- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Coeliac disease is an autoimmune disorder that is characterised by gluten sensitivity. It is one of the most prevalent gastroenterological conditions worldwide in both children and adults.
In the UK, around 1% of the population are affected by coeliac disease.1
Women are more likely to be affected and account for around two-thirds of cases.2
There are two peak age periods seen in the diagnosis of coeliac disease. The first peak occurs in infancy when children are beginning to be exposed to solid foods containing gluten, and a second larger peak between 40-50 years old. However, coeliac disease can be diagnosed at any age.3,4
Aetiology
In coeliac disease, gliadin, a component of gluten, is not broken down fully and passes through the intestinal epithelial layer triggering an immune response.
Gliadin binds to HLA DQ2 or DQ8 which activates T-cells in the intestinal mucosa leading to the immune response. The immune response results in chronic inflammation within the small bowel, damaging the epithelium and ultimately resulting in malabsorption.5
Almost all patients with coeliac disease are HLA DQ2 positive and many are also DQ8 positive.
Risk factors
There are a number of risk factors for coeliac disease. These factors, and the lifetime prevalence of developing coeliac disease, are listed below:6
- Genetics (around 70% if monozygotic twin affected)
- Autoimmune thyroid disease (15%)
- Genetic syndromes e.g. Down’s and William’s syndrome (up to 12%)
- Type 1 diabetes mellitus (8%)
- IgA deficiency (7%)
Clinical features
History
The symptoms of coeliac disease can differ slightly between children and adults.
Typical symptoms of coeliac disease in children include:6
- Failure to thrive (stunted growth, growth chart faltering)
- Chronic diarrhoea
- Constipation (coeliac disease should be considered whenever diagnosing idiopathic constipation)
- Abdominal bloating
- Irritability
- Features of anaemia (adolescents)
Children normally present with these symptoms in the first few years of life as gluten products are introduced to their diets.
Typical symptoms of coeliac disease in adults include:3
- Long-standing diarrhoea (may be intermittent in nature)
- Nausea and vomiting
- Fatigue (patients often have underlying iron-deficiency anaemia)
- Weight loss
Other important areas to cover in the history:
- Family history: coeliac disease often runs in families and those with an affected first-degree family member have around a 10% chance of developing it.7
- Associated conditions: there are a range of conditions that, if present, would increase the risk of coeliac disease. These conditions are listed below.7
Conditions associated with coeliac disease
Mnemonic: “I Don’t Take Apples, I Take Oranges”
- IgA deficiency
- Down’s syndrome
- Turner’s syndrome
- Autoimmune thyroid disease and autoimmune hepatitis
- IgA nephropathy
- Type 1 diabetes mellitus
- Other autoimmune conditions (e.g. Sjögren’s, myasthenia gravis, Addison’s disease)
Clinical examination
The clinical features of coeliac differ between children and adults. All children and adults who present with features of coeliac disease should receive a thorough clinical examination.
Clinical features that may be identified in children with coeliac disease include:6
- Failure to thrive (although less common due to increased calorific diets in modern western diet)
- Abdominal distension
- Abdominal pain
- Muscle wasting (usually the buttocks are predominantly affected)
- Features of anaemia (adolescents) e.g. angular cheilitis, fatigue and pallor
Clinical features that may be identified in adults with coeliac disease include:3
- Features of anaemia
- Mouth ulcers
- Weight loss (most adults will not experience significant weight loss)
- Anxiety features
- Joint pain
- Abdominal pain
- Dermatitis herpetiformis
Extra-intestinal manifestations of coeliac disease
There is a range of extra-intestinal manifestations of coeliac disease and you should look out for these when taking a medical history and examining patients. These features include:8
- Arthritis
- Dermatitis herpetiformis
- Osteoporosis/osteopenia
- Infertility
- Ataxia
- Epilepsy
- Anxiety
- Depression
Investigations
The diagnosis of coeliac disease is based on immunological investigation results and the histology of small bowel biopsies.
Coeliac features are often non-specific and many patients have mild to moderate disease making the diagnosis difficult.
