- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Background
Tonsillitis refers to the inflammation of the tonsils in the throat. Tonsillitis may either be acute or chronic. A general practitioner (GP) typically sees around 120 people in a 2,000-patient population with an acute sore throat every year.1 Often presenting first as a sore throat to GPs, chronic tonsillitis generally has an incidence of 100 per 1,000-patient population in the UK.2 Among these patients, children and young adults, aged 5 to 24 years old, have the highest incidence, representing 50% of total cases.3 Annually, there are approximately 37,000 childhood tonsillectomy operations in the UK, costing the NHS approximately £42 million.4,5
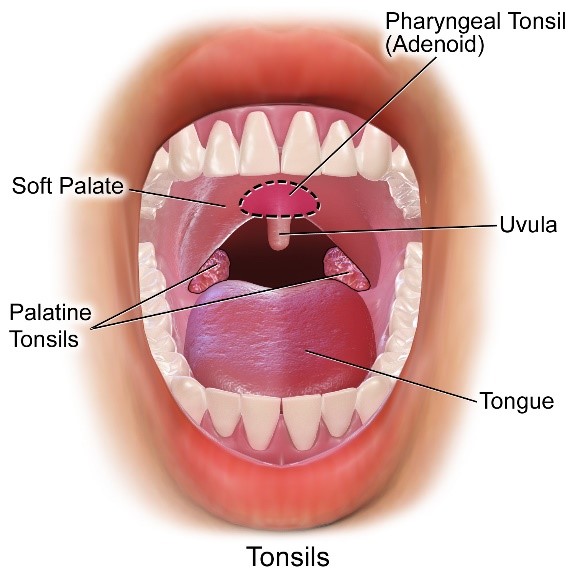
Anatomy of the oral cavity
The tonsils are part of the ring-shaped lymphoid tissue in the oropharynx, known as Waldeyer’s ring. Waldeyer’s ring consists of four main groups of tonsils: adenoid, tubal, palatine and lingual. In clinical practice, tonsillitis usually refers to the inflammation of the palatine tonsils, which are located in the lateral walls of the oropharynx.6 Irrespective of size, the palatine tonsils should be visible on examination, unlike the others.
Causes of tonsillitis
Tonsillitis may be acute or chronic (repeated acute infections). An episode of acute tonsillitis can be caused by either a viral (more common) or bacterial infection.7 There are also non-infectious causes of tonsillitis.
Common viral causes include: 8
- Rhinovirus (most common)
- Coronavirus
- Parainfluenza
- Epstein Barr Virus (EBV)
Common bacterial causes include:
- Group A beta-haemolytic Streptococcus (GABHS; most common)
- Haemophilus influenzae
- Moraxella catarrhalis
Non-infectious causes include:
- Gastro-oesophageal reflux disease
- Physical irritation (e.g. from nasogastric tubes)
Clinical features
History
Overview
Ask questions relating to symptoms outlined in CENTOR and FeverPAIN criteria (Tables 2 & 3).
Typical symptoms of tonsilitis include:
- Sore throat
- Cough
- Coryzal prodrome
- Dysphonia
- Pyrexia
- Pain and malaise
Less common symptoms include:
- Dysphagia
- Halitosis
Examination
Typical clinical findings:
- Fever
- Swollen, erythematous palatine tonsils
- Cervical lymphadenopathy
- Tonsils covered with exudate
Less common clinical findings:
- Peritonsillar abscess (usually a complication of acute tonsillitis) – unilateral bulge above tonsils, accompanied by symptoms such as a sore throat, dysphagia, trismus and a classical hot potato voice.
Differential diagnoses
The clinical presentation of tonsillitis may mimic several other conditions. The key differentiating features between these diagnoses are presented in Table 1.
Table 1. Differential diagnoses of tonsillitis, and their distinguishing features
| Differential diagnosis | Features differentiating from tonsillitis |
| Epiglottitis |
|
| Infection mononucleosis (glandular fever) due to Epstein Barr Virus |
|
| Squamous cell carcinoma |
|
Investigations
An acute episode of tonsillitis is traditionally diagnosed using clinical features alone. During this process, it is key for clinicians to identify whether tonsillitis is of viral or bacterial aetiology. This will allow for the appropriate prescription of antibiotics. This may be done with the help of the CENTOR (Table 1) and FeverPAIN criteria (Table 2).
Table 2. CENTOR criteria, indicating the likelihood of a bacterial (GABHS) tonsillitis. Scores are totalled from 0-49
| CENTOR Criteria | |
| Symptoms of tonsillitis | Points |
| Tonsillar exudate | 1 |
| Tender anterior cervical lymphadenopathy | 1 |
| History of fever (>38°C) | 1 |
| Absence of cough | 1 |
| Total points | 4 |
Note:
- A score of 0-2 has a low probability of a GABHS infection and should be managed conservatively.
- A score of 3-4 has a higher probability of a GABHS infection and should be treated with an antibiotic prescription.
Table 3. The FeverPAIN criteria consist of five symptoms of acute tonsillitis, each scoring 1 point, indicating the likelihood of a bacterial (GABHS) tonsillitis, scoring 0-5.9
| FeverPAIN criteria | |
| Symptoms of tonsillitis | Points |
| Fever (during previous 24 hours) | 1 |
| Purulence (pus on tonsils) | 1 |
| Attend rapidly (within 3 days after symptoms’ onset) | 1 |
| Severely inflamed tonsils | 1 |
| No cough or coryza (inflammation of mucous membranes in the nose) | 1 |
| Total points | 5 |
Note:
- A score of 0-1 indicates a low possibility of GABHS infection and should be managed conservatively.
- A score of 2-3 indicates a moderate possibility of GABHS infection. These patients can be either managed conservatively or given a delayed antibiotic prescription to use if symptoms do not resolve within three to five days or if they deteriorate.
