- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Fundamental principles
The veins of the central nervous system drain deoxygenated blood from the cerebrum, cerebellum, brainstem and spinal cord. After emptying into the dural venous sinuses, most cerebral venous blood flows into the internal jugular veins before it is returned to the heart. This article discusses the venous drainage of the brain and relevant clinical conditions such as cavernous sinus thrombosis.
Drainage
Cerebrum
Veins draining the brain parenchyma may be divided into superficial and deep veins. The superficial veins primarily drain the cerebral cortex, whereas the deep veins drain the deep structures within the hemispheres. These veins do not typically follow the arterial supply and there is significant variation in anatomy between different subjects. Another notable feature of cerebral veins is that they lack muscular walls and valves.
The cerebral veins empty into the dural venous sinuses situated within the subarachnoid space. The superficial system drains into the superior sagittal sinus, while the deep system drains into transverse, straight and sigmoid sinuses.
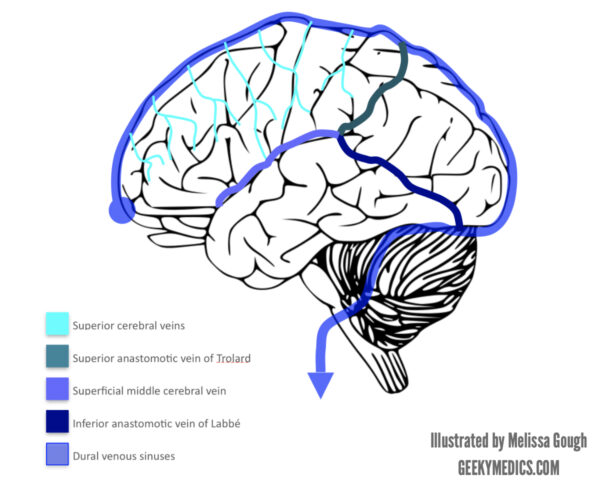
Superficial veins
The superficial venous system comprises:
- Sagittal sinuses
- Cortical veins
The cortical venous system is further divided into superior, middle and inferior groups.
There are several important superficial cerebral veins:
- Superior anastamotic vein of Trolard
- Superficial middle cerebral vein (Sylvian vein)
- Inferior anastomotic vein of Labbé
Inferior anastomotic vein of Labbé
The vein of Labbé connects the superficial middle cerebral vein with the transverse sinus. The location of this vein is extremely variable, making it vulnerable to injury during craniotomy procedures.
Superior anastomotic vein of Trolard
The superior anastomotic vein of Trolard connects the superior sagittal sinus with the superficial middle cerebral vein. It is usually the smallest of the three superficial veins mentioned in this article.
Superficial middle cerebral vein
The superficial middle cerebral vein is also known as the Sylvian vein, and it usually courses along the Sylvian fissure (lateral sulcus) picking up veins from the surrounding operculum (brain region surrounding the lateral sulcus) as it runs postero-anteriorly. The superficial middle cerebral vein then drains into the cavernous sinus after curving around the anterior temporal lobe.
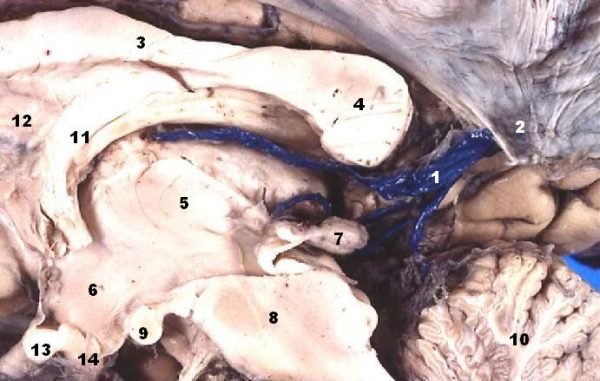
Deep veins
The deep cerebral venous drainage system comprises:
- Sinuses:
- Transverse
- Straight
- Sigmoid
- Deep cerebral veins:
- Subependymal
- Medullary
This system drains the thalamus, hypothalamus, internal capsule, septum pellucidum, choroid plexuses, corpus striatum, and the white matter.
Internal cerebral veins
This pair of veins originate at the foramen of Munro (interventricular foramen) and run posteriorly within the roof of the third ventricle. The two internal cerebral veins eventually anastomose to form the Great vein of Galen.
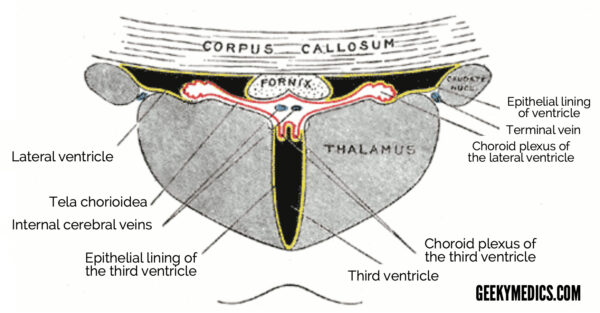
Basal veins
The two basal veins are closely related to the midbrain structures and drain into the great vein of Galen (great cerebral vein). The origin of these veins lies close to the anterior perforated substance.