There is no role for a trial of a gluten-free diet in terms of diagnosis. All patients with suspected coeliac disease should receive an antibody screen followed by a duodenal biopsy if appropriate.1
The average time to diagnosis from first symptoms is around 13 years in the UK.1
Laboratory investigations
- Anti-tissue transglutaminase (tTG) antibodies and total IgA count: anti-tTG antibodies are diagnostic of coeliac disease if strongly positive. A total IgA count is required as an underlying IgA deficiency can results in false-negative results, masking coeliac disease.9 If TTG is 10x the upper limit of normal, a positive endomysial antibody (EMA) screen is required.
- IgG endomysial antibodies (EMA), IgG deamidated gliadin peptide (DGP) or IgG tTG: in those who are IgA deficient, IgG EMA, IgG DGP or IgG tTG can be used to diagnose coeliac disease.9 Performing these tests first-line to screen for coeliac disease is not recommended.
- Genetic HLA DQ2 and DQ8 screen: currently, in the UK, positive genetic testing is also required, however, this is likely to change over time as many patients who are HLA DQ2 and DQ8 positive do not have coeliac disease.
If TTG, EMA and genetic testing is positive, children do not require a duodenal biopsy and the diagnosis of coeliac disease can be made.6
Duodenal biopsy
If serology markers are positive, a small bowel biopsy is carried out by gastroenterology to support the diagnosis.
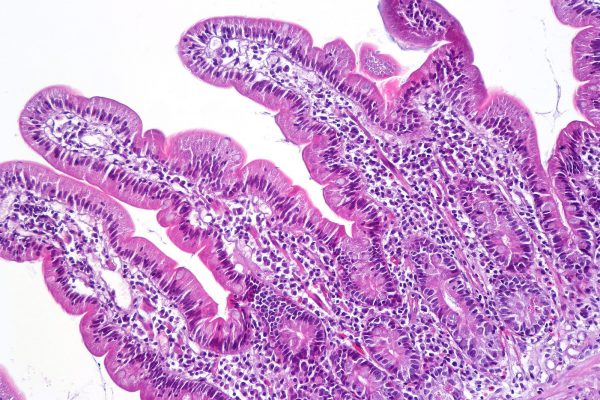
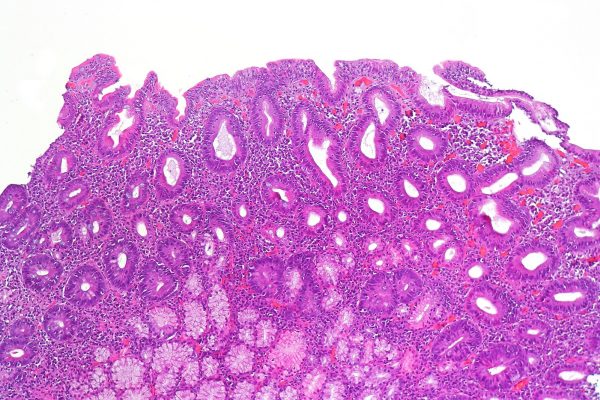
There are four key changes that are seen on duodenal biopsy in those with coeliac disease:10
- Presence of villous atrophy leading to a flat mucosa
- Crypt cell hyperplasia
- Intraepithelial cell lymphocytosis
- Inflammatory cell infiltration of the lamina propria
The villous atrophy and the immunology findings that are used in the diagnosis of coeliac disease often normalise following the removal of gluten from the diet.
Therefore, those who have removed gluten from their diet and subsequently request testing, cannot be tested. You should advise to reintroduce gluten into the diet and return in 6-8 weeks if a formal diagnosis is necessary.1
Differential diagnoses
There is a range of conditions that can present in a similar fashion to coeliac disease and which should be considered during the diagnostic workup.
Some of the main differentials include:13
- Anorexia nervosa
- Bacterial overgrowth of the small bowel
- Crohn’s disease
- Irritable bowel syndrome
- Lactose intolerance
- Autoimmune enteropathy
Management
Children with suspected coeliac disease should be referred to a paediatric gastroenterologist or an appropriate paediatrician with a special interest in gastroenterology.7
There are two key aspects of management in coeliac disease:
- Lifelong gluten-free diet: foods containing gluten include rye, wheat, barley and oats. Dietetic input may be required and should be considered case by case.
