- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
What is cardiotocography?
Cardiotocography (CTG) is used during pregnancy to monitor fetal heart rate and uterine contractions. It is most commonly used in the third trimester and its purpose is to monitor fetal well-being and allow early detection of fetal distress. An abnormal CTG may indicate the need for further investigations and potential intervention.
How CTG works
The device used in cardiotocography is known as a cardiotocograph. It involves the placement of two transducers onto the abdomen of a pregnant woman. One transducer records the fetal heart rate using ultrasound and the other transducer monitors the contractions of the uterus by measuring the tension of the maternal abdominal wall (providing an indirect indication of intrauterine pressure). The CTG is then assessed by a midwife and the obstetric medical team.
How to read a CTG
To interpret a CTG you need a structured method of assessing its various characteristics. The most popular structure can be remembered using the acronym DR C BRAVADO:
- DR: Define risk
- C: Contractions
- BRa: Baseline rate
- V: Variability
- A: Accelerations
- D: Decelerations
- O: Overall impression
Define risk
When performing CTG interpretation, you first need to determine if the pregnancy is high or low risk. This is important as it gives more context to the CTG reading (e.g. if the pregnancy categorised as high-risk, the threshold for intervention may be lower). Some reasons a pregnancy may be considered high risk are shown below.1
Maternal medical illness
- Gestational diabetes
- Hypertension
- Asthma
Obstetric complications
- Multiple gestation
- Post-date gestation
- Previous cesarean section
- Intrauterine growth restriction
- Premature rupture of membranes
- Congenital malformations
- Oxytocin induction/augmentation of labour
- Pre-eclampsia
Other risk factors
- Absence of prenatal care
- Smoking
- Drug abuse
Contractions
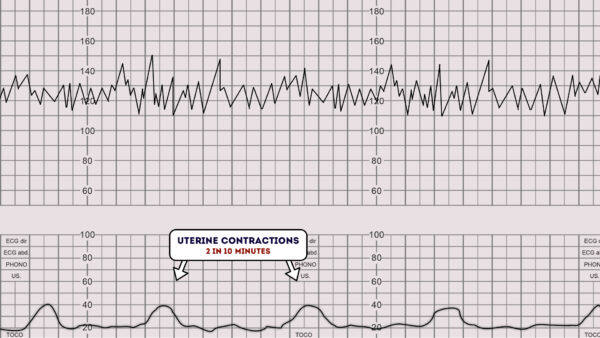
Next, you need to record the number of contractions present in a 10 minute period.
Each big square on the example CTG chart below is equal to one minute, so look at how many contractions occurred within 10 big squares.
Individual contractions are seen as peaks on the part of the CTG monitoring uterine activity.
Assess contractions for the following:
- Duration: How long do the contractions last?
- Intensity: How strong are the contractions (assessed using palpation)?
- In the below example, there are 2 contractions in a 10 minute period (this is often referred to as “2 in 10”).
Baseline rate of the fetal heart
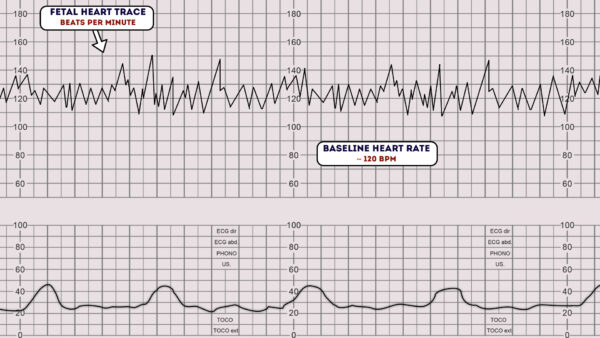
The baseline rate is the average heart rate of the fetus within a 10-minute window.
Look at the CTG and assess what the average heart rate has been over the last 10 minutes, ignoring any accelerations or decelerations.
A normal fetal heart rate is between 110-160 bpm.
Fetal tachycardia
Fetal tachycardia is defined as a baseline heart rate greater than 160 bpm.
Causes of fetal tachycardia include:
- Fetal hypoxia
- Chorioamnionitis
- Hyperthyroidism
- Fetal or maternal anaemia
- Fetal tachyarrhythmia
Fetal bradycardia
Fetal bradycardia is defined as a baseline heart rate of less than 110 bpm.
It is common to have a baseline heart rate of between 100-120 bpm in the following situations:
- Postdate gestation
- Occiput posterior or transverse presentations
Severe prolonged bradycardia (less than 80 bpm for more than 3 minutes) indicates severe hypoxia.
