- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Wolff-Parkinson-White (WPW) syndrome is a condition that predisposes to supraventricular tachycardia due to an accessory pathway in the heart.
Wolff-Parkinson-White syndrome presents with characteristic ECG findings, which may be associated with tachyarrhythmias and clinical symptoms of tachycardia.
The accessory pathway in Wolff-Parkinson-White syndrome is a congenital abnormality occurring in 1-3 people per 1000.1
Aetiology
In Wolff-Parkinson-White, an accessory pathway leads to stimulation of the ventricles. The accessory pathway enables electrical conduction to bypass the AV node and stimulate the proximal ventricles prematurely (pre-excitation). This, in addition to normal electrical conduction through the AV node, leads to ‘double excitation’ of the ventricles.
The location and conduction through the accessory pathway varies between individuals. In most patients, conduction can move both anterograde (from the atria to the ventricles) and retrograde (from the ventricles to the atria).
In a smaller group (approx. 15% of patients), conduction moves in a retrograde manner only. Anterograde conduction by itself is rare.
Additionally, the accessory pathway may be left-sided or right-sided. This will affect the changes seen on the ECG (see investigations section).
The accessory pathway in Wolff-Parkinson-White Syndrome is sometimes referred to as the ‘bundle of Kent’.
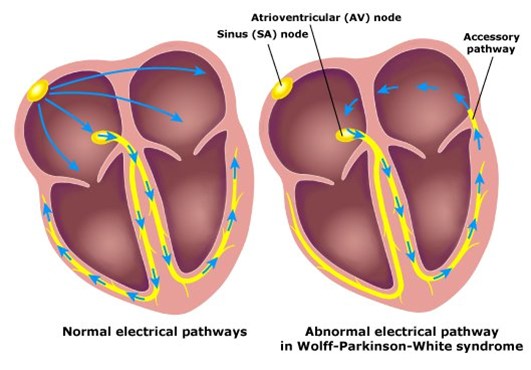
Unlike normal conduction pathways in the heart, conduction through the accessory pathway in WPW is not regulated by the AV node and can lead to tachyarrhythmias (the heart beating too fast).
Risk factors
Wolff-Parkinson-White Syndrome most commonly presents in males aged 30-40 years.2
Most WPW cases are sporadic. However, a small percentage of cases are thought to be due to an inherited mutation in the PRKAG2 gene. This genetic mutation is autosomal dominant.3
WPW Syndrome is also associated with congenital heart disease, such as Ebstein’s anomaly.
Clinical features
The clinical features of Wolff-Parkinson-White syndrome are caused by the associated tachyarrhythmias. Some patients may be asymptomatic and only diagnosed following a routine ECG.
Typical symptoms of tachyarrhythmias include:4
- Palpitations
- Feeling lightheaded
- Presyncope
- Syncope
- Cardiac arrest
Other features may include chest pain, shortness of breath and sweating.4
For more information on history taking in patients with palpitations, see the Geeky Medics OSCE guide to palpitations history taking.
The duration of these symptoms varies from person to person and can range from seconds to hours. The frequency of symptoms also varies considerably. Symptoms do not usually have any precipitating factors, however, episodes may be triggered by strenuous exercise, alcohol or caffeine.4
Differential diagnoses
The main differential diagnoses for Wolff-Parkinson White syndrome are other tachyarrhythmias:5
- Atrial fibrillation
- Atrial flutter
- Atrioventricular nodal re-entry tachycardia (AVNRT)
- Ventricular fibrillation
- Ventricular tachycardia
Other conditions that may present similarly include valvular disease, Ebstein’s anomaly (a congenital malformation of the tricuspid valve) and hypertrophic cardiomyopathy.6
Investigations
Electrocardiogram (ECG)
Key features of WPW on an ECG in sinus rhythm include:
- Short PR interval <120ms
- Delta wave: slurred upstroke of the QRS
- Widened QRS complex >110ms
- Incongruous ST segment and T waves changes
- Prominent R waves in V1-3: this mimics a posterior infarction
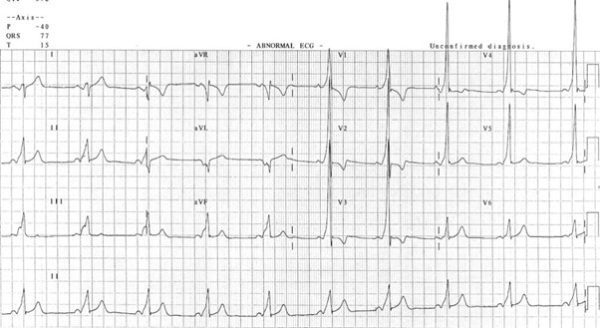
Type A vs type B
Wolff-Parkinson-White syndrome can also be subdivided depending on which side the accessory pathway runs in the heart. Type A WPW pattern is a left-sided accessory pathway and type B WPW pattern is a right-sided accessory pathway.