- Immunisation: individuals with coeliac disease often have functional hyposplenism (defective immune response) and therefore require pneumococcal vaccines every 5 years. Yearly influenza vaccines may be given to patients, however, this is on a case by case basis.
Follow-up
Patients with coeliac disease should be followed up annually reviewing weight, height, ongoing symptoms and the need for dietetic input.9
In those with ongoing symptoms, IgA tTG measurements can be carried out to check for compliance with a gluten-free diet. Adults with well-controlled disease may be followed up less frequently.14
Complications
Untreated disease can result in numerous complications including:15
- Hyposplenism (anatomical or functional)
- Iron deficiency anaemia
- Malnutrition
- Osteoporosis
- Small bowel T-cell lymphoma
- Vitamin B12 and folate deficiency (you may see mixed anaemia if iron deficiency is also present)
Key points
- Coeliac disease is a common gastrointestinal disorder caused by a sensitivity to gluten.
- Common symptoms include diarrhoea, abdominal bloating and features of malnutrition.
- Diagnosis is achieved by serology (anti-tissue transglutaminase antibodies) and biopsy (duodenum).
- Treatment is with a life-long gluten-free diet.
- Complications include malignancy of the small bowel, hyposplenism and malnutrition.
Reviewer
Dr Owen Wilson
ST3 Paediatrics
Editor
Dr Chris Jefferies
References
- Payne, D., 2018. Coeliac Disease. [online] Patient.info. Available from: [LINK].
- Singh, P., Arora, A., Strand, T., Leffler, D., Catassi, C., Green, P., Kelly, C., Ahuja, V. and Makharia, G., 2018. Global Prevalence of Celiac Disease: Systematic Review and Meta-analysis. Clinical Gastroenterology and Hepatology, 16(6), pp.823-836.e2.
- Green, P., 2005. The many faces of celiac disease: Clinical presentation of celiac disease in the adult population. Gastroenterology, 128(4), pp.S74-S78.
- Green, P., Stavropoulos, S., Panagi, S., Goldstein, S., McMahon, D., Absan, H. and Neugut, A., 2001. Characteristics of adult celiac disease in the USA: results of a national survey. The American Journal of Gastroenterology, 96(1), pp.126-131.
- Pelkowski, T., 2014. Celiac Disease: Diagnosis and Management. American Family Physician, 89(2), pp.99-105.
- Coeliac UK. 2013. BSPGHAN Guidelines For Diagnosis Of Coeliac Disease In Children. [online] Available at: <https://www.coeliac.org.uk/document-library/122-bspghan/> [Accessed 22 June 2020].
- nhs.uk. 2019. Coeliac Disease – Causes. [online] Available from: [LINK].
- Barker, J. and Liu, E., 2008. Celiac Disease: Pathophysiology, Clinical Manifestations, and Associated Autoimmune Conditions. Advances in Pediatrics, 55(1), pp.349-365.
- National Institute for Health and Care Excellence. 2015. Overview | Coeliac Disease: Recognition, Assessment and Management | Guidance | NICE. [online] Available from: [LINK].
- Kamboj, A. and Oxentenko, A., 2017. Clinical and Histologic Mimickers of Celiac Disease. Clinical and Translational Gastroenterology, 8(8), p.e114.
- CoRus13. Duodenal biopsy showing normal mucosa. License: [CC-BY-SA]. Available from: [LINK].
- CoRus13. Gluten-sensitive enteropathy (Marsh 3c). License: [CC-BY-SA]. Available from: [LINK].
- Presutti, R., Cangemi, J., Cassidy, H. and Hill, D., 2008. Celiac Disease. American family physician, 76(12), pp.1795-802.
- Caio, G., Volta, U., Sapone, A., Leffler, D., De Giorgio, R., Catassi, C. and Fasano, A., 2019. Celiac disease: a comprehensive current review. BMC Medicine, 17(142).
- nhs.uk. 2019. Coeliac Disease – Complications. [online] Available at: [LINK].