Causes of prolonged severe bradycardia include:
- Prolonged cord compression
- Cord prolapse
- Epidural and spinal anaesthesia
- Maternal seizures
- Rapid fetal descent
Variability
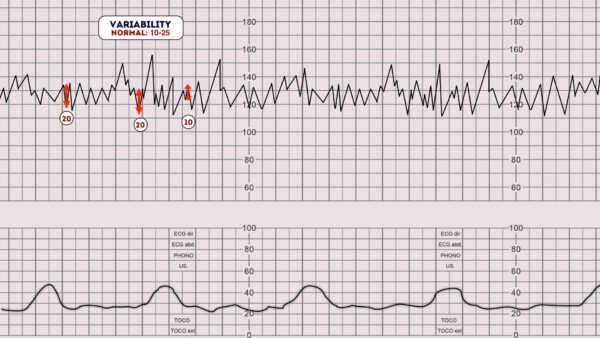
Baseline variability refers to the variation of fetal heart rate from one beat to the next.
Variability occurs as a result of the interaction between the nervous system, chemoreceptors, baroreceptors and cardiac responsiveness.
It is, therefore, a good indicator of how healthy a fetus is at that particular moment in time, as a healthy fetus will constantly be adapting its heart rate in response to changes in its environment.
Normal variability indicates an intact neurological system in the fetus.
Normal variability is between 5-25 bpm.3
To calculate variability you need to assess how much the peaks and troughs of the heart rate deviate from the baseline rate (in bpm).
Variability categorisation
Variability can be categorised as either reassuring, non-reassuring or abnormal. 3
Reassuring: 5 – 25 bpm
Non-reassuring:
- less than 5 bpm for between 30-50 minutes
- more than 25 bpm for 15-25 minutes
Abnormal:
- less than 5 bpm for more than 50 minutes
- more than 25 bpm for more than 25 minutes
- sinusoidal
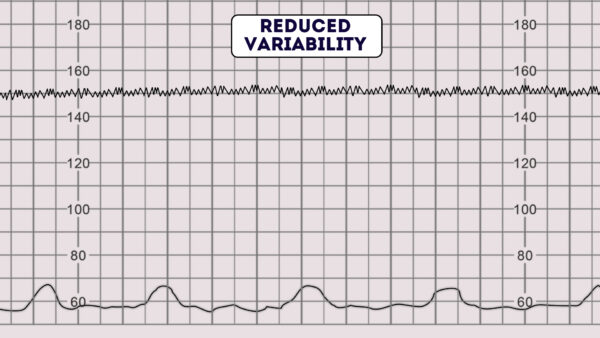
Reduced variability can be caused by any of the following:2
- Fetal sleeping: this should last no longer than 40 minutes (this is the most common cause)
- Fetal acidosis (due to hypoxia): more likely if late decelerations are also present
- Fetal tachycardia
- Drugs: opiates, benzodiazepines, methyldopa and magnesium sulphate
- Prematurity: variability is reduced at earlier gestation (<28 weeks)
- Congenital heart abnormalities
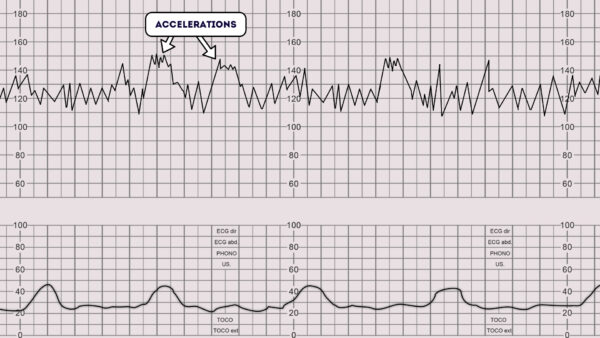
Accelerations
Accelerations are an abrupt increase in the baseline fetal heart rate of greater than 15 bpm for greater than 15 seconds.1
The presence of accelerations is reassuring.
Accelerations occurring alongside uterine contractions is a sign of a healthy fetus.
The absence of accelerations with an otherwise normal CTG is of uncertain significance.
Decelerations
Decelerations are an abrupt decrease in the baseline fetal heart rate of greater than 15 bpm for greater than 15 seconds.
The fetal heart rate is controlled by the autonomic and somatic nervous system. In response to hypoxic stress, the fetus reduces its heart rate to preserve myocardial oxygenation and perfusion. Unlike an adult, a fetus cannot increase its respiration depth and rate. This reduction in heart rate to reduce myocardial demand is referred to as a deceleration.
