- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Tricyclic antidepressants (TCAs) are a class of medications developed initially for severe depression. However, the development of newer antidepressants means TCAs are now rarely used in psychiatric conditions.
Despite this, TCAs remain a commonly prescribed medication in the community and are used to manage neuropathic pain and for migraine prophylaxis. Examples of TCAs include amitriptyline, nortriptyline and dosulepin.
TCAs are a common substance ingested in self-poisoning and are highly toxic in overdose. They are second only to analgesic drugs as the most commonly taken in fatal overdose.1 An estimated 268 people die in the United Kingdom each year following tricyclic antidepressant overdose.
Aetiology
Pharmacology
TCAs act on multiple neurotransmitter pathways to enhance the effects of certain hormones while inhibiting others.
There are two main mechanisms of action:
- Reuptake inhibition: this prevents the neurotransmitter from being transported back into the pre-synaptic neurone once released into the synaptic cleft. Subsequently, the neurotransmitter remains in the synaptic cleft and continues to activate the postsynaptic receptor, increasing its effect.
- Postsynaptic receptor antagonism: this prevents the neurotransmitter from activating the postsynaptic receptor, overall reducing its effect.
Table 1. An overview of the pathways affected by TCAs.2
| Reuptake inhibition (increased effect) | Postsynaptic receptor antagonism (decreased effect) |
|
|
The key mechanism by which TCAs achieve their antidepressant effect is by inhibiting the reuptake of serotonin and noradrenaline. However, the lack of specificity and effects on other pathways results in an extensive side effect profile and contributes to their toxicity in overdose.
The clinical manifestations of pathways involved are listed below:2
- Serotonin: nausea, gastrointestinal upset, sexual dysfunction
- Noradrenaline: tachycardia, tremors
- Antihistamine: sedation, weight gain
- Anticholinergic: dry mouth, blurred vision, confusion, constipation, tachycardia, urinary retention
- Alpha-1 adrenergic: postural hypotension, drowsiness, dizziness
TCAs also act on the fast sodium channels in myocardial cells, resulting in sodium channel blockade and risk of cardiac arrhythmias, convulsions, and coma in overdose.
Risk factors
Intentional overdose
Most commonly, TCA overdose results from a suicide attempt or an act of self-harm. The patient may have a past psychiatric history or have a history of previous overdoses.
Unintentional or accidental overdose
Unintentional/accidental overdose is less common in patients presenting with a TCA overdose as they are not available over the counter.
However, there is a risk in the elderly population that those with cognitive impairment take more than their prescribed doses of medication. Likewise, a child may ingest medication that is left unattended.
Clinical features
History
TCAs are highly toxic in overdose, the most severe effects being cardiovascular and neurological instability. They have a narrow therapeutic window, with toxicity seen even with lower doses.
The clinical presentation can vary depending on severity. The clinical manifestations of overdose become apparent within six hours of ingestion.1
The key clinical features of TCA overdose include signs of anticholinergic toxicity and the result of sodium channel blockade. Severe effects include arrhythmia, cardiovascular collapse, convulsions and coma.
Typical symptoms may include:
- Dry mouth
- Hot, dry skin
- Confusion and hallucinations
- Palpitations
Other important areas to cover in the history include:
- History of ingestion: ascertain how much of the medication has been ingested. A calculation of mg/kg ingestion can be helpful prognostically. Explore whether the patient may have taken a mixed overdose and manage each substance accordingly
- Past medical history
- Past psychiatric history
Collateral history is especially important if the patient has a reduced level of consciousness. Helpful information can be gained from patients’ relatives or paramedics at the scene following the overdose. Paramedics may often bring empty medication boxes to the hospital, which helps estimate ingestion.
Clinical examination
As with all acutely unwell patients, follow an ABCDE approach to the initial assessment and management.
TCA overdose has a spectrum of clinical presentations ranging from asymptomatic patients to those acutely unwell and at risk of death.