ECG features will be different depending on whether a person has type A or type B WPW pattern:7
- Type A (left-sided): positive delta wave in the precordial leads (V1 – V6)
- Type B (right-sided): negative delta wave in leads V1 and V2
Laboratory investigations
Blood tests may be useful in ruling out other (non-cardiac) causes of palpitations.
Relevant laboratory investigations include:
- Full blood count
- Urea and electrolytes
- Liver function tests
- Thyroid function tests
Imaging
Relevant imaging investigations include:
- Chest X-ray: to rule out other (non-cardiac) causes
- Echocardiogram: to rule out structural heart disease (e.g. Ebstein’s anomaly, hypertrophic cardiomyopathy, valvular diseases) and assess left ventricular function.
Other investigations
Other relevant investigations may include:
- Ambulatory ECG monitoring (e.g. 72-hour tape): this allows the ECG to detect periods of pre-excitation amongst normal sinus rhythm. This is often used to confirm the diagnosis of WPW syndrome.
- Exercise stress test: may help to establish the relationship between exercise and tachyarrhythmias associated with WPW
- Electrophysiology studies: may help identify accessory pathways for ablation
Management
Often, episodes of pre-excitation are short, self-terminating and do not cause problems. In people who only experience occasional symptoms, no treatment is needed, and they are followed up regularly by a cardiologist.
In patients whose episodes are triggered by stress, exercise or alcohol, simple lifestyle changes may help to reduce the frequency of tachyarrhythmia episodes.
Management of SVT
During a symptomatic episode, Wolff-Parkinson-White syndrome is treated similarly to other supraventricular tachycardias.
Vagal manoeuvres are first-line and can be used by the patient at home. An example of a vagal manoeuvre is the Valsalva manoeuvre (forced expiration against a closed glottis) which slows the heart rate via stimulation of the vagus nerve.
If vagal manoeuvres are unsuccessful, intravenous adenosine may terminate the episode by blocking conduction through the AV node.
Finally, cardioversion may be performed if adenosine is not successful.
Long-term episodes may be prevented by catheter ablation of the accessory pathway, which is effective in 95% of patients. Alternatively, daily amiodarone can slow the heart rate and prevent tachyarrhythmias.
Complications
Complications of Wolff-Parkinson-White syndrome are related to periods of tachyarrhythmia. Complications may include palpitations, dizziness, syncope and sudden cardiac death.8
Sudden cardiac death in WPW Syndrome is rare, and the overall risk is approximately 0.1% in asymptomatic patients and 0.3% in symptomatic patients per year.9
Key points
- Wolff-Parkinson-White syndrome is a congenital abnormality resulting in an abnormal accessory pathway in the heart
- This accessory pathway causes pre-excitation of the ventricles and may result in tachyarrhythmias
- The main diagnostic investigation is an ECG which has key features of a short PR interval, delta wave and broad QRS complex
- Most cases do not require active management, however, during periods of tachyarrhythmia the main management options are vagal manoeuvres or adenosine
- Complications of Wolff-Parkinson-White syndrome are related to periods of tachyarrhythmia. Sudden cardiac death is rare but more common in symptomatic patients.
Editor
Dr Chris Jefferies
References
- Lovely Chhabra; Amandeep Goyal; Michael D. Benham. Wolff-Parkinson-White Syndrome. Published 2021. Available from: [LINK]
- StatPearls. Wolff-Parkinson-White Syndrome. Published 2022. Available from: [LINK]
- Vaughan CJ, Hom Y, Okin DA, McDermott DA, Lerman BB, Basson CT. Molecular genetic analysis of PRKAG2 in sporadic Wolff-Parkinson-White syndrome. J Cardiovasc Electrophysiol. 2003 Mar;14(3):263-8. Available from: [LINK]
- Wolff-Parkinson-White Syndrome. Published August 2018. Available from: [LINK]
- Marrakchi, S. Kammoun, I. Kachboura S. Wolff-Parkinson-White Syndrome mimics a conduction disease. Case Resp Med. Published July 2014. Available from: [LINK]
- Dr C Tidy, Patient Info. Wolff-Parkinson-White Disease. Published 2020. Available from: [LINK]
- Robert Buttner, Ed Burns. Pre-Excitation Syndromes. Life in the Fast Lane. Published December 2021. Available from: [LINK]
- Wolff-Parkinson-White Syndrome Q&A. Published Jan 2017. Available from: [LINK]
- Laaouaj J, Jacques F, O’Hara G, et al. Wolff–Parkinson–White as a bystander in a patient with aborted sudden cardiac death. HeartRhythm Case Reports2016;2:399. Available from: [LINK]
Image references
- Figure 1. Tom Luck. Wolff-Parkinson-White Syndrome. License: [CC BY 3.0]. Available from: [LINK]
- Figure 2. Robert Buttner, Ed Burns. Pre-Excitation Syndromes. Life in the Fast Lane. Published December 2021. Available from: [LINK]