- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Tuberculosis (TB) is a granulomatous disease caused by the Mycobacterium tuberculosis complex. TB most commonly affects the lung, but it can affect almost any organ.
After HIV/AIDs, TB is the second most common cause of death from infectious disease and is particularly prevalent in sub-Saharan Africa.1
Aetiology
The Mycobacterium tuberculosis complex includes M. tuberculosis (majority of cases), M. bovis and M. africanum.2
Infection is through droplet inhalation and therefore commonly spread by coughing and sneezing.3
After exposure to TB, the mycobacterium is engulfed by macrophages in the lung. Most people clear the infection at this point and have a spontaneous recovery. Those who do not clear it develop primary TB (Figure 1).3
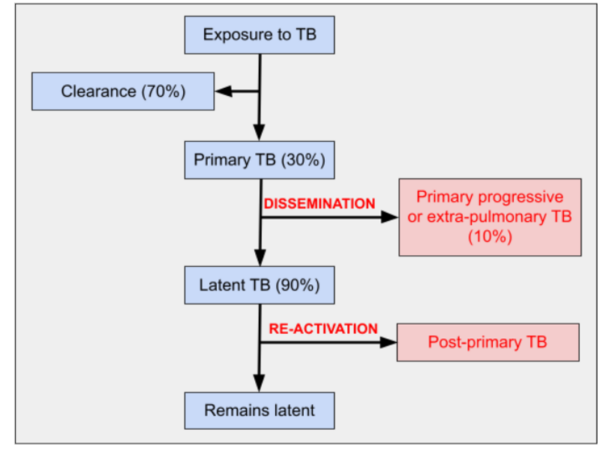
Primary TB leads to asymptomatic latent TB in most people. Latent TB can re-activate in 10%, causing post-primary TB.
A small number of people with primary TB develop primary progressive pulmonary or extra-pulmonary TB through haematogenous dissemination.3
Extra-pulmonary TB can affect almost any organ:4
- Genitourinary (sterile pyuria, pyelonephritis)
- Central nervous system (meningitis)
- Gastrointestinal system (peritonitis)
- Cardiac (pericarditis)
- Lymphatics (lymphadenitis)
- Spinal vertebrae (Pott’s disease)
Miliary TB is a disseminated form of TB commonly found in the lungs, which can develop from primary progressive or post-primary TB. The name originates from millet seeds which are said to resemble the lung nodules occurring in miliary TB.3

Risk factors
An important risk factor is close contact with a patient infected with pulmonary TB. It is important to consider exposure at school and/or work (including healthcare professionals).
Demographic features which confer increased risk of TB are ethnic minorities, those born in or travelling from high prevalence areas (India and sub-Saharan Africa), extremes of age and homelessness.1
Some medical conditions or medications can increase the risk of contracting TB or reactivation of latent TB. These include alcohol and drug dependency, immunosuppression (including HIV), malignancy, diabetes, long term steroid use and end-stage renal disease.1
Clinical features
Primary TB is often asymptomatic, and symptoms of primary progressive or post-primary TB are varied.1 A thorough history and examination are therefore vital when considering TB.
History
Typical symptoms of TB may include:1
- General: fever, lethargy, anorexia, weight loss, enlarged and tender lymph nodes
- Pulmonary: cough (usually chronic), sputum (initially dry, then purulent or blood-stained), breathlessness, pleuritic chest pain
- Extra-pulmonary: genitourinary (urinary symptoms), musculoskeletal (joint pain), neurological (headache, reduced GCS, focal neurology), cardiac (chest pain), gastrointestinal (abdominal pain, bloating), rash
Other important areas to cover in the history include:
- Past medical history: HIV or other immunosuppressive condition, chronic conditions such as diabetes
- Drug history: immunosuppressive medications including steroids
- Social history: occupation, alcohol or drug dependence, homelessness, country of birth and travel history
- TB contacts: nature and duration of contact
Clinical examination
As 60% of TB cases in the UK are pulmonary, a respiratory examination is essential when suspecting TB.1
Typical clinical findings on respiratory examination may include:
- Sputum pots with purulent or blood-stained sputum
- Enlarged, tender lymph nodes
- Crackles or bronchial breathing over consolidation
- Dullness to percussion and decreased fremitus over pleural effusions
As extra-pulmonary TB has the potential to affect almost any organ, consider performing neurological, abdominal, cardiology, musculoskeletal and skin examinations depending on features in the history.
