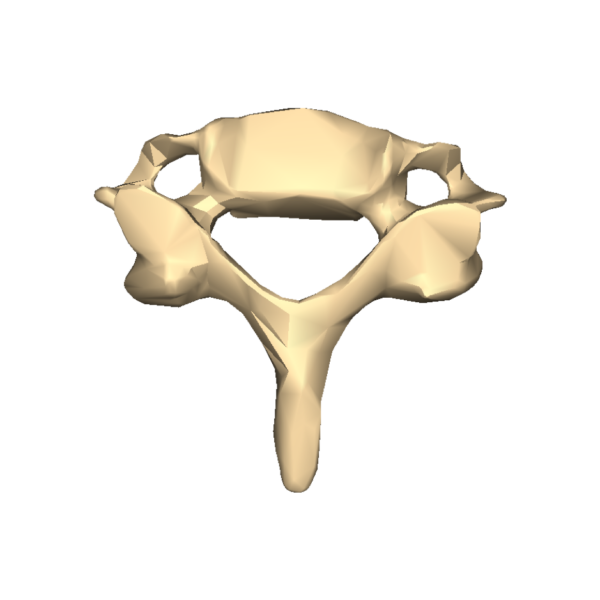
Cervical vertebrae
There are seven cervical vertebrae in the human vertebral column. They are the superior-most vertebral column group, and have several identifying features that are explained in more detail in the atypical vertebrae article:
- Small vertebral body
- Large, triangular-shaped vertebral foramen
- Transverse foramina
- Bifid spinous process
Cervical vertebrae having small vertebral bodies is the result of two important considerations:
- The mass being transmitted through the cervical vertebrae is relatively small, and does not need a large base of support
- The spinal cord is at its widest diameter in the cervical region, and a small vertebral body allows for a larger vertebral foramen
Transverse foramen in the cervical region have a distinct transverse foramina (hole). These transverse foramina allow the vertebral arteries to travel up the side of the vertebral column before entering the skull through the foramen magnum.
The vertebral arteries usually enter the transverse foramen of C6-C1, but can sometimes pass through the C7 transverse foramina as well.
Thoracic vertebrae
There are twelve thoracic vertebrae in the human vertebral column. They serve as the dorsal attachment site for the ribs, which form the majority of the lateral margin of the thoracic cavity (thorax) and line the thoracic inlet and outlet.
There are several identifying features of the typical thoracic vertebrae:
- Heart-shaped vertebral body
- Circular vertebral foramen
- Anteriorly-posteriorly facing articular facets
- Transverse processes with costal facets
- Inferiorly pointing spinous process
- Demi-facets
Each typical thoracic vertebrae has two demi-facets (half-facets) that are located on the superior and inferior lateral aspects of the thoracic vertebral body. These are positioned such that adjacent thoracic vertebrae each attach to a common rib.
Each typical rib will then attach to a single transverse process to improve the stability of the ribs and thoracic cage.
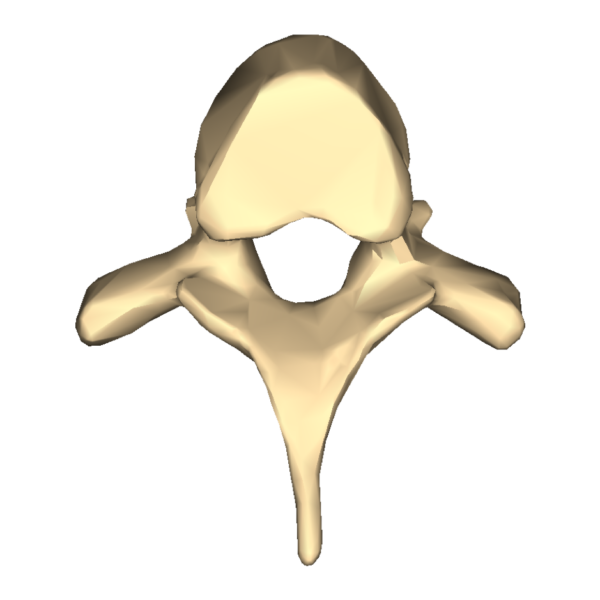
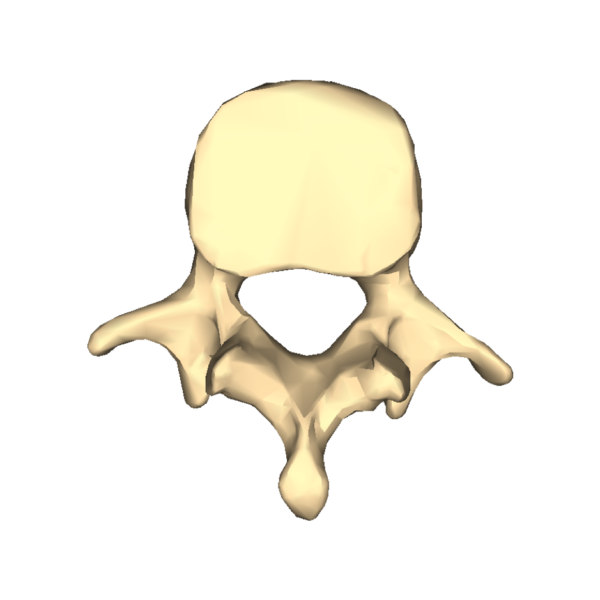
Lumbar vertebrae
The lumbar vertebrae are the last of the individual vertebrae in the vertebral column. There are five lumbar vertebrae, and each provides significant support to the body mass above the vertebral level. As a result of this, they have the largest vertebral bodies.