Airway
There is a risk of airway compromise in patients who present with a reduced consciousness level and/or seizures. Signs of airway compromise include snoring, secretions, and reduced respiratory rate/reduced SpO2.
Basic airway manoeuvres can help in the acute setting, but typically patients with a GCS of 8 or below require intubation to protect the airway.
Breathing
In patients presenting with severe toxicity, respiratory depression may occur resulting in reduced respiratory rate and reduced SpO2.
Circulation
TCAs cause myocardial sodium channel blockade resulting in hypotension and arrhythmia.
Tachycardia and peripheral vasodilation may occur because of serotonergic activity.
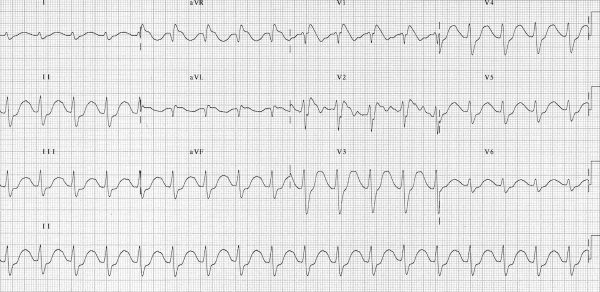
ECG findings include widened QRS and prolonged QTc. These rhythms predispose to ventricular tachycardia and ventricular fibrillation.
Disability
Assess the conscious level, either using the AVPU scale or Glasgow coma scale. Presentation of TCA overdose can range from confusion to seizures and coma.
Patients may present actively seizing or in a postictal state.
Don’t ever forget glucose, ensure all patients have bedside glucose checked to exclude hypoglycaemia.
Exposure
It is important to check temperature as patients may be hyperthermic due to serotonergic effects.
Look for anticholinergic signs including dry skin, eyes and mouth, urinary retention and ileus.
Co-ingestion with other medications which up-regulate serotonin increases the risk of serotonin syndrome.
Serotonin syndrome
Serotonin syndrome is a potentially life-threatening presentation precipitated by the overactivation of both central and peripheral serotonin receptors. It is caused by using serotonergic drugs, which include TCAs, but also other medications including SSRIs and some opioids.
The hallmark features of serotonin syndrome are altered mental state, neuromuscular hyperactivity and autonomic hyperactivity. Resultant clinical features are hypertension, tachycardia, diaphoresis, myoclonus and hyperreflexia. Severe cases result in hyperthermia and muscle rigidity.
The diagnosis of serotonin syndrome is clinical and often involves the history of ingestion of serotonergic medication. Management is largely supportive. Benzodiazepines are often used for sedation.3
Investigations
Bedside investigations
Relevant bedside investigations include:
- Basic observations (vital signs): should be checked as part of the ABCDE assessment. Findings include tachycardia, hypotension and hyperthermia.
- 12-lead ECG: TCA toxicity causes serious and potentially fatal arrhythmias. Typical ECG findings include widened QRS and prolonged QTc (Figure 1). Patients with an abnormal initial ECG are at risk of progressing to VF and VT
- Blood glucose: to exclude hypoglycaemia as a cause of presentation
- Blood gas: TCAs can cause mixed acidosis. Those with acidosis require specific treatment with bicarbonate.
Laboratory investigations
Relevant laboratory investigations include:
- Full blood count: to establish a baseline
- Urea & electrolytes: hypokalaemia is seen in TCA overdose. This can contribute to seizures or cardiac arrhythmias. TCAs are renally excreted therefore patients with renal impairment may be at risk of more serious or prolonged toxicity.
- Magnesium and bone profile: electrolyte disturbances can worsen arrhythmia and require correction
- Liver function tests: useful if there is a concern regarding co-ingestion of other medications, particularly paracetamol
- Paracetamol and salicylate levels: typically checked in all patients presenting with overdose, particularly where the history is unclear
Imaging
There is no specific imaging required for all patients presenting with TCA overdose, however, the following imaging investigations may be relevant:
- Chest X-ray: useful in the assessment of patients who are presenting with reduced conscious level and airway compromise, where there is a risk of aspiration pneumonia
- CT head: should be considered in patients with significantly reduced GCS to rule out concurrent intracranial pathology. May also be performed in those presenting with seizures.