Differential diagnoses
Important differential diagnoses to consider when suspecting pulmonary TB are:
- Bacterial pneumonia or viral respiratory tract infection
- Interstitial lung disease
- Malignancy including lymphoma
- Sarcoidosis
Investigations
Bedside investigations
Relevant bedside investigations include:
- Urine dip: sterile pyuria in genitourinary TB
- ECG: small complexes suggestive of pericardial effusion or ST-T wave changes in pericarditis6
Laboratory investigations
Relevant laboratory investigations include:1
- Basic blood tests: looking for raised inflammatory markers, renal and liver profile to guide the use of drug treatment
- Viral screen: HIV, hepatitis B and C which can increase the risk of TB
- Sputum microscopy, culture and sensitivities: three samples (a least one early morning) prior to starting antimicrobial treatment. Bronchoscopy with lavage or bronchial washings can be considered if there is no spontaneous sputum production.
- Rapid diagnostic tests for TB are used in some cases.
- Extra-pulmonary sites: early morning urine or lymph node biopsies can be cultured for TB.
- Mantoux and interferon-gamma release assay: can help to diagnose latent TB.7
Analysing samples for TB1
Samples are stained with Ziehl-Neelson (ZN) stain for acid-fast bacilli.
Samples are cultured on Löwenstein-Jensen media for 4-8 weeks. Sensitivities are complete after a further 3-4 weeks.
Imaging
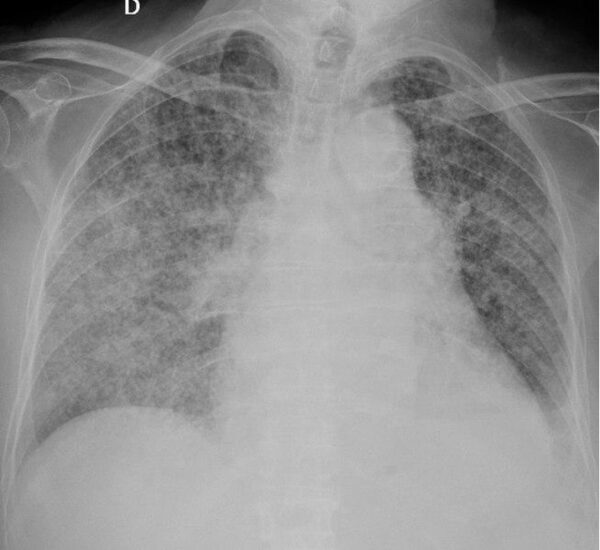
The most useful initial imaging is a chest X-ray.
Pulmonary TB can have various appearances on chest x-ray:8
- Patchy or lobar consolidation
- Linear and nodular opacities
- Miliary TB (small, uniformly distributed nodules)
- Cavitating lesions (more likely in post-primary TB)
- Tuberculoma (a caseating granuloma)
- Calcified tuberculoma (known as a Ghon focus) or lymph nodes
- Lymphadenopathy
- Pleural effusion
A CT chest can be used to further characterise pulmonary lesions or investigate for differential diagnoses.
Other investigations
Further investigations will depend on any features of extra-pulmonary TB identified from history or examination.
Investigations may include CT/MRI brain, lumbar puncture, echocardiogram, ultrasound liver or kidneys and skin biopsy.7
Management
TB is a notifiable disease under the Public Health (Infectious Diseases) Regulations 1988.1 Screening should be offered to any close contacts of a person with active TB.7
Patients with suspected TB should be managed in a single room or a negative pressure room if they are considered high risk.7
Medical management
Medical treatment for TB is delivered through several antimicrobials which are usually given daily for a prolonged period.