There are only a handful of spinal nerves left to branch from the spinal cord in the lumbar region, and the lumbar vertebrae have a small triangular vertebral foramen.
The identifying features of the lumbar vertebrae include:
- Bean-shaped, large vertebral body
- Small, triangular vertebral foramen
- Laterally-facing superior and inferior articular facets
- Short and posteriorly projecting spinous process

Figure 7. Typical lumbar vertebra.7
Sacral vertebrae
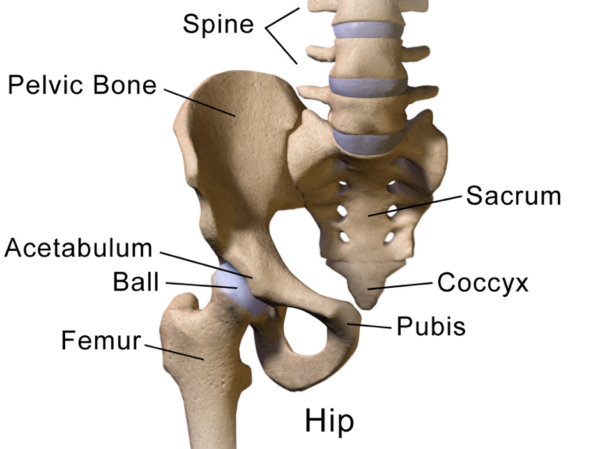
The sacrum is formed by 5 fused vertebrae that form an inverted triangle, with the base lying atop the apex.
- Superiorly the sacrum connects to the intervertebral disc of L5/S1
- Inferiorly, the sacrum connects to the coccygeal vertebrae
- Laterally, the sacrum connects to the ilium of the pelvis via several dense, strong ligaments that help form the sacroiliac joint (SIJ)
The sacral nerves travel through the sacral canal to exit via the dorsal and ventral sacral foramina.
Lumbarisation and sacralisation are two recognised anatomical variants:
- Lumbarisation refers to the separation of S1 from the rest of the sacrum
- Sacralisation refers to the fusion of L5 to the sacrum
- They are of little significance but may increase or decrease (respectively) range of motion in the lumbosacral region
Coccygeal vertebrae
The coccyx is formed by 3 (and occasionally 4) fused coccygeal vertebrae, also known as the tailbone.
Co1 and Co2 are invariably present, but Co3 can be absent or detached from the other two coccygeal vertebrae.
There are no vertebral arches in the coccygeal vertebrae, and thus, no vertebral canal can form in this region.
Clinical relevance
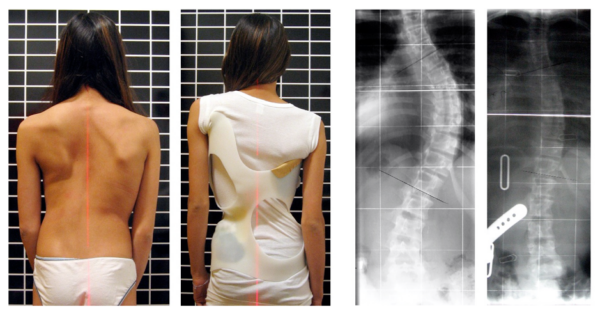
Clinical relevance – lateral curvature: scoliosis
Scoliosis refers to lateral curvature of the spine that may occur in any vertebral region, but more commonly the thoracolumbar spine.
It can be brought about by improper posture from muscular or skeletal abnormalities and may present at any age. It affects women more than men.
The signs and symptoms are location dependent, but pain is common. In thoracic scoliosis, dyspnoea and restrictive lung function patterns may be seen. In lumbar scoliosis, abdominal pain and ‘tightening’ of abdominal viscera are common.
Conservative therapy with physiotherapy, braces and exercise management can be corrective in mild disease. More advanced disease may need surgical intervention.