Diagnosis
Most commonly, the diagnosis of TCA toxicity will be guided by the history of ingestion. In unresponsive patients, it is important to gain a collateral history of the substances that may have been ingested. Information regarding this can be gained from relatives, paramedics, or items on the patient (e.g. empty pill packets).
Management
Acute management
There is no specific antidote to TCAs, therefore management is supportive.
Activated charcoal can be given to the conscious patient to prevent absorption if they present within one hour of ingestion. Sodium bicarbonate can be given in arrhythmia and acidosis to prevent progression to ventricular arrhythmias.1
Resuscitation
As with the assessment of the patient, follow the ABCDE approach to the initial management of TCA overdose
Airway
Simple airway manoeuvres or adjuncts can be used initially, however, those with significantly reduced consciousness require intubation for definitive airway management
Breathing
Administer high flow oxygen and start SpO2 monitoring
Circulation
Establish intravenous access. Start continuous cardiac monitoring in all unwell patients or those with an abnormal initial ECG.
Administer fluid bolus to hypotensive patients and sodium bicarbonate if cardiac arrhythmias occur.
Disability
Assess and monitor the level of consciousness.
Benzodiazepines should be given for seizures. Phenytoin should be avoided due to its serotonergic effects.
Exposure
Cooling measures may be required to manage hyperpyrexia. Manage other specific symptoms as they develop (e.g. catheterise in urinary retention).
Capacity and Mental Health Act assessment
Patients presenting with an overdose may be confused or have a severe mental health illness resulting in an added complexity to their care. They may refuse treatment or attempt to abscond from the emergency department.
Mental capacity should be assessed during the initial review. To be deemed capacious, patients must be able to understand information, retain it, weigh up their decision and communicate their decision back to the clinician. If any of these elements of capacity are not fulfilled, then the patient lacks capacity and can be treated in their best interests.
If a patient is deemed to have capacity but remains a risk to their health, they may need to be detained under the Mental Health Act. They will need a full Mental Health Act assessment in order to be detained, which is typically performed by the hospital mental health team.
The hospital mental health team should be involved to assist in the assessment and management of patients presenting with overdose.
Ongoing management
Patients with severe toxicity need to be managed in a monitored area in the emergency department and may need intensive care unit admission for ongoing care.
Once medically stable, those who have presented with an intentional overdose require mental health assessment to manage the underlying cause of their presentation.
Complications
Ultimately, untreated TCA overdose can result in death secondary to cardiac or neurological effects. Prolonged seizure activity can result in brain injury and coma. Those with reduced consciousness are at risk of aspiration pneumonia if their airway is not managed effectively.
Key points
- TCAs are highly toxic drugs in overdose and can have serious effects even at low doses.
- Toxicity is mainly caused by anticholinergic effects and myocardial sodium channel blockade.
- The key clinical manifestations of severe toxicity are cardiovascular and neurological instability, with patients presenting with hypotension, tachycardia, convulsions and coma.
- Key investigations are ECG which may show QRS widening or QTc prolongation, and blood gas which may show acidosis.
- Management is supportive. Sodium bicarbonate can be used to manage cardiac arrhythmia and acidosis.
- Following medical management, patients require mental health assessment for ongoing care.
Reviewer
Dr Shariq Ahmed
Emergency Medicine Consultant
Editor
Dr Chris Jefferies
References
- Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Available from: [LINK].
- Westenberg HG. Pharmacology of antidepressants: selectivity or multiplicity?. Available from: [LINK]
- Volpi-Abadie, J, Kaye, AM, Kaye, AD. Serotonin Syndrome. Available from [LINK]
Image references
- Figure 1. Life in the Fast Lane. Tricyclic overdose. License: [CC BY-NC-SA]