- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Being able to share information in a clear and concise way is an essential skill in all fields of medicine. This can range from simple explanations, such as why a blood test may be needed, to more complex situations, such as explaining a new diagnosis. Often, sharing information with a patient occurs naturally during a consultation. However, providing clinical information may also be the primary focus of an appointment, and in these situations, it is crucial to have a structured format in order to communicate more effectively.
This guide provides a step-by-step approach to explaining a diagnosis of acne vulgaris. You should also read our overview of how to effectively communicate information to patients.
Structuring your explanation
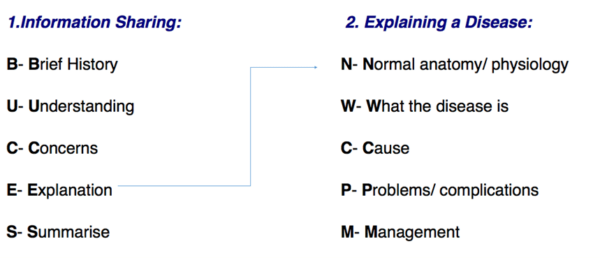
Explaining a diagnosis requires structure and adequate background knowledge of the disease. Whether the information being shared is about a procedure, a new drug or a disease, the BUCES structure (shown below) can be used.
Opening the consultation
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
BUCES can be used to remember how to structure a consultation in which providing information is the primary focus. Before explaining the various aspects of a disease, it is fundamental to have a common starting point with your patient. This helps to establish rapport and creates an open environment in which the patient can raise concerns, ask questions and gain a better understanding of their problem. After introducing yourself, it is important to take a brief history (this is the first part of the BUCES structure):
- What has brought the patient in to see you today?
- What are their symptoms?
- Are there any risk factors that can be identified? (e.g. lifestyle/family history)
For example, a patient with acne vulgaris will likely mention areas such as the face, chest and upper back being affected, and will report symptoms such as pustules and redness. They will also potentially mention exacerbating factors such as cosmetic use or medications such as steroids.
Tip: Practice taking concise histories to get the timing right. In OSCE stations, timing is crucial and you do not want to spend all your time taking a history when you are meant to be explaining a diagnosis! A rough guide would be to keep the introduction and brief history between 1-2 minutes maximum.
What does the patient understand?
Following a brief history, it is important to gauge the patient’s knowledge of their condition. Acne vulgaris is very common amongst teenagers (80-90% are affected) and so patients will likely know someone else with the condition. This means that they may have a very good understanding of the condition and the ways it might be managed. On the other hand, this may be their first experience of the condition, particularly if they are in early adolescence.
Due to these reasons, it is important to start with open questioning. Good examples include:
- “What do you think is causing your symptoms?”
- “What do you know about acne?”
- “What has been explained to you about acne so far?”
Open questioning should help you to determine what the patient currently understands, allowing you to tailor your explanation at an appropriate level.
At this stage, primarily focus on listening to the patient. It may also be helpful to give positive feedback as the patient talks (i.e. should a patient demonstrate some understanding, reinforce this knowledge with encouraging words and non-verbal communication such as nodding).
Checking the patient’s understanding should not be solely confined to this point of the consultation but should be done throughout by repeatedly ‘chunking and checking’.
Tip: Try using phrases such as: “Just to check that I am explaining acne clearly, can you repeat back to me what you understand so far?”. This is far better than only saying “What do you understand so far?” as the onus is placed upon the quality of your explanation rather than there being an issue with the patient’s ability to understand.
What are the patient’s concerns?
The patient’s concerns should never be overlooked. While acne itself is not necessarily harmful it can have a significant psychological impact, particularly if the patient is of school age. Asking the patient if they have any concerns before beginning your explanation allows you to specifically tailor what is most relevant to the patient, placing them at the centre of the explanation. The “ICE” (ideas, concerns and expectations) format, can provide a useful structure for exploring this area further.
ICE
Ideas:
- What does the patient think is causing their symptoms?
- What is their understanding of the diagnosis?
Concerns:
- What are the patient’s concerns regarding their symptoms and diagnosis?
Expectations:
- What is the patient hoping to get out of the consultation today?
Explanation
After determining the patient’s current level of understanding and concerns, you should be able to explain their condition clearly. For more information on acne, see the Geeky Medics guide to acne vulgaris.
You should begin by signposting what you are going to explain to give the patient an idea of what to expect.
“I’m going to begin by talking about the normal function of the skin and then move on to discuss what acne is, what causes it and how we can manage it together.”
Tip: Use the mnemonic “Normally We Can Probably Manage” to help you remember the structure of explaining a disease.
Normal anatomy/physiology
“The normal function of the skin is to act as a barrier. We can imagine the skin to be layers of bricks stacked on top of each other. In normal skin, there are glands that produce an oily substance called sebum which helps maintain and protect the skin. In acne, there is too much sebum produced which leads to spots.”
What the disease is
Acne is a disease of the pilosebaceous unit (hair follicle and associated sebaceous gland). Increased sebum production from these glands leads to the development of comedones, papules and pustules on the skin. It is very common in teenagers and affects 80% of 13-18-year-olds.
It most commonly affects the face, chest and upper back, but can affect any area of the skin where sebaceous glands are present. The most common form of acne is acne vulgaris (the form typically affecting teenagers), however, there are other types such as infantile acne and adult acne.
Mild acne tends to present with comedones, which are blocked hair follicles. Closed comedones are also known as “whiteheads” and open ones are known as “blackheads”.