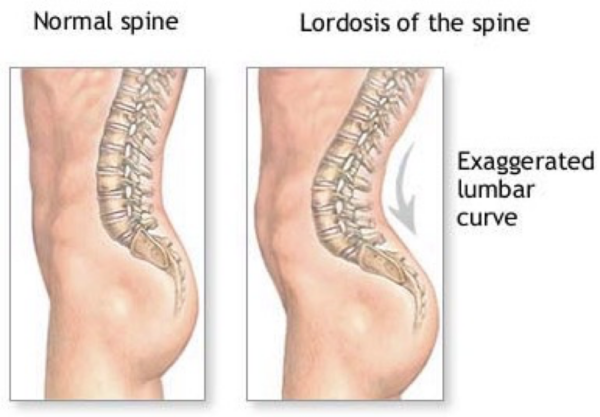
Clinical relevance – anterior/posterior curvature: kyphosis and lordosis
Kyphosis usually refers to pathological and excessive flexion of the primary spinal curves: the thoracic or the sacral curvatures.
Thoracic kyphosis presents with a heavily stooped posture and back pain. It is commonly the product of lower bone mineral density causing osteopaenic or osteoporotic crush fractures of the thoracic vertebrae.
Lordosis refers to a pathological and excessive extension of the secondary spinal curves: the cervical or lumbar curvatures.
Lumbar lordosis presents with anteriorly rotated hips and excess extension of the lumbar spine (a “hollow back”, or “Saddleback”).
Common causes of lumbar lordosis may be tight hip flexors and erector spinae muscle groups, pregnancy, and pubertal growth spurts.
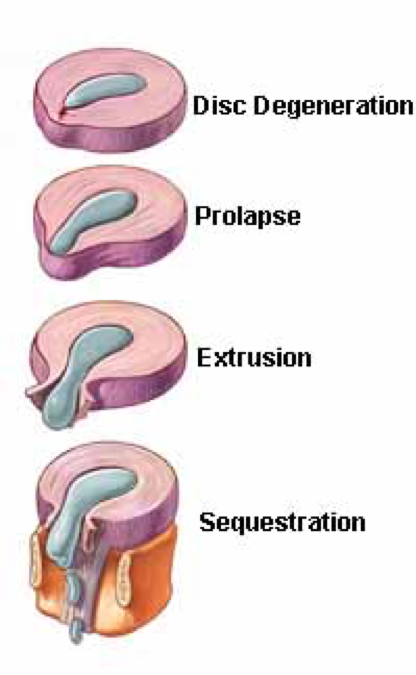
Clinical relevance – disc herniation
The intervertebral disc is the major shock absorber of the vertebral column.
The superior half of intervertebral discs send organised sheets of type I collagen fibres superiorly to attach the base of a superior vertebral body; and the inferior half of the intervertebral discs send these organised sheets inferiorly to the top of an inferior vertebral body.
Thus, a point of weakness in the intervertebral disc is this (vertically) middle portion of the disc, where there are disarrayed type I collagen fibres. The weakest portion of the intervertebral disc is the middle of the posterolateral portion, where the contents of a disc may slip through and protrude into the vertebral canal to cause spinal cord or nerve compression.
The most common locations for disc herniation are the lower cervical regions and lower lumbar regions. In both regions, the primary complaint is a shooting or radiating pain on movement of the spine or limb. Later in the disease course, motor dysfunction can occur.
To assess for disc herniation in the lumbar region, the supine leg raise test is completed. Reproducing symptoms in the first 30 degrees of hip flexion is a positive sign, and suggests the need for further workup for lumbar disc herniation.
There are several stages of disc herniation, in order:
- Disc degeneration: The nucleus pulposus bulges mildly into the annulus fibrosis
- Disc prolapse: The nucleus pulposus bulges through the annulus fibrosis, which remains intact
- Disc extrusion: The nucleus pulposus ruptures through the annulus fibrosis
- Disc sequestration: The nucleus fibrosis and annulus fibrosis both rupture
Editor
William Maish
References
Reference images
- Dr Johannes Sobotta. License: [CC BY-SA]
- BodyParts3D/Anatomography. License: [CC BY-SA]
- Jmarchn. License: [CC BY-SA]
- Beatricebalciunaite. License: [CC BY-SA]
- Anatomography. License: [CC BY-SA]
- Anatomography. License: [CC BY-SA]
- Anatomography. License: [CC BY-SA]
- BruceBlaus. License: [CC BY]
- Weiss HR. License: [CC BY]
- BruceBlaus. License: [CC BY-SA]
- Gunel Malikova. License: [CC BY-SA]
- Dawson, E. G., An, H. S. Herniated Discs: Definition, Progression, and Diagnosis by Edgar G. Accessed April 27, 2019. Available from: [LINK]
Reference texts
- Moore, K. L., Dalley, A. F., & Agur, A. M. (2013). Clinically oriented anatomy. Lippincott Williams & Wilkins.
- Sinnatamby, C. S. (2011). Last’s Anatomy, International Edition: Regional and Applied. Elsevier Health Sciences.