- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A 48 year old woman presents to the emergency department with jaundice. Work through the case to reach a diagnosis.
UK Medical Licensing Assessment (UKMLA)
This clinical case maps to the following UKMLA presentations:
- Jaundice
History
Presenting complaint
“Well, I went to my GP because over the last week or two, my skin had been getting more and more yellow. I didn’t think it was too bad, but my husband said I was very yellow, especially the whites of my eyes. I’m also getting a lot of tummy pain, which has been getting much worse!”
History of presenting complaint
When did you or your husband first notice you were yellow? “My husband said he first noticed something was wrong about 12 days ago.” Have you been unwell recently? “No, I’ve been well for a while now.” Have you noticed any other associated symptoms? “Well I’ve had some intermittent pain in my tummy and my bowels have been a bit off, but other than that I’ve been ok, no fevers or anything like that.” What’s changed with your bowels? “Well, they just seem a weird colour, pale I’d say.” Have you had any urinary symptoms? “My urine is definitely a lot darker, but other than that, no other changes.” Site – Where is this pain specifically? “Here, on my side.” (*she indicates her right hypochondrium*) Onset – When did you first start experiencing the abdominal pain? “It’s been on and off for a few months.” Character – What kind of pain is it? Is it sharp or a dull ache? “It can be quite sharp and when it’s bad it can just completely stop me in my tracks.” Radiation – Does it move anywhere else? “It used to give me some back pain behind my right shoulder, but now it’s only sore in the same place on my side.” Associated symptoms – Do you experience any other symptoms when you have the abdominal pain? “I often feel a bit nauseated when it’s happening, but that’s about it.” Timing – How frequently are you experiencing the abdominal pain? “Well when it started a few months ago, I’d get the pain every week or so, but now I’m getting at least one or two bouts of pain a day.” Exacerbating and/or relieving factors – Does anything seem to trigger the pain or make it better? “I know that if I eat a big dinner it will get more painful. I don’t eat much at all now because it makes me sore and a bit nauseous.” Severity – If you were to rate the pain out of 10, how bad would you say it is? “Right now? I’d say 7 out of 10.” Past medical and surgical history “The only times I was ever in the hospital were for the birth of my two children and for appendix surgery when I was a teenager. I never had a blood transfusion to my knowledge.” Drug history “I just take a blood pressure tablet, can’t remember the name, but I’ve taken it for years. Other than that I don’t take anything. I don’t have any allergies.” Social history “I would usually have a glass of wine each day with dinner. I’ve never smoked and haven’t ever used recreational drugs. I was on holiday last summer but it wasn’t abroad.” Family history “No, we don’t have any medical conditions that run in the family.” General assessment Abdominal examination Murphy’s sign is elicited by asking the patient to breathe out and then gently placing the hand below the costal margin on the right side at the mid-clavicular line (the approximate location of the gallbladder). The patient is then instructed to breathe in. Normally, the abdominal contents are pushed downward during inspiration as the diaphragm moves down. The test is considered positive if the patient stops breathing in and winces with a ‘catch’. The same manoeuvre must not elicit pain when performed on the left side for the test to be positive.¹Exploring the abdominal pain
Other areas of the history
Clinical examination
Abdominal examination findings
Courvoisier’s law states if a patient presents with jaundice and they have a non-tender, palpable gallbladder on examination, the cause is unlikely to be due gallstones. This is because gallstones form over a prolonged period, which results in a shrunken fibrotic gallbladder which does not distend easily. As a result, jaundice and a palpable gallbladder should raise suspicion of malignant obstruction of the biliary tree (e.g. pancreatic cancer).
Mirizzi’s syndrome is a rare complication in which a gallstone becomes impacted in the cystic duct or neck of the gallbladder causing compression of the common bile duct (CBD) or common hepatic duct, resulting in obstruction and jaundice. Obstructive jaundice can be caused by direct extrinsic compression by the stone or from fibrosis caused by chronic cholecystitis (inflammation).²
This is when a cholecystoenteric fistula forms and a gallstone passes into the small intestine and obstructs the terminal ileum.