More severe acne can present with papules and pustules on the skin or even the formation of cysts in severe cases. Once the lesions have healed there can be leftover scarring or changes in the pigmentation of the skin.
Cause of the disease
“Acne is a problem with the hair follicles and their associated glands in the skin. These glands produce an oily, waxy substance called sebum. In some people, these glands produce more sebum than normal, which leads to spots on the skin – this is known as acne. It is very common in teenagers, with around 80% having acne at some point.”
“There are a few different things that can cause the skin to produce too much sebum, one is changes in sex hormones – which happens when people go through puberty. This can also explain why patients who menstruate have symptoms that vary throughout the menstrual cycle.”
“Some other things that can cause or worsen acne include certain bacteria on the skin, medications like steroids or the glands being blocked by things like make-up.”
Problems/complications
Outlining potential complications of acne is necessary so that the patients can identify problems early and seek medical advice. Being aware of common problems will also encourage patients to adhere to their treatment.
The most common complication of acne is post-inflammatory lesions. These include scarring, hyperpigmentation and keloid scars and can persist long after the initial lesion has healed. Some treatments are available for acne scarring, such as fillers or laser therapy.
It is also important to be aware of the potential mental health implications of acne. It can often lead to feelings of self-consciousness and low self-esteem in patients and can contribute to depression and anxiety.
“Sometimes once the spots have healed you can be left with scarring on the skin or changes to the normal colour of the skin. This is why it’s important to try and treat acne well. But if you do develop these problems there are potential treatments available.”
“Acne can also often make people feel self-conscious or worried about their appearance. If this is happening to you then it’s really important that you talk to someone about it.”
Management
Reinforce to the patient that they need to work with you as a team to achieve a good result.
Patients should be advised to avoid any exacerbating factors/triggers that they have identified and to try to avoid picking or scratching at the lesions.
Topical therapies
Most patients with mild to moderate acne can be managed with topical therapy.
Some of these are available over-the-counter without a prescription, such as salicylic acid and benzoyl peroxide. Salicylic acid is present in several cleansers and skincare products, and benzoyl peroxide is available as a gel or face wash.
If these are ineffective alone then a patient can be prescribed a topical retinoid, which helps to inhibit sebum production. It is important to warn patients that these can be quite drying, so it may be best to try using them on alternate days if their skin becomes irritated. Even though it is topical it is still considered teratogenic, so should not be prescribed to patients who are trying to conceive, are pregnant or breastfeeding.
Systemic therapies
If topical therapies fail to improve symptoms then there are several systemic treatments that can be prescribed for moderate to severe acne.
Patients assigned female at birth can be prescribed anti-androgenic options. The first of these is the oral contraceptive pill (OCP). While this can be very effective it can take 6 months for a benefit to be seen and it is important to tell patients this. Another option is spironolactone, although this is less commonly prescribed and is contraindicated in pregnancy.
Sometimes oral antibiotics (usually tetracyclines or erythromycin) can be used. They are prescribed at low doses and have an anti-inflammatory effect on the skin.
Isotretinoin
If the above options fail or the acne is severe then patients can be referred to dermatology to consider isotretinoin.
This is a very effective treatment and is generally indicated if acne is persistent, treatment-resistant, cystic or scarring. It may induce remission in some patients.
It should only be prescribed in specialist settings, however, as it can have significant side effects, such as mucosal dryness, sensitivity to the sun and potential mental health issues. Patients also need to have their cholesterol and LFTs monitored while taking isotretinoin and again, it is considered teratogenic.
Example of how you might explain the management of acne
“Acne can be really unpleasant to live with so it’s important we try and get it under control.”
“We can start out by trying some topical creams, you can get some of them over-the-counter. One is called salicylic acid and it’s available in a lot of skin cleansers – this helps to unblock the glands in your skin. Another is called benzoyl peroxide, which you can buy in pharmacies. This helps with any bacteria on your skin that might be causing your acne. You can use these every day to cleanse and wash your skin.”
“As you have some signs of moderate acne I’ll also prescribe you something called a topical retinoid to use as well. This helps reduce the amount of sebum your skin makes and because of this it can be quite drying. So try using it every other day at first and see how you get on with it.”
“If these don’t work or your acne gets worse then come back and there are some tablets that we can try that often help and if we’re really struggling then we can refer you to the skin specialists for some more options.”
Closing the consultation
Summarise the key points back to the patient.
“In summary acne is a problem with the glands in the skin producing too much sebum so they get blocked and cause spots to develop. You might notice certain things like make-up make things worse and if so you should try to avoid this and try to avoid picking at the spots as this can lead to scars. We’ll start off with some topical treatments and see if they help, but if not then you can book another appointment and we can try some tablets that might help a bit more.”
Ask the patient if they have any questions or concerns that have not been addressed.
“Is there anything I’ve explained that you’d like me to go over again?”
“Do you have any other questions before we finish?”
Arrange appropriate follow-up to discuss their acne further. Acknowledge that you have discussed a large amount of information and it is unlikely that they will remember everything.
Offer the patient some leaflets on acne and its management, and direct them to some reliable websites which they can use to gather more information (examples include patient.info and the BAD)
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
References
- British Association of Dermatologists. Handbook for Medical Students and Junior Doctors. 2020. Available from: [LINK]
- DermNet NZ. Acne. 2014. Available from: [LINK]
- Patient.info. Acne Vulgaris. 2021. Available from: [LINK]
- Patient.info. Acne. 2021. Available from: [LINK]
- British Association of Dermatologists. Acne PIL. 2020. [LINK]