- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
A Bartholin’s cyst is a fluid-filled sac in one of the Bartholin glands of the vagina. They occur in approximately 3% of women, typically of childbearing age.1
Bartholin’s cysts and abscesses account for approximately 2% of all annual gynaecological visits.2
Aetiology
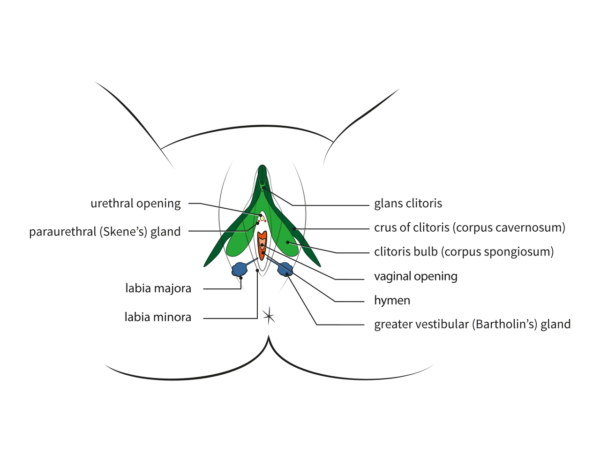
The Bartholin’s glands (greater vestibular glands) are paired and located at the posterior aspect of the labia majora. The gland openings are in the 4 o’clock and 8 o’clock position, on either side of the vaginal orifice within the vestibule. The function of these glands is mucus secretion, providing lubrication for the vagina. Generally, they cannot be palpated.
Cysts form when an accumulation of mucus secretions causes the gland to become blocked.
Risk factors
Women of childbearing age (between 20 and 30) who are nulliparous or of low parity are most affected.
There are several other risk factors to consider:
- Personal history of previous Bartholin’s cysts
- History of vulval surgery
- Being sexually active (some cysts or abscesses are thought to be linked to sexually transmitted infections, STIs)
- Previous vulval trauma
Clinical features
History
Small cysts may be asymptomatic. However, in cases where they have become larger, typical symptoms include:
- Vulvar pain, especially when walking or sitting
- Superficial dyspareunia (pain during sexual intercourse)
- Rapid onset of symptoms over a few days to hours with acute pain
- Difficulty passing urine
- Sudden relief of pain, which would indicate spontaneous cyst rupture
- Vaginal discharge (very likely in women with bacterial infections or STIs)
It is also important to ascertain the patient’s previous history of Bartholin’s cyst and whether this is becoming a recurrent issue.
Clinical examination
When suspecting a Bartholin’s cyst, clinical examination is essential.
A unilateral labial mass will be seen. This mass will arise from the posterior aspect of the labia majora, but there will be anterior expansion in cases where it has become significantly large.
If left untreated, the cyst can become infected, resulting in the formation of an abscess.
During the examination, it is important to differentiate between a Bartholin’s cyst and an abscess; this will help to guide management:4
- Bartholin’s cyst: non-tender, soft and fluctuant on palpation
- Bartholin’s abscess: tense and firm with surrounding erythema/ cellulitis
Differential diagnoses
These differentials are considered for labial or vulval masses:
- Sebaceous cyst
- Folliculitis
- Lipoma
- Fibroma
- Haematoma
- Hidradenitis suppurativa
- Bartholin’s gland carcinoma
- Bartholin’s gland tumour (e.g. adenoma or nodular hyperplasia)
Investigations
The diagnosis of Bartholin’s cysts is usually clinical, through bedside examination. In most cases, there is no necessity for further investigation.
Laboratory investigations
Where appropriate (for management purposes), a swab of the cyst/abscess contents should be taken. Laboratory findings most commonly confirm skin commensal organisms rather than pathogens.
In infection, aerobic organisms are the most common causative pathogens and Escherichia coli predominates. Occasionally, organisms that cause sexually transmitted infections, such as gonorrhoea or chlamydia, may also be cultured. Treatment regimens can then be tailored to target the identified causative organism(s).
Biopsy
It is important to note that women over the age of 40 presenting with a Bartholin’s cyst should have a biopsy taken of the region to rule out carcinoma.
