- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The Glasgow Coma Scale (GCS) allows healthcare professionals to consistently evaluate the level of consciousness of a patient. It is commonly used in the context of head trauma, but it is also useful in a wide variety of other non-trauma related settings. Regular assessment of a patient’s GCS can identify early signs of deterioration.
There are three aspects of behaviour that are independently measured as part of an assessment of a patient’s GCS – motor responsiveness, verbal performance and eye-opening. The highest response from each category elicited by the healthcare professional is scored on the chart.
The highest possible score is 15 (fully conscious) and the lowest possible score is 3 (coma or dead).
Eye-opening (E)
A maximum possible score of 4 points
Eyes opening spontaneously (4 points)
To assess eye response, initially observe if the patient is opening their eyes spontaneously.
If the patient is opening their eyes spontaneously, your assessment of this behaviour is complete, with the patient scoring 4 points. You would then move on to assessing verbal response, as shown in the next section. If however, the patient is not opening their eyes spontaneously, you need to work through the following steps until a response is obtained.
Eyes opening to sound (3 points)
If the patient doesn’t open their eyes spontaneously, you need to speak to the patient “Hey Mrs Smith, are you ok?”
If the patient’s eyes open in response to the sound of your voice, they score 3 points.
Eyes opening to pain (2 points)
If the patient doesn’t open their eyes in response to sound, you need to move on to assessing eye-opening to pain.
There are different ways of assessing response to pain, but the most common are:
- Applying pressure to one of the patient’s fingertips
- Squeezing one of the patient’s trapezius muscles (known as a trapezius squeeze)
- Applying pressure to the patient’s supraorbital notch
If the patient’s eyes open in response to a painful stimulus, they score 2 points.
No response (1 point)
If the patient does not open their eyes to a painful stimulus, they score 1 point.
Not testable (NT)
If the patient cannot open their eyes for some reason (e.g. oedema, trauma, dressings), you should document that eye response could not be assessed (NT).
Summary
| Criterion | Score |
| Eye-opening spontaneously | 4 points |
| Eye-opening to sound | 3 points |
| Eye-opening to pain | 2 points |
| No response | 1 point |
| Not testable | NT |
Verbal response (V)
A maximum possible score of 5 points
Assessing a patient’s verbal response initially involves trying to engage the patient in conversation and assess if they are orientated.
You should score the patient based on the highest scoring response they demonstrate during the assessment.
Some common questions you can ask to help assess this might include:
- “Can you tell me your name?”
- “Do you know where you are at the moment?”
- “Do you know what the date is today?”
Orientated response (5 points)
If the patient is able to answer your questions appropriately, the assessment of verbal response is complete, with the patient scoring 5 points.
Confused conversation (4 points)
If the patient is able to reply, but their responses don’t seem quite right (e.g. they don’t know where they are, or what the date is), this would be classed as confused conversation and they would score 4 points.
Sometimes confusion can be quite subtle, so pay close attention to their responses.
Inappropriate words (3 points)
If the patient responds with seemingly random words that are completely unrelated to the question you asked, this would be classed as inappropriate words and they would score 3 points.
Incomprehensible sounds (2 points)
If the patient is making sounds, rather than speaking words (e.g. groans) then this would be classed as incomprehensible sounds, with the patient scoring 2 points.
No response (1 point)
If the patient has no response to your questions, they would score 1 point.
Not testable (NT)
If the patient is intubated or has other factors interfering with their ability to communicate verbally, their response cannot be tested, and for this, you would write NT (not testable).
| Criterion | Score |
| Orientated | 5 points |
| Confused conversation | 4 points |
| Inappropriate words | 3 points |
| Incomprehensible sounds | 2 points |
| No response | 1 point |
| Not testable | NT |
Motor response (M)
A maximum possible score of 6 points
The final part of the GCS assessment involves assessing a patient’s motor response.
You should score the patient based on the highest scoring response you were able to elicit in any single limb (e.g. if they were unable to move their right arm, but able to obey commands with their left arm, they’d receive a score of 6 points).
Obeys commands (6 points)
Ask the patient to perform a two-part request (e.g. “Lift your right arm off the bed and make a fist.”).
If they are able to follow this command correctly, they would score 6 points and the assessment would be over.
Localises to pain (5 points)
This assessment involves applying a painful stimulus and observing the patient for a response.
There are different ways of assessing response to pain, but the most common are:
- Squeezing one of the patient’s trapezius muscles (known as a trapezius squeeze)
- Applying pressure to the patient’s supraorbital notch
If the patient makes attempts to reach towards the site at which you are applying a painful stimulus (e.g. head, neck) and brings their hand above their clavicle, this would be classed as localising to pain, with the patient scoring 5 points.
Withdraws to pain (4 points)
This is another possible response to a painful stimulus, which involves the patient trying to withdraw from the pain (e.g. the patient tries to pull their arm away from you when applying a painful stimulus to their fingertip).
This response is also referred to as a “normal flexion response” as the patient typically flexes their arm rapidly at their elbow to move away from the painful stimulus.
It differs from the “abnormal flexion response to pain” shown below due to the absence of the other features mentioned (e.g. internal rotation of the shoulder, pronation of the forearm, wrist flexion).
Withdrawal to pain scores 4 points on the Glasgow Coma Scale.
Abnormal flexion response to pain (3 points)
Abnormal flexion to a painful stimulus typically involves adduction of the arm, internal rotation of the shoulder, flexion of the elbow, pronation of the forearm and wrist flexion (known as decorticate posturing).
Decorticate posturing indicates that there may be significant damage to areas including the cerebral hemispheres, the internal capsule, and the thalamus.
Abnormal extension response to pain (2 points)
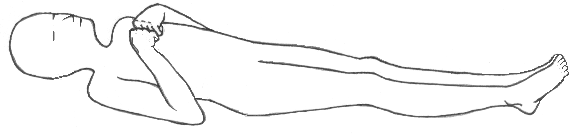
Abnormal extension to a painful stimulus is also known as decerebrate posturing.
In decerebrate posturing, the head is extended, with the arms and legs also extended and internally rotated.
The patient appears rigid with their teeth clenched.
The signs can be on just one side of the body or on both sides (the signs may only be present in the upper limbs).
Decerebrate posturing indicates brain stem damage. It is exhibited by people with lesions or compression in the midbrain and lesions in the cerebellum.
Progression from decorticate posturing to decerebrate posturing is often indicative of uncal (transtentorial) or tonsilar brain herniation (often referred to as coning).

No response (1 point)
The complete absence of a motor response to a painful stimulus scores 1 point.
Not testable (NT)
If the patient is unable to provide a motor response (e.g. paralysis), this should be documented as not testable (NT).
| Criterion | Score |
| Obeys command | 6 points |
| Localises to pain | 5 points |
| Withdraws to pain | 4 points |
| Flexion decorticate posture | 3 points |
| Abnormal extension decerebrate posture | 2 points |
| No response | 1 point |
| Not testable | NT |
Summary
Once you have assessed eye-opening, verbal response and motor response you add the scores together to calculate the patient’s GCS.
The GCS should be documented showing the score for each individual behaviour tested:
- GCS 15 [E4, V5, M6]
References
- Teasdale G, Jennett B; Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974 Jul 13 2(7872):81-4. Available from: [LINK].
- Royal College of Physicians and Surgeons of Glasgow. GLASGOW COMA SCALE: Do it this way. Available from: [HERE].