There are a number of different types of decelerations, each with varying significance.
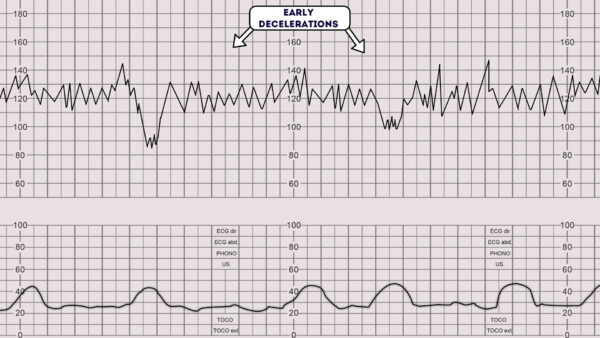
Early deceleration
Early decelerations start when the uterine contraction begins and recover when uterine contraction stops. This is due to increased fetal intracranial pressure causing increased vagal tone. It therefore quickly resolves once the uterine contraction ends and intracranial pressure reduces. This type of deceleration is, therefore, considered to be physiological and not pathological.3
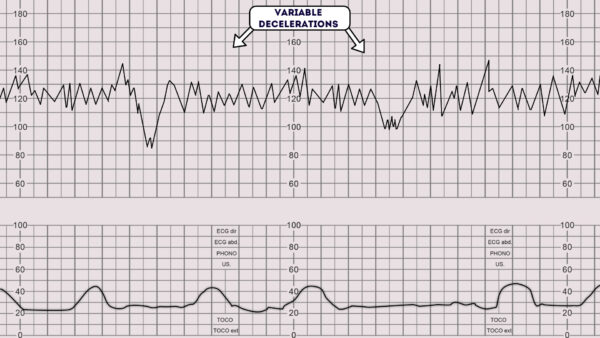
Variable deceleration
Variable decelerations are observed as a rapid fall in baseline fetal heart rate with a variable recovery phase.
They are variable in their duration and may not have any relationship to uterine contractions.
They are most often seen during labour and in patients’ with reduced amniotic fluid volume.
All fetuses experience stress during the labour process, as a result of uterine contractions reducing fetal perfusion. Whilst fetal stress is to be expected during labour, the challenge is to pick up pathological fetal distress.
Variable decelerations are usually caused by umbilical cord compression. The mechanism is as follows:1
1. The umbilical vein is often occluded first causing an acceleration of the fetal heart rate in response.
2. Then the umbilical artery is occluded causing a subsequent rapid deceleration.
3. When pressure on the cord is reduced another acceleration occurs and then the baseline rate returns.
The accelerations before and after a variable deceleration are known as the shoulders of deceleration. Their presence indicates the fetus is not yet hypoxic and is adapting to the reduced blood flow. Variable decelerations can sometimes resolve if the mother changes position. The presence of persistent variable decelerations indicates the need for close monitoring. Variable decelerations without the shoulders are more worrying, as it suggests the fetus is becoming hypoxic.
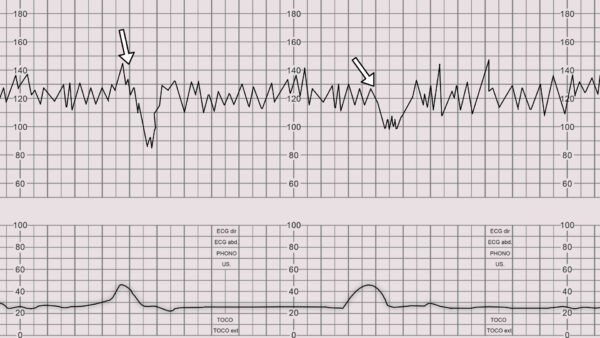
Late deceleration
Late decelerations begin at the peak of the uterine contraction and recover after the contraction ends. This type of deceleration indicates there is insufficient blood flow to the uterus and placenta. As a result, blood flow to the fetus is significantly reduced causing fetal hypoxia and acidosis.
Causes of reduced uteroplacental blood flow include:1
- Maternal hypotension
- Pre-eclampsia
- Uterine hyperstimulation
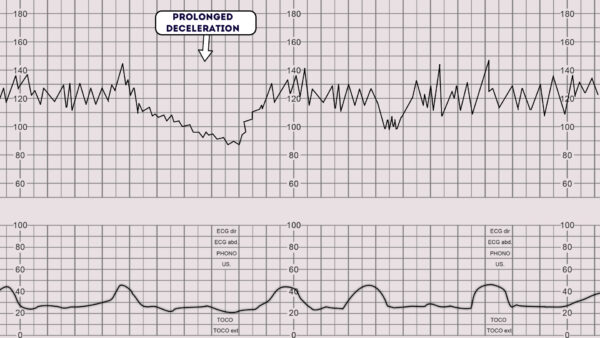
Prolonged deceleration
A prolonged deceleration is defined as a deceleration that lasts more than 2 minutes:
- If it lasts between 2-3 minutes it is classed as non-reassuring.