Striate veins
A number of striate veins drain the caudate nucleus, thalamus, corpus striatum, and internal capsule, returning blood to the internal cerebral and basal veins. The superior striate veins empty into the internal cerebral veins, while the inferior striate veins empty into the basal veins.
Great cerebral vein
The two internal cerebral veins unite to form the great cerebral vein before it passes beneath the corpus callosum and anastomoses with the straight sinus. As well as the internal cerebral and basal veins, it receives blood from the corpus callosum itself, as well as the occipital lobes.
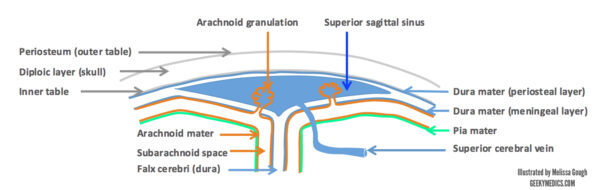
Dural venous sinuses
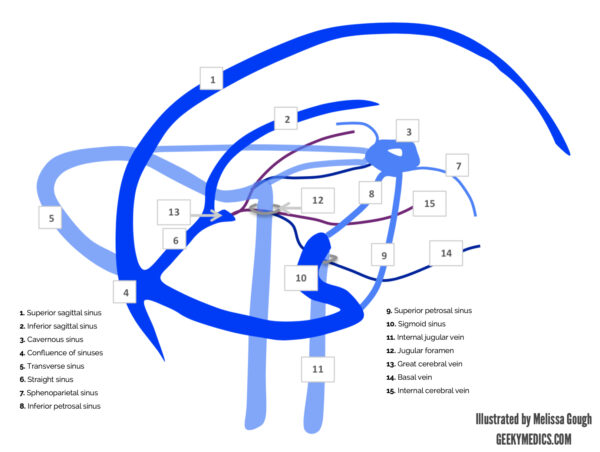
The dural venous sinus layers lie between the outer (periosteal) and inner (meningeal) layers of the dura mater (see Figure 4). Cerebral veins discussed above drain blood into the sinuses and follow a course through the dural venous sinus system eventually meeting the internal jugular veins (see Figure 5). There are no valves within the sinuses. The falx cerebri contains the superior and inferior sagittal sinuses, as well as the straight sinus. The sinuses anastomose at the confluence of sinuses at the anatomical landmark of the internal occipital protuberance.
The inferior sagittal sinus meets the great cerebral vein before continuing as the straight sinus. The transverse sinuses emerge from the confluence and go on the form the sigmoid sinuses, which drain into the internal jugular veins as they leave the cranium via the jugular foramina. The cavernous sinus is located anteriorly, and receives blood from the ophthalmic veins before emptying into the superior and inferior petrosal sinuses and subsequently the internal jugular veins.
Clinical relevance: Cavernous sinus thrombosis
Anatomically, the cavernous sinus is closely related to the highly anastomotic system of nasal sinuses, which can result in the retrograde spread of infection. The causative organism is usually Staphylococcus, Streptococcus or Haemophilus species. ¹
Common causes include: ²
- Nasal furuncle (boil) [50%]
- Sinus infection (sphenoid, ethmoid) [30%]
- Dental infections [10%]
- Trauma
Cavernous sinus thrombosis is also a rare but potentially lethal complication of orbital cellulitis. ³
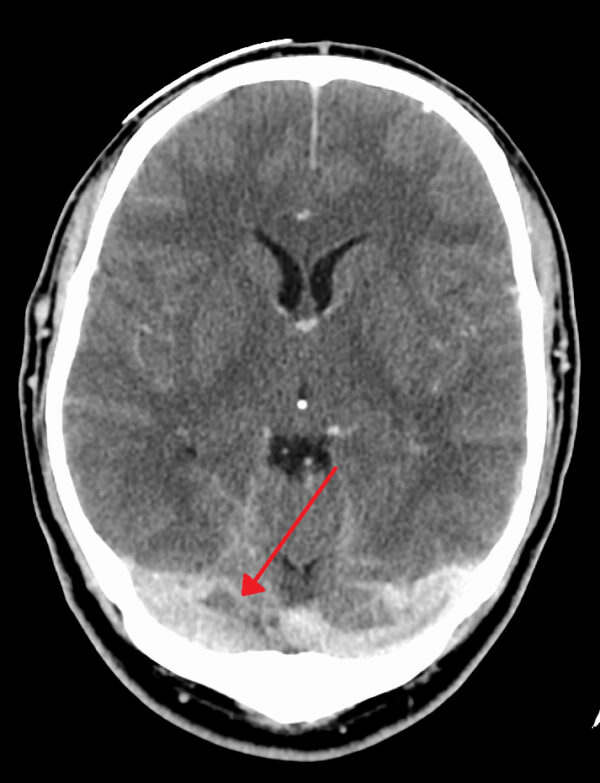
Clinical relevance: Cerebral venous thrombosis
This describes a situation wherein a clot has formed within the dural venous sinuses.