- A score of 4-5 suggests a high possibility of GABHS infection and should be managed with antibiotics.
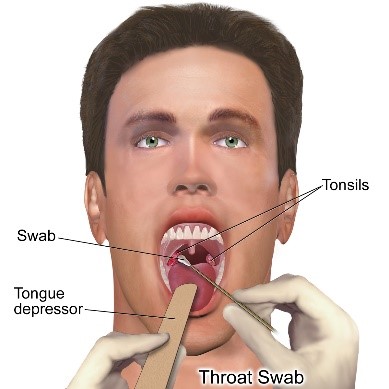
Laboratory investigations
Laboratory testing is not routinely performed as tests have no role in the diagnosis or management of tonsillitis. However, lab investigations may be useful in confirming a history of GABHS infection in patients with other conditions linked to GABHS, such as rheumatic fever and heart disease.
Examples of such investigations include:
- Throat swab for culture (to detect the presence of bacteria)
- Rapid streptococcal antigen test (to identify the presence of GABHS)
- Monospot test for EBV
Management
The overall management of tonsillitis can be broken down into acute and chronic management.
Acute management
- Supportive: hydration, fluids, ibuprofen ± paracetamol and rest
- Prescribe antibiotics (if suspected bacterial infection):
- Phenoxymethylpenicillin (Penicillin V) for 10 days.
- If allergic to penicillin, clarithromycin or erythromycin for 5 days. Consult your local BNF for appropriate doses.
- It is important to note that amoxicillin should be avoided as it can cause a generalised rash in patients who have EBV.
Chronic management
NICE advises that certain patients with recurrent episodes of tonsillitis, who meet any of the following criteria,9 can be referred for tonsillectomy (surgical removal of the tonsillar glands8):
- More than 7 documented, adequately treated, sore throat episodes in 1 year
- More than 5 episodes in 2 years
- More than 3 episodes in 3 years
- For whom there is no other explanation for recurrent symptoms
Complications
Tonsillitis
There are multiple problems that can arise if tonsillitis is not appropriately identified and treated, including:
- Otitis media (most common)
- Sinusitis
- Peritonsillar abscess (quinsy) – presents with difficulty swallowing, trismus (difficulty in opening the mouth due to spasm or pain), and airway compromise
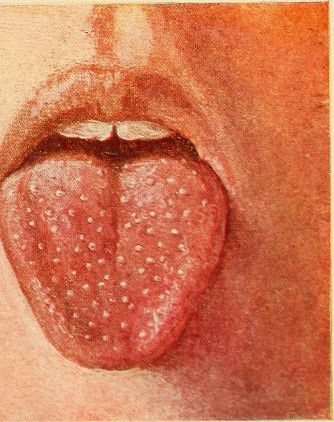
- Scarlet fever – caused by Streptococcus pyogenes (a form of GABHS), causing a rash on the chest or axillae following a sore throat and fever. Scarlet fever is traditionally known for its’ ‘strawberry tongue’ sign (Figure 3).
Tonsillectomy
Tonsillar haemorrhage is an ENT emergency, requiring immediate from an ENT surgeon and anaesthetist.
- Primary haemorrhage (within 24 hours)
- Secondary haemorrhage (after 24 hours, usually 5-10 days post-operatively) – due to infection of the tonsillar fossa
Key points
- Tonsillitis refers to inflammation of the tonsillar glands, mainly the palatine tonsils.
- It is usually caused by a viral infection.
- Clinically, the CENTOR and FeverPAIN criteria can be used by clinicians to distinguish between a viral and bacterial source of infection.
- Most common reported symptoms include sore throat, cough and a coryzal prodrome.
- Most common examination findings include fever, swollen, erythematous palatine tonsils, cervical lymphadenopathy and tonsillar exudate.
- Medical management includes pain relief if viral, and phenoxymethylpenicillin (Penicillin V) if bacterial (depending on patient allergies).
- Complications of tonsillitis include otitis media, peritonsillar abscess and scarlet fever.
References
- MeReC Bulletin. Managing sore throats. Published in 1999. Available from: [LINK]
- Georgalas C.C., Tolley, N.S. and Narula, P.A. Tonsillitis. Published in 2014. Available from: [LINK]
- Caserta, M.T. and Flores, A.R. Mandell, Douglas and Bennett’s principles and practice of infectious diseases. Published in 2010. Available from: [LINK]
- Baugh RF, Archer SM, Mitchell RB, et al. Clinical practice guideline: tonsillectomy in children. Published in 2011. Available from: [LINK]
- NHS England, Monitor. 2016/17 National tariff payment system – Annex A: 2016/17 national prices and national tariff workbook. Published in 2016. Available from: [LINK]
- Color Atlas of Oral and Maxillofacial Diseases – Bacterial Infections. Published in 2019. Available from: [LINK]
- New England Journal of Medicine (NEJM) Acute pharyngitis. Published in 2001. Available from: [LINK]
- Oxford Handbook of Clinical Specialties 10th Ear, Nose and Throat. Published in 2016. Available from: [LINK]
- National Institute for Health and Care Excellence (NICE). Sore throat – acute. Published in 2018. Available from: [LINK]
- British Medical Journal (BMJ) Best Practice. Tonsillitis. Published in 2019. Available from: [LINK]
- Bruce Blaus. Tonsils&Adenoids. Licence: [CC BY-SA]. Available from: [LINK]
- Bruce Blaus. Throat Culture. Licence: [CC BY-SA]. Available from: [LINK]
- Lewis Fischer. Diseases of Infancy and Childhood. Licence: [CC BY-SA]. Available from: [LINK]
Reviewer
Miss Shadaba Ahmed
Consultant ENT Surgeon