Whilst unusual, vulval malignancies can occasionally present in this way. Carcinoma of the Bartholin’s gland itself accounts for approximately 5% of all vulval carcinomas.5
Management
In cases where the cyst is small or asymptomatic, there is no need to initiate treatment. Warm baths can be recommended to try to stimulate spontaneous rupture.
Medical management
Antibiotic therapy may be initiated, if necessary, with swabs and cultures taken from the cyst. Generally, this is only when the individual is systemically unwell or immunocompromised.
Surgical management
There are two main surgical management options: word catheter or marsupialisation.
Word catheter
Performed under local anaesthetic. A small incision is made into the cyst/ abscess, and a catheter is inserted. The catheter tip (balloon) is inflated with up to 3ml of saline.
This is then left in place for up to 4 weeks, allowing for epithelialisation of the tract that has been created. Fluid from the cyst can drain around the catheter tubing. Once epithelialisation has occurred, the catheter can be removed.6
Marsupialisation
Performed under general anaesthesia. A small vertical incision is made into the cyst behind the hymenal ring of the vagina, this allows for spontaneous drainage of the cyst.
The wall of the cyst is then everted and sutured to the end of the vaginal mucosa. The cyst has been sutured open, preventing recurrence.
Other treatment options
There are some other treatment options, although far less common and rarely used nowadays. These include:
- Silver nitrate cautery: cyst/ abscess drained, and small stick of silver nitrate inserted into the cavity once fluid has drained. This is left for 2/3 days at which point the contents are removed or they fall out on their own.
- Carbon dioxide laser: used to create an opening on the surface of the cyst/ abscess so the cyst can drain.
- Needle aspiration: used to drain the cyst. In some instances, alcohol sclerotherapy is used whereby the cavity is filled with 70% alcohol fluid, left for 5 minutes and then drained.
Generally, complete excision and removal of the gland is avoided except in instances where malignancy is suspected/ confirmed or there are very high rates of recurrence and treatments have so far been unsuccessful.4
Complications
Complications if Bartholin’s cyst/abscess are left untreated include:
- Spread of infection to local structures
- Bacteraemia and potential sepsis
Possible complications of balloon catheter insertion include:
- Pain at the site of the catheter insertion
- Pain/discomfort during sexual intercourse
- Local oedema around the labia
- Infection
- Bleeding
- Scarring
Complications post marsupialisation are rare but include:
- Infection
- Cyst/abscess recurrence
- Bleeding
- Pain
Key points
- Bartholin’s glands are paired and located either side of the vagina orifice in the vestibule.
- Cysts/ abscesses arise from mucus secretion build-up, leading to outflow obstruction.
- They are very common, with the highest prevalence in nulliparous women of childbearing age.
- Suspicion of malignancy should always arise with women presenting over 40 years of age with Bartholin’s cyst.
- Treatment is either use of a word catheter or marsupialisation.
- When there is a clear infection, or the patient is systemically unwell, then antibiotic therapy should also be initiated.
Reviewer
Mr Michael Stephanou
Consultant Obstetrician & Gynaecologist
Editor
Dr Chris Jefferies
References
- Berger, M. B., Betschart, C., Khandwala, N., DeLancey, J. O., & Haefner, H. K. (2012). Incidental bartholin gland cysts identified on pelvic magnetic resonance imaging. Obstetrics & Gynecology, 120(4), 798-802.
- Marzano, D. A., & Haefner, H. K. (2004). The bartholin gland cyst: past, present, and future. Journal of lower genital tract disease, 8(3), 195-204.
- R. Dewaele (Bioscope, Unige), J. Abdulcadir (HUG), C. Brockmann (Bioscope, Unige), O. Fillod, S. Valera-Kummer (DIP), Female anatomy showing Bartholin’s glans. License: [CC BY-SA]
- Lee, W.A. (2023) Bartholin gland cyst, StatPearls. Available from: [LINK]
- Heller, D. S., & Bean, S. (2014). Lesions of the Bartholin gland: a review. Journal of lower genital tract disease, 18(4), 351-357.
- NICE. Balloon catheter insertion for Bartholin’s cyst or abscess; NICE Interventional Procedure Guidance. Published in 2009. Available from: [LINK]