Signs and symptoms can mimic stroke presentation, and include:
- Headache (can be similar to that described in subarachnoid haemorrhage i.e. sudden blow to the head)
- Seizures, status epilepticus (common in first few days of onset) 4
- Impaired consciousness
- Focal neurological signs
- Papilloedema
- Cranial nerve palsies (if jugular vein thrombosis, affects IX, X, XI, XII)
Common causes include infection spreading from the frontal sinuses, subdural empyema (Staphylococcus aureus is the most common organism), trauma, surgery, pregnancy, and the combined oral contraceptive pill.
Recommended treatment is anticoagulation with heparin, followed by warfarin, to reach INR target 2 – 3. 5 Rarely, surgical intervention may be required to evacuate the clot.
Cerebellum
The superior and inferior cerebellar veins drain this region. The former empties into the transverse, straight, and superior petrosal sinuses, and the latter drains into the sigmoid, inferior petrosal, occipital and straight sinuses.
Brainstem
Deoxygenated blood is drained from the midbrain region as it empties into the great cerebral and basal veins. Inferiorly, veins drain blood from the pons and medulla into the superior and inferior petrosal sinuses, as well as the transverse and occipital sinuses.
Clinical relevance – measuring internal jugular venous pressure
In this article, we have discussed the major vessels draining venous blood from the brain – the IJVs.
There is a second system that assists in cerebral venous drainage. It is known as the vertebral venous plexus (VVP), and can be divided into one plexus lying inside (internal) the vertebral column, and one lying outside (external) the vertebral column.
Physiologically, the IJVs are capable of draining 100% of cerebral venous outflow, while the VVP can drain up to 30%.
The inferior petrosal sinus is a vessel that is fed by the majority of the veins in the posterior cranial fossa, such as the superficial and deep brainstem and cerebellar veins. The inferior petrosal sinus is a conduit between the IJVs and the VVP, meaning that blood from the posterior fossa can be drained by either system.
As we have discussed, we know that cerebral veins do not contain valves and are quite muscular structures. However, the IJV is an extremely thick, muscular vein – atypical when compared to other veins (it even retracts back into the skull when dissected close to the jugular foramen). This muscular wall suggests two things:
- It is under the control of the sympathetic and parasympathetic nervous systems by way of adrenergic and cholinergic smooth muscle tone; and
- It plays an important role in cerebral perfusion pressure control.
It is widely accepted that when lying supine, the IJVs remain patent, but their patency reduces upon erect sitting or standing, where it closes completely. This loss of patency is driven by the pressure exerted on the veins by the tissue surrounding them.
Thus, when sitting or standing, our IJVs are closed, and blood ‘backfills’ into the inferior petrosal sinus and posterior fossa veins while the VVP attempts to compensate for the sudden increase in venous load. Eventually, the intracranial venous pressure exceeds the perijugular tissue pressure, and the IJVs open to allow venous return toward the heart (until the tissue pressure again exceeds the venous pressure, after which the IJVs close again). This cycle continues throughout periods of erect sitting and standing. But what does this mean clinically?
When assessing the jugular venous pressure, we use the internal jugular vein as a surrogate for cardiac function at 45o for two reasons:
- It has no valves: it is a relatively good representation of what is occurring in the right heart; and
- It is normally empty: any blood ‘regurgitating’ back into the IJV is causing the IJV to open in what is normally a closed vessel, greatly exaggerating the appearance of the JVP waveform.
If it wasn’t for the dual cerebral venous outflow and having IJVs that normally remain closed in sitting and standing positions, it is likely that we wouldn’t be able to use JVP as a surrogate marker for cardiac function.
You can purchase a licence for the Complete Anatomy software we use in our videos here (we also get a percentage of your purchase fee if you use this link).
References
- Varshney S, Malhotra M, Gupta P, Gairola P, Kaur N. Cavernous sinus thrombosis of nasal origin in children. Indian J Otolaryngol Head Neck Surg 2015;67:100-5.
- https://www.msdmanuals.com/en-gb/professional/eye-disorders/orbital-diseases/cavernous-sinus-thrombosis [accessed on 14/10/2018]
- DiNubile MJ Septic thrombosis of the cavernous sinuses. Arch Neurol.1988;45567- 572
- Coutinho JM, Middeldorn S, Stam J; Advances in the treatment of cerebral venous thrombosis. Curr Treat Options Neurol. 2014 Jul16(7):299. Doi: 10.1007/s11940-014-0299-0.
- Coutinho JM, de Bruijn SF, deVeber G, et al; Anticoagulation for cerebral venous sinus thrombosis. Stroke. 2012 Apr43(4):e41-e42.
Figures and tables
- Melissa Gough, 2018
- By Henry Gray (1918), Anatomy of the Human Body, public domain via Wikimedia.org (https://commons.wikimedia.org/wiki/File:Gray723.png)
- By John A Beal, PhD Dept. of Cellular Biology & Anatomy, Louisana State University Health Sciences Center Shreveport
- Melissa Gough, 2018
- Melissa Gough, 2018
- By James Heilman, MD, Wikimedia.org (https://commons.wikimedia.org/wiki/File:Duralvenoussinusthrombosis.png)