- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
What is clinical reasoning?
Clinical reasoning is a difficult concept to define. This is because, for the most part, it is a process that occurs inside your thoughts, making it difficult to describe and for others to observe. Learning about clinical reasoning can feel challenging, especially in the beginning. This page is designed to help you take the first steps.
Clinical reasoning can be compared to detective work. In its simplest form, it involves the processes of collecting, interpreting, and integrating relevant clinical information to reach a ‘working diagnosis’ and determine an effective approach to management.
You can also think of clinical reasoning as completing a jigsaw puzzle. We tend to start with the edges first, filling in gaps with parts of the picture once we have an outline to work from. In clinical reasoning, you start with the patient history (which usually forms the edges) and fill the gaps with examination findings, investigation results, clinical guidelines, and the patient’s wishes.

Clinicians are presented with immense amounts of data every day. After seeing a patient, we have collected information including a clinical history, examination findings, and (possibly) investigation results.
On top of this, we may have biases in the way we think, we may have advice from team members to consider, and we work in a naturally chaotic environment (potentially at strange times of day) … AND we look after patients who are individuals with their own thoughts, concerns and preferences who may not present like the textbooks say they will.
Making sense of this information can feel overwhelming. It is therefore important to have a robust thinking process that helps clinicians to filter through the information to determine a diagnosis, consider further investigations, or create a patient-centred management plan. This process is clinical reasoning.
A technical perspective on clinical reasoning…
Young et al. define clinical reasoning using specific stages; ‘gathering and synthesizing information’; ‘generating hypotheses’; and ‘formulating a clinical impression, prognosis, diagnosis, treatment, care, and/or management plan’.1
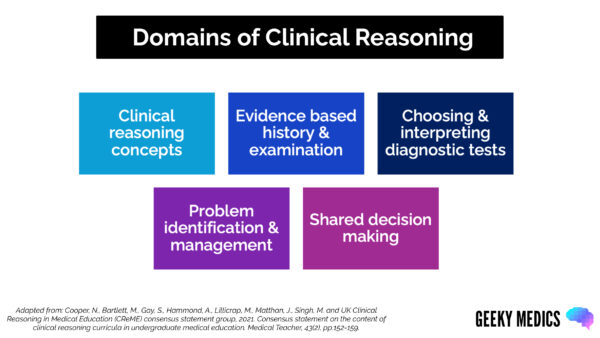
The Clinical Reasoning in Medical Education (CReME) group describes key ‘domains’ of clinical reasoning.2 This helps us to consider different facets of the clinical reasoning process.
In addition, it is important to remember that clinical reasoning is not just about ‘thinking’; it should also involve ‘thinking about thinking’ or metacognition. Clinicians should reflect on their thinking in detail throughout the clinical reasoning process. They should be questioning not only the clinical information itself but how and why they collected the information they did.
Why is clinical reasoning important?
Clinical reasoning is of interest to medical educators and medical students because of its importance in clinical practice, particularly in relation to patient safety.2
Obtaining a good grasp of clinical reasoning processes and principles in medical school is important to safeguard patients when you graduate. There is an emerging stance that clinical reasoning should be taught more explicitly in medical education.3
Some UK medical schools have already begun to do this, and you may encounter purposely designed clinical reasoning teaching in your education.
Your clinical reasoning skills are frequently tested in medical school because they are the building blocks of safe and effective clinical practice.
The role of clinical reasoning
- It allows clinicians to recognise patterns in patient presentations and, therefore, reach conclusions efficiently based on rich experience.
- It helps to guide which questions to ask/which focused examinations to perform to differentiate between different problems.
- It helps healthcare professionals to decide on the most appropriate and relevant investigations to distinguish between diagnoses (this protects patients from unnecessary and potentially invasive/radiation-exposing investigations, and also ensures that investigations are targeted and cost-effective).
- It allows clinicians to consider what steps are clinically appropriate for individual patients based on a more holistic assessment of their needs, medical history, and wishes.
When implemented well, a strong understanding of clinical reasoning helps clinicians deliver safe, effective and patient-centred care.
