- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
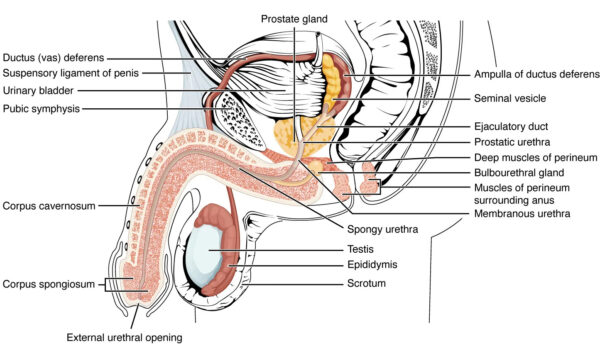
The male reproductive system spans the abdominal, pelvic, and perineal regions. This article describes the anatomy of the scrotum, including the testes, epididymis, and spermatic cord, and will focus on definitions, anatomical structure, innervation and blood supply.
The scrotum
The male reproductive system includes the scrotum, which contains three major paired structures:1
- The testes
- Epididymis
- Spermatic cord
The layers of the scrotum are continuations of the abdominal wall layers, and from superficial to deep, the layers are:2
- Skin
- Dartos fascia and muscle
- External spermatic fascia
- Cremasteric fascia
- Internal spermatic fascia
- Tunica vaginalis
- Tunica albuginea
Tip: A useful mnemonic to remember these is ‘Some Damn Englishman Called It The Testis’
Structures
Testes
The testes are paired male sex glands located within the scrotum.
They are oval-shaped and attached to the scrotum by the scrotal ligament. Each testis is surrounded by the double-layered tunica vaginalis. Deep to this layer is the tunica albuginea, a fibrous capsule that encloses the testicle and epididymis.3
The tunica albuginea also projects internally to form compartments within the testis, which are divided by septa. Each septum separates the seminiferous tubules (Sertoli cells present here) and the interstitial tissue (Leydig cells present here).
The seminiferous tubules are the site of germ cell production. These looped tubules are continuous at their ends with the rete testis, a network of collecting tubes that eventually coalesce to form efferent ducts that provide a conduit for collecting the testicular fluid and spermatozoa to the epididymis.
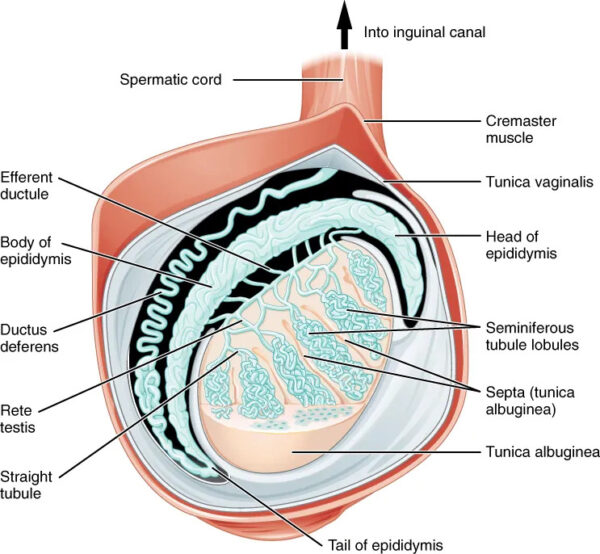
Epididymis
The epididymis is a coiled duct and divided into three parts:5
- Head: this is the most proximal part of the epididymis and transports sperm from the testes to the epididymis
- Body: the heavily coiled duct of the epididymis
- Tail: this is the most distal part of the epididymis and marks the start of the vas deferens, which transport sperm to the urethra for ejaculation
Spermatic cord
The spermatic cord is a collection of vessels, nerves and ducts formed at the opening of the inguinal canal.
