- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Assessing growth is a key component of the paediatric exam. The measurement of height, length, weight and head circumference appears deceptively simple but requires accuracy, adaptability of method and patience to ensure it is done correctly.
With all children, don’t expect to follow a pre-defined order. Be creative and playful, making the examination into a game involving parents, siblings and the toys available to you.
Introduction
Introduce yourself to the parents and the child, including your name and role.
Confirm the child’s name and date of birth.
Explain what the growth assessment will involve and explain why the measurement is required: “Today I’d like to measure your child’s height (or length), weight and head circumference, which will involve the use of scales, a standing ruler (or measuring board – as appropriate) and a tape measure.”
Gain consent from the parents/carers and/or child before proceeding: “Are you happy for me to carry out the assessment?”
Wash your hands.
Length/height measurement
Children less than 2 years old should be measured supine (lying down, facing upwards).
Children unable to stand, or who find standing difficult, due to illness/physical disability should also be measured supine.
If the child is known to have one leg shorter than the other, they should be measured standing on the longest leg. They should always be measured on the same leg.
The following should be removed:
- Shoes
- Hair clips and braids (undo braids)
- Orthopaedic braces
Supine length
Preparation
Two people are generally required to measure a child when supine.
Play and distraction techniques may be useful to keep the child comfortable and entertained during what can be a distressing moment of measurement.
An appropriate measuring board/rollameter should be placed on a firm and flat surface.
Measurement of supine length
1. Lay the child on the board.
2. One person should ensure the head is supported (in contact with the headboard) and is in the correct position (the corner of the eyes horizontal to the middle of the ear – looking straight up at the ceiling). This is a great job for the parent/carer, helping to also minimise distress for the child being held in this position.
3. The other person should position the child:
- Feet together
- Heels touching the backplate of the measuring instrument
- Legs straight and in alignment with the body
- Buttocks against the backboard
- Scapula against the backboard if possible
- The ankles should be supported, and this position maintained
4. Record the measurement to the last complete millimetre. Don’t round up or down.
Standing height
Preparation
The positioning of the child/young person is crucial for the accurate measurement of height.
It is often helpful to involve the parent/carer in the measurement of the child to aid in positioning.
An appropriate stadiometer (standing ruler) should be used, with an accompanying 500-gram beanbag to weight the headboard.
Measuring standing height
1. The measurer should be performed at a level that is eye to eye with the child.
2. The child should be positioned with:
- Their feet together and flat on the ground
- Heels touching the backplate of the measuring instrument
- Legs straight
- Buttocks and scapula against the backboard
- Arms loosely by their side
3. The child’s head should be positioned with the corners of their eyes horizontal to the middle of the ear, looking straight ahead.
4. The weighted headboard should be placed carefully on the child’s head.
5. Hold the child’s mastoid processes to ensure they are in the correct position.
6. Ask the child to take a ‘big breath in’ and maintain pressure on the mastoids.
7. Ask the child to ‘breath out normally’ and exert upward pressure on their mastoid processes. Ensure their feet and heels remain on the ground. Don’t lift or overextend the child.
8. Once the child has fully exhaled, record the measurement to the last complete millimetre. Read at eye level. Don’t round up or down.
NB. Sitting height or Crown-rump length may also be required in some children. See the ‘Further reading’ section below for appropriate measurement guides.
Weight assessment
Preparation
A child is weighed naked up to 2 years old. Appropriate baby scales should be used (ensure the nappy is removed).
After 2 years of age, light clothes only should be worn. Shoes or slippers should be removed and pockets emptied of their contents.
Appropriate sitting or stand on scales should be used.
If the child is weighed with additional equipment (i.e. splint/cast, medical equipment or dressing), this should be documented.
Measurement
As with height/length, it is often easier if two people are involved in the process of weighing a child. This may include the parent/carer if they are willing to assist.
Again, play and distraction techniques may be useful throughout the measurement of weight.
If appropriate, ask the parent/carer to place the child on suitable scales. The child must be placed completely on the scales and their weight fully borne.
For a distressed child, the carer can be asked to stand on the standing scales, the scales then zeroed with the carer still standing on them, and the child handed to the parent. The scale should then show the child’s weight.
Alternatively, the child can be measured with the carer on sitting scales. The weight of the carer with the child should be measured, then the carer’s weight subtracted.
Record the figure on the scale to the last complete gram for neonates or children <4kg and to the last 100g for older children or if >4kg. Do not round the measurement up or down.
The child should then be redressed and left comfortable.
Further information:
- RCPCH video example of measuring weight
- RCPCH video example of measuring weight in a distressed child

Head circumference measurement
A Lasso-o™ is the recommended equipment used to measure head circumference as per RCPCH guidelines.
The child’s hairstyle should allow for accurate measurement (i.e. remove plaits or braids and remove any hair adornments). If these are not removed – this must be documented.
Measurement
Preparation
Again, play and distraction techniques may be useful throughout the measurement process.
Before using the measuring tape:
- Consider the general clinical condition (e.g. is the child irritable or vomiting).
- Observe the state of the fontanelle (open, closed, full, tense, soft or dipped).
- Note the shape of the child’s head (i.e. craniosynostosis, or a low hairline, e.g. Saethre-Chotzen syndrome).
Measurement of head circumference
1. Loop the Lasso-o™ and place over the child’s head.
2. The tape should be placed above the ears and midway between the eyebrows and the hairline, to the occipital prominence at the back of the head (the aim is to measure the largest circumference possible).
3. Pull the Lasso-o™ or measuring tape taut so that any hair is compressed.
4. Read the measurement from the appropriately marked place. This should be taken to the nearest millimetre.
5. Repeat the procedure above to ensure the accuracy of the measurement.
If the child does have an abnormally shaped head, the tape should be placed over the largest measurable circumference. This should be documented against the recorded measurement.
A separate head circumference chart is available for children with achondroplasia and trisomy 21.

To complete the assessment…
Explain to the child and parents that the assessment is now finished.
Ensure the child is re-dressed after the examination.
Thank the child and parents for their time.
Explain your findings to the parents.
Ask if the parents and child (if appropriate) have any questions.
Wash your hands.
Report/record findings on an appropriate growth chart and calculate growth centiles (see the Growth Chart Documentation guide for further instructions on appropriate documentation).
Reviewer
Dr Sunil Bhopal
Senior Paediatric Registrar
References
Text references
- Southern, L (2017). Height: measuring a child/young person. Clinical Guidelines – Great Ormond Street Hospital for Children NHS Foundation Trust. Accessed 28 March 2019. [LINK]
- Southern, L (2017). Weight: measuring a child/young person. Clinical Guidelines – Great Ormond Street Hospital for Children NHS Foundation Trust. Accessed 28 March 2019. [LINK]
- May, L (2017). Head circumference: measuring a child. Clinical Guidelines – Great Ormond Street Hospital for Children NHS Foundation Trust. Accessed 28 March 2019. [LINK]
Image references
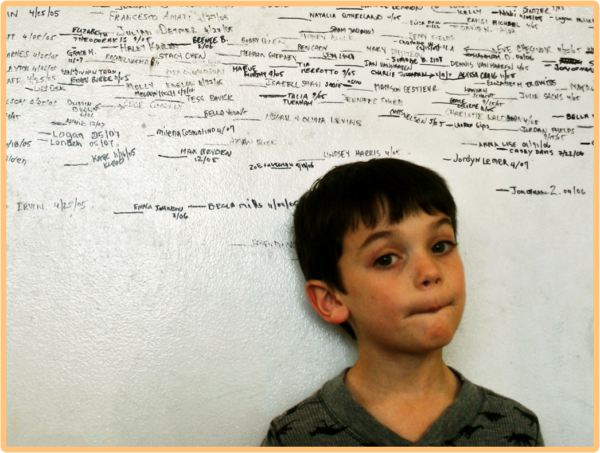
- “Measuring up” (CC BY 2.0) by woodleywonderworks
- “Seven Pounds, Eleven Ounces” (CC BY-ND 2.0) by mikeporcenaluk
- “Checking the circumference” by Stephanie Mancha, Air Force Medical Service Photos is licensed under CC BY 2.0




