- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Eyelid disorders are a common presenting complaint in primary care. Although most eyelid conditions can be managed conservatively, some risk sight loss and require referral to ophthalmology.
Eyelids comprise skin, muscle, connective tissue, glands and conjunctiva. They have an important role in preventing the eye from drying out and help protect the eye from foreign bodies and excessive light.
Meibomian glands are in the posterior aspect of the eyelid (Figure 1). They are modified sebaceous glands that produce the lipid outer layer of the tear film. The lacrimal puncti are responsible for tear drainage and are on the medial aspect of each eyelid.
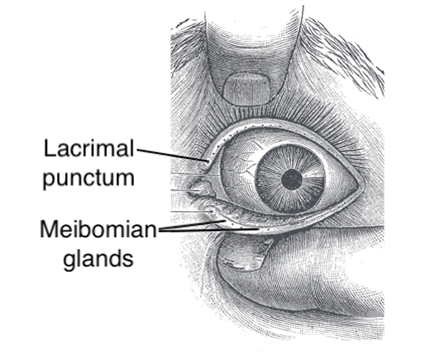
Eyelashes are in the anterior aspect of the eyelid and help prevent foreign bodies from entering the eye. Each eyelash follicle is associated with sweat and sebaceous glands.
Blepharitis
Blepharitis is inflammation of the eyelid. It is the most common cause of dry eye disease and accounts for 5% of ophthalmology-related presentations in primary care.2
Patients typically present with bilateral symptoms of ocular irritation, foreign body sensation, burning, redness and crusting. There may be paradoxical watering of the eye due to reflex tear secretion.
Although the exact aetiology of blepharitis is unclear, the underlying disease process involves congestion and inflammation of eyelash follicles and meibomian glands. Blepharitis often has multiple causative factors.
Causes of blepharitis include:
- Atopic dermatitis (staphylococcal)
- Seborrheic dermatitis
- Acne rosacea
- Demodex infestation (mites)
Blepharitis commonly presents with appears as erythematous and thickened eyelid margins. The base of eyelashes may reveal crusting (Figure 2). and matting. Immediately posterior to the eyelashes, yellow ‘capping’ of meibomian gland orifices may be seen.
Lid hygiene is important for treating and preventing blepharitis.
There are three steps to cleaning eyelids that should be performed at least once a day:
- Warm compression of the eyelids with a warm compress to loosen debris
- Eyelid massage to empty glands of debris
- Cleaning eyelids with cotton wool to remove debris
Topical antibiotic ointments (e.g. chloramphenicol) can