- If it lasts longer than 3 minutes it is immediately classed as abnormal.
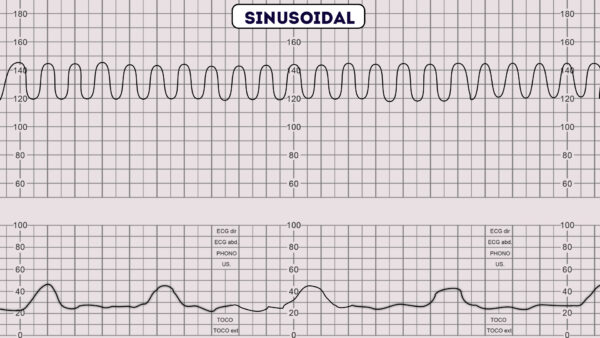
Sinusoidal pattern
A sinusoidal CTG pattern is rare, however, if present it is very concerning as it is associated with high rates of fetal morbidity and mortality.1
A sinusoidal CTG pattern has the following characteristics:
- A smooth, regular, wave-like pattern
- Frequency of around 2-5 cycles a minute
- Stable baseline rate around 120-160bpm
- No beat to beat variability
A sinusoidal pattern usually indicates one or more of the following:
- Severe fetal hypoxia
- Severe fetal anaemia
- Fetal/maternal haemorrhage
Overall impression
Once you have assessed all aspects of the CTG you need to determine your overall impression.
The overall impression can be described as either reassuring, suspicious or abnormal.3
Overall impression is determined by how many of the CTG features were either reassuring, non-reassuring or abnormal. The NICE guidelines below demonstrate how to decide which category a CTG falls into.3
Reassuring
Baseline heart rate
- 110 to 160 bpm
Baseline variability
- 5 to 25 bpm
Decelerations
- None or early
- Variable decelerations with no concerning characteristics for less than 90 minutes
Non-reassuring
Baseline heart rate
Either of the below would be classed as non-reassuring:
- 100 to 109 bpm
- 161 to 180 bpm
Baseline variability
Either of the below would be classed as non-reassuring:
- Less than 5 for 30 to 50 minutes
- More than 25 for 15 to 25 minutes
Decelerations
Any of the below would be classed as non-reassuring:
- Variable decelerations with no concerning characteristics for 90 minutes or more.
- Variable decelerations with any concerning characteristics in up to 50% of contractions for 30 minutes or more.
- Variable decelerations with any concerning characteristics in over 50% of contractions for less than 30 minutes.
- Late decelerations in over 50% of contractions for less than 30 minutes, with no maternal or fetal clinical risk factors such as vaginal bleeding or significant meconium.
Abnormal
Baseline heart rate
Either of the below would be classed as abnormal:
- Below 100 bpm
- Above 180 bpm
Baseline variability
Any of the below would be classed as abnormal:
- Less than 5 for more than 50 minutes
- More than 25 for more than 25 minutes
- Sinusoidal
Decelerations
Any of the below would be classed as abnormal:
- Variable decelerations with any concerning characteristics in over 50% of contractions for 30 minutes (or less if any maternal or fetal clinical risk factors – see above).
- Late decelerations for 30 minutes (or less if any maternal or fetal clinical risk factors).
- Acute bradycardia, or a single prolonged deceleration lasting 3 minutes or more.
Regard the following as concerning characteristics of variable decelerations:
- Lasting more than 60 seconds
- Reduced baseline variability within the deceleration
- Failure to return to baseline
- Biphasic (W) shape
- No shouldering
Reviewer
Dr Venkatesh Subramanian
Obstetrics & Gynaecology Registrar in London
References
- AMIR SWEHA, M.D. Interpretation of the Electronic Fetal Heart Rate During Labor. Am Fam Physician. 1999 May 1;59(9):2487-2500. Available from: [LINK].
- Clinical obstetrics and gynaecology. 2nd Edition. 2009. B.Magowan, Philip Owen, James Drife.
- Intrapartum care for healthy women and babies: NICE guideline CG190. Available from: [LINK].




