- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Sputum sample collection involves the collection of expectorated secretions from a patient’s lower respiratory tract for the purpose of isolating microorganisms.
This guide provides an overview of collecting a sputum sample in an OSCE setting.
Gather equipment
In order to obtain a sputum sample you will need to gather the following equipment:
- Sputum specimen container
- Biohazard bag for delivery of the specimen to the laboratory
- Tissue paper for the patient to clear away any secretions
- Sputum sample microbiology request form
- Gloves and apron (if the patient is suspected of having tuberculosis or other serious infectious diseases, you will need to wear full personal protective equipment including a mask, gown and goggles).
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
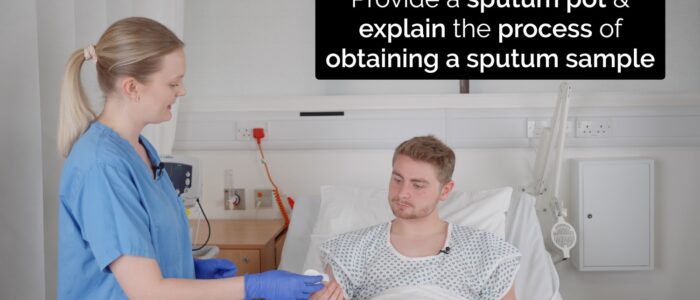
Briefly explain what the procedure will involve using patient-friendly language: “Today I need to collect a sputum sample to provide more information about which bugs are causing your current chest infection. The procedure will involve asking you to cough up a sample of sputum into a sample pot.”
Gain consent to proceed with the sputum sample collection.
Ask the patient if they have any pain before continuing with the clinical procedure.
Position the patient sitting comfortably on a chair or bed.
Collecting the sputum sample
1. Confirm the patient’s details by asking them to tell you their name and date of birth (compare these details to the patient’s wristband if present).
2. Ask the patient to sit upright if they are able to.
3. Advise the patient to breathe in and out deeply several times and then perform a series of coughs to produce a sputum sample into the specimen container.
4. Collect 1-2 teaspoons of sputum in the specimen container and then seal the lid.
5. Ensure the patient is comfortable after the procedure and check their vital signs are stable.
6. Label the specimen container at the patient’s bedside with the relevant details.
7. Complete the microbiology request form, including the relevant clinical details (e.g. current symptoms, recent investigation results and past medical history).
8. Place the sputum sample container and microbiology request form in a specimen bag and transport to the laboratory for analysis (e.g. culture and sensitivity, viral PCR).
9. Remove your personal protective equipment and place into a clinical waste bin.
To complete the procedure…
Explain to the patient that the procedure is now complete.
Thank the patient for their time.
Offer the patient paper towels to clean away any secretions.
Dispose of PPE appropriately and wash your hands.
Document the details of the procedure in the patient’s notes including the appearance of the sputum.
Reviewer
Nicky Milner
Biomedical Scientist
Editor
Hannah Thomas
References
- Smith SF, Duell DJ, Martin BC. Clinical nursing skills. Published in 2011. Available from: [LINK].
- Blakeborough L, Watson JS. The importance of obtaining a sputum sample and how it can aid diagnosis and treatment. British Journal of Nursing. Published in 2019. Available from: [LINK].
- New South Wales (NSW) health. Sputum induction guidelines – Tuberculosis. Published in 2018. Available from: [LINK].
- Shepherd E. Specimen collection 4: procedure for obtaining a sputum specimen. Published in 2020. Available from: [LINK].
- Eccles S, Pincus C, Higgins B, Woodhead M. Diagnosis and management of community and hospital-acquired pneumonia in adults: summary of NICE guidance. Published in 2014. Available from: [LINK].