Differential diagnoses
- Cholecystitis
- Choledocholithiasis
- Cholangitis
Investigations
- Full blood count (Hb, platelets, WCC)
- Serum lipase and amylase (to help rule out pancreatitis)
- LFTs (useful when trying to differentiate between obstructive jaundice and primary hepatic pathology)
- Coagulation screen (helpful to assess the liver’s synthetic function)
- U&Es (baseline renal function)
Results
- Hb 14 (13-18.5g/dL)
- Platelets 175 (150 – 450 x109/L)
- WCC 13 (4-11 x109/L) ↑
- Na+ 136 (135-145mmol/L)
- K+ 4.1 (3.5-5mmol/L)
- Urea 5 (3-7mmol/L)
- Creatinine 100 (62-106mmol/L)
- Albumin 44 (35-50g/L)
- PT and APTT: normal
- Bilirubin 75 (<17µmol/L) ↑
- ALT 29 (7-35 IU/L)
- AST 26 (8-48 IU/L)
- ALP 137 (45-115 IU/L) ↑
- γGT 83 (<60 IU/L) ↑
- Lipase 150 (114-286IU/L)
- Amylase 80 (25-115 IU/L)
- USS gallbladder – the gold standard in the investigation of gallstones
- Abdominal X-ray – not that useful as only 10% of gallstones are calcified are therefore visible on x-ray
- CT abdomen with contrast – can be useful if other modalities fail however some gallstones are isodense to bile and therefore may not be visible on CT scans
- MRCP – provides detailed imaging of the biliary tree – often used for pre-operative planning of surgery
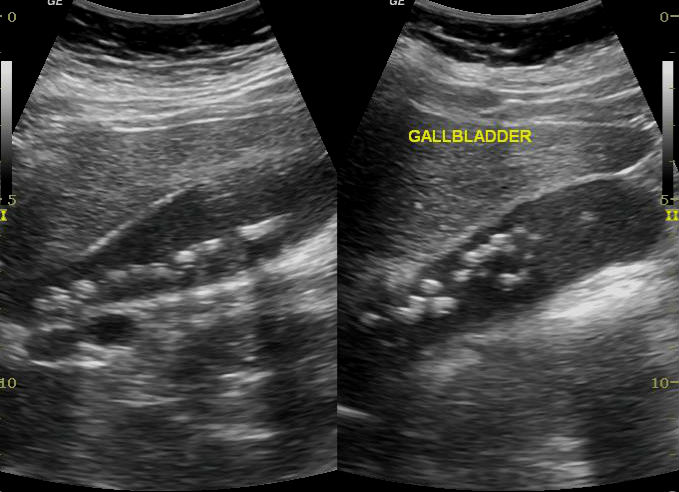
Radiology report
“Distended gallbladder containing multiple calculi. Diffuse wall oedema. CBD dilated at 8mm.”
Diagnosis
Acute cholecystitis
This patient has jaundice which is concerning for common bile duct stones or Mirizzi syndrome and should be investigated thoroughly before surgical intervention.
Management
Patients with acute cholecystitis almost always require hospital admission. They should receive antibiotics to cover any superimposed infection. Antibiotics can be given either orally or IV, depending on the patient’s clinical condition and local microbiology guidelines.
Patients should be restricted to clear oral fluids as they will likely require surgery. Although most cases of acute cholecystitis will settle with antibiotic therapy, current guidelines recommend an emergency laparoscopic cholecystectomy provided the patient is within seven days of symptom onset.
Due to infection and inflamed friable tissues, emergency cholecystectomy can be more technically challenging than elective surgery. However, it appears to be just as safe. It is also associated with shorter hospital stays and lower overall morbidity, as many patients will become unwell with further acute complications of gallstones whilst waiting for an elective operation.
References
- Bree, R. L. (1995). Further observations on the usefulness of the sonographic Murphy sign in the evaluation of suspected acute cholecystitis. Journal of clinical ultrasound, 23(3), 169-172.
- Vitale M. Mirizzi Syndrome Type IV: An Atypical Presentation That Is Difficult to Diagnose Preoperatively. 2009. Society for Surgery of the Alimentary Tract
- Greg McLatchie, Neil Borley, Joanna Chikwe (2013). Oxford Handbook Of Clinical Surgery. 4th ed. Oxford, UK: Oxford University Press. P311-321.
- Alasdair K.B. Ruthven (2010). Essential Examination. 2nd ed. Oxfordshire, UK: Scion Publishing Limited. p14-17.
- Case courtesy of Maulik S Patel, Radiopaedia.org, rID: 24354