In exceptional circumstances, three times weekly dosing can be considered. This regimen is particularly useful if there is a risk of non-adherence, and a patient needs directly observed therapy (i.e. substance misuse, homelessness or major psychiatric disorder). In directly observed therapy, a healthcare worker administers and observes the patient taking the medication.7
The treatment for active TB without central nervous system (CNS) involvement is:
- Isoniazid, rifampicin, pyrazinamide and ethambutol for two months, followed by…
- Isoniazid and rifampicin for a further four months7
In TB with CNS involvement, treatment is similar, but isoniazid and rifampicin should be continued for ten months rather than four.7
Multi-drug resistant TB (resistant to isoniazid and rifampicin) and TB in HIV positive patients should be managed and treated with close specialist input.7
Latent TB is treated with three months of isoniazid and rifampicin or six months of isoniazid only.7
To avoid peripheral neuropathy, pyridoxine (vitamin B6) is always given with isoniazid.1
Complications
Pulmonary complications of TB include pleurisy, pleural effusions, empyema, pneumothorax, bronchiectasis and respiratory failure.
Other important complications include reduced quality of life (through prolonged treatment and stigmatisation), sepsis and death.12
In addition to complications relating to TB itself, the medical treatment of TB can have adverse effects:1
- Hepatitis: rifampicin, isoniazid and pyrazinamide
- Visual disturbance: ethambutol
- Peripheral neuropathy: isoniazid
- Drug interactions: most notably with anti-retroviral therapy used in HIV
In view of the potential complications, liver function and visual acuity should be monitored during treatment.
Key points
- Tuberculosis (TB) is a granulomatous disease most commonly caused by Mycobacterium tuberculosis. It can affect any organ, but most commonly the lungs.
- Exposure to TB can lead to primary, primary progressive, latent and post-primary TB.
- Common extra-pulmonary sites of TB include the genitourinary system, central nervous system and lymphatics.
- Aside from close contact with TB, important risk factors for TB include ethnic minorities, homelessness and immunosuppression.
- Primary TB can be asymptomatic, but pulmonary and extra-pulmonary symptoms or signs should be elicited. Risk factors from the history should also be identified.
- The most important investigations when suspecting TB are cultures (from sputum or elsewhere) and a chest X-ray. Other investigations such as a urine dip, basic blood tests, Mantoux and interferon-gamma release assay can be considered to look for extra-pulmonary or latent TB.
- The mainstay of treatment is a combination of four antimicrobials. Specialist regimes are needed in some cases.
- Complications can be due to TB (pneumothorax and bronchiectasis) or adverse effects of treatment (hepatitis, visual disturbance and peripheral neuropathy).
Reviewer
Dr Samantha Cockburn
Respiratory registrar
Editor
Dr Chris Jefferies
References
- Patient Info. Tuberculosis. Published in 2019. Available from [LINK].
- Antimicrobe. Mycobacterium Tuberculosis Complex. Published in 2010. Available from [LINK].
- E. Wang, A. Sohoni. Tuberculosis: A Primer for the Emergency Physician. Published in 2006. Available from [LINK].
- MSD Manual, Professional Version. Extrapulmonary Tuberculosis (TB). Published in 2018. Available from [LINK].
- Mikael Häggström. Extrapulmonary tuberculosis symptoms. Licence: [Public domain].
- B. Mayosi et al. Tuberculous Pericarditis. Published in 2005. Available from [LINK].
- NICE. Tuberculosis. Published in 2016. Available from [LINK].
- Radiopaedia. Tuberculosis (pulmonary manifestations). Published in 2020. Available from [LINK].
- Dr Jeremy Jones, Radiopaedia.org. Pulmonary tuberculosis. Licence: [CC BY-NC-SA 3.0].
- Benjamín Herreros, Isabel Plaza, Rebeca García, Marta Chichón, Carmen Guerrero and Emilio Pintor. Chest radiograph of miliary tuberculosis. Licence: [CC BY 4.0].
- Basem Abbas Al Ubaidi. Chest X-ray of a Ghon. Licence: [CC BY 4.0].
- NICE CKS. Tuberculosis: What are the complications? Published in 2019. Available from: [LINK].