It is located laterally to the inferior epigastric vessels and passes through the inguinal canal and into the scrotum via the superficial inguinal ring. It continues into the scrotum and ends at the posterior border of the testes.6
Contents of the spermatic cord
The spermatic cord contains:
- Vessels: testicular artery, cremasteric artery and vein, artery to the vas deferens and the pampiniform plexus of testicular veins.7
- Nerves: genital branch of the genitofemoral nerve and autonomic nerves.8
- Additional structures: the vas deferens also lies within the spermatic cord, and transports sperm from the epididymis to the urethra in preparation for ejaculation.9
Blood supply
The testes and epididymis are supplied by paired testicular arteries, which directly arise from the abdominal aorta.
The testicular arteries descend the abdomen and pass into the scrotum via the inguinal canal. They are contained within the spermatic cord.
In addition to the testicular arteries, the testes are supplied by branches of the cremasteric artery and the artery of the vas deferens.10 The cremasteric artery arises from the inferior epigastric artery, and the inferior vesical artery gives rise to the artery of the vas deferens. These two arteries give anastomoses to the main testicular artery.11
Innervation
The innervation of the scrotum is derived from branches of the genitofemoral, pudendal, posterior femoral cutaneous, and ilioinguinal nerves.
The anterior aspect of the scrotum receives cutaneous innervation from the anterior scrotal nerves, derived from the genital branches of the genitofemoral nerve and ilioinguinal nerve.2
The posterior aspect of the scrotum is supplied by the posterior scrotal nerves, which are branches of the pudendal nerve and the posterior femoral cutaneous nerve.2
Clinical relevance – Scrotal swelling
Scrotal swelling can be caused by several causes, depending on the structure affected:12
- Hydrocele: a collection of serous fluid between the parietal and visceral layers of the tunica vaginalis. It can be congenital, caused by failure of the tunica vaginalis to close, creating a space where fluid can accumulate. Hydroceles can also occur because of infection, injury or malignancy.
- Haematocele: a collection of blood in the tunica vaginalis and can be distinguished from a hydrocele by transillumination. The dense nature of blood means light is unable to pass through.
- Varicocele: enlargement of the pampiniform venous complex. The plexus of veins drains blood from the testicles. The left testicle is more commonly affected as the left testicular vein is longer and drains into the left renal vein at a perpendicular angle. Varicocele has an estimated prevalence of 15-20% in the general population and can look and feel like a ‘bag of worms’ within the scrotum.
- Epididymitis: inflammation of the epididymis and is usually caused by bacterial or viral infection
Reviewer
Mr Chaitya Desai
Urology Registrar
Editor
Dr Chris Jefferies
References
- OpenStax. Testicular Reproductive System. License: [CC BY]
- Patel, A.P., Anatomy and physiology of chronic scrotal pain. Transl Androl Urol, 2017. 6(Suppl 1): p. S51-S56.
- Kühn, A.L., et al., Ultrasonography of the scrotum in adults. Ultrasonography, 2016. 35(3): p. 180-97.
- OpenStax. Anatomy of the Testis. License: [CC BY]
- Mital, P., B.T. Hinton, and J.M. Dufour, The blood-testis and blood-epididymis barriers are more than just their tight junctions. Biol Reprod, 2011. 84(5): p. 851-8.
- Köckerling, F. and C. Schug-Pass, Spermatic Cord Lipoma-A Review of the Literature. Front Surg, 2020. 7: p. 39.
- Dagur, G., et al., Neoplastic diseases of the spermatic cord: an overview of pathological features, evaluation, and management. Transl Androl Urol, 2017. 6(1): p. 101-110.
- Pankhania, M. and S. Ali, The genitofemoral nerve block: a method for hemiscrotal anaesthesia at the bedside. Ann R Coll Surg Engl, 2012. 94(4): p. 272.
- Koslov, D.S. and K.E. Andersson, Physiological and pharmacological aspects of the vas deferens-an update. Front Pharmacol, 2013. 4: p. 101.
- Key, R. Doppler Imaging of the Scrotum. 2016 [cited 2023 20/10/23]; Available from: [LINK]
- Benzi, T.C., et al., Testicular arteries anatomy applied to fowler-sthephens surgery in high undescended testis – a narrative review. Int Braz J Urol, 2022. 48(1): p. 8-17.
- Davis, J.E. and M. Silverman, Scrotal emergencies. Emerg Med Clin North Am, 2011. 29(3): p. 469-84.