Preparing for exams
Understanding clinical reasoning in medical school will help you prepare for placements, understand the rationale behind healthcare professionals’ decisions, and prepare for your medical school exams.
See our guide to using clinical reasoning in exams for more information.
Key components of clinical reasoning
Below, we provide a brief outline of each of the key CReME domains of clinical reasoning. We have also included a table within each domain with some core clinical reasoning terms you might encounter.
1. Clinical reasoning concepts
This first domain of clinical reasoning requires the practitioner to understand some of the processes going on in their minds when they approach a clinical scenario. By understanding these processes, a clinician can remain alert to and challenge potential flaws in their own reasoning.
Table 1. Key clinical reasoning concepts
| Key term | Definition |
| Cognitive bias | Cognitive biases are mental short-cuts used to aid our decision-making. The human brain has a tendency to pick certain answers based on flawed logic, which can result in incorrect conclusions being drawn, |
|
Illness scripts |
These are the mental tables/spider diagrams/mind-palaces that house all of the information known about a condition in your brain. These help us to spot diagnoses more easily through pattern recognition when patients present. |
|
Hypothetico-deductive reasoning |
A cyclical pattern of proposing hypotheses and trying to prove or disprove them using the information available. |
| Dual process reasoning | A combination of both ‘fast’ (intuitive approach) and ‘slow’ (analytic approach) thinking. The brain relies on pattern recognition where possible, but also needs to utilise critical analysis and complex thinking when pattern recognition isn’t available – or if it has jumped to the wrong conclusion. |
2. History and physical examination
You will choose the history questions and examination components that you feel will help you distinguish between key features of a patient’s presentation.
This will help you to rule things in and rule things out and make a plan. To begin with, you might take a ‘checklist history’ and realise a lot of the information you’ve gathered is irrelevant. Equally, you might take a history and realise that key information is missing.
Over time, as you practice, you will work out how to tailor your clinical skills to individual patient encounters.
3. Choosing and interpreting diagnostic tests
As you build your illness scripts from experience with patients, you will understand what tests you need to request to ‘rule things in’ and ‘rule things out’ if you cannot do this through history and examination alone.
It is important to avoid performing tests ‘for the sake of it’ and ensure that your investigations always aim to answer a relevant clinical question.
4. Problem identification and management
Once you’ve gathered the information, you must rationalise and summarise it.
This might include presenting a case, creating problem lists, and identifying differential diagnoses. From here, you can consider evidence-based management options.
Table 2. Key terms in problem identification and management
| Key term | Definition |
| Semantic qualifiers | Paired opposing terms used to describe specific aspects of a clinical presentation (e.g. acute/chronic onset, sharp/dull pain, pleuritic/non-pleuritic). |
| Problem representation | Using semantic qualifiers to give a precise clinical summary of the relevant clinical information pertaining to a patient presentation. |
| Differential diagnosis | A list of possible diagnoses that may explain the patient presentation. |
| Problem list | A list of the most relevant biopsychosocial problems which may influence the presentation and ongoing care of the patient (e.g. constipation, social isolation, electrolyte disturbance). |
5. Shared decision-making
You should discuss the management options with the patient (and the wider team, where applicable) to determine the most appropriate plan.
Shared decision making is a vast topic, and it is beyond the scope of this article to cover in sufficient detail. We suggest you read around this topic further to gain a rich understanding of this.
How to approach clinical reasoning
Why vs What
The key transition that will help you engage your clinical reasoning skills is to think about “why” you’re doing something, not just “what” you’re doing.
Table 3. Examples of asking “why”
| What | Why |
| I’m going to ask about the patient’s drug history | The drug history might give me clues about potential causes or complications of the patient’s epigastric pain, so I will specifically ask them about NSAID/steroid use, PPI use and anticoagulant use. |
| I’m going to ask the patient about their social history | If the patient has a diagnosis of bowel cancer, I need to see whether they would be fit enough to survive the surgery, so I will ask in detail about their baseline function before admission. |
| I’m going to do a neurological examination | I need to pick up on signs that are suggestive of Parkinson’s disease, therefore I will include assessment of distractable cog-wheeling and writing in my examination. |
| I’m going to request an FBC | An FBC will help me to assess for an elevated WCC, which will help me to assess the likelihood of infection. |
Thinking about the “why” makes the biggest difference between performing a checklist and engaging in an insightful and patient-specific clinical assessment.
This is difficult for a junior (and even senior) medical student. We suggest you start by doing a ‘full version’ of a history/examination and thinking about these questions afterwards. Eventually, you will learn to integrate them as you go along.
An important note about exams…
In some circumstances (such as exams/OSCEs), you must demonstrate that you know how to perform a skill fully (e.g., a complete neurological examination).
In this setting, you might not be able to tailor your approach, but you can still actively think about what signs/symptoms you’re looking for while examining. Please seek advice from your educational institution regarding what is expected of you in your exams.
Observing clinical reasoning
Every day on placement, and in teaching sessions, you will observe clinical reasoning. However, as discussed at the beginning of this article, clinical reasoning often happens internally, and clinicians do not always voice their thought processes out loud. Ask clinicians to explain the rationale behind the decisions they make to help you learn:
- “Please could you tell me why you have requested a lumbar puncture for this patient? What signs/symptoms pointed you towards this investigation? What differentials are you trying to rule in/rule out?”
- “Please could you explain the important positive findings and important negative findings that helped you reach the diagnosis of bipolar affective disorder?”
- “What factors led you to conclude that non-operative management was the best course of action for this patient? How did the patient influence the management plan?”
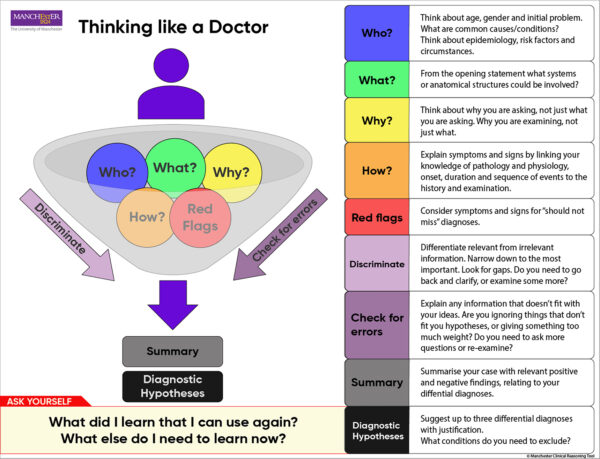
Manchester Clinical Reasoning Tool
The Manchester Clinical Reasoning Tool provides a useful graphical representation of the thoughts you should have when approaching a clinical scenario.4 Engaging in these types of thoughts will help you think more like a doctor.
Clinical reasoning activities
Ready to try out what you have learned? We have produced resources to help you develop clinical reasoning skills on clinical placement and in your own time:
- Clinical reasoning games and activities: a collection of games and activities, including downloadable worksheets
- Clinical reasoning clerking: how to make the most of patient encounters to develop your clinical reasoning
You may also be interested in our guide to using clinical reasoning in exams.
References
- Young M, Thomas A, Lubarsky S, Ballard T, Gordon D, Gruppen LD, et al. Drawing Boundaries: The Difficulty in Defining Clinical Reasoning. Academic Medicine. 2018;93(7):990–5.
- Cooper N, Bartlett M, Gay S, Hammond A, Lillicrap M, Matthan J, et al. Consensus statement on the content of clinical reasoning curricula in undergraduate medical education. Medical Teacher. 2021 Feb 1;43(2):152–9.
- Graber ML, Rencic J, Rusz D, Papa F, Croskerry P, Zierler B, et al. Improving diagnosis by improving education: a policy brief on education in healthcare professions. Diagnosis. 2018;5(3):107–18.
- Singh M, Collins L, Farrington R, Jones M, Thampy H, Watson P, Warner C, Wilson K, Grundy J. From principles to practice: embedding clinical reasoning as a longitudinal curriculum theme in a medical school programme. Diagnosis. 2022 May 11;9(2):184-94.
Figure 1. kallerna. Jigsaw puzzle solving 2. License: [CC BY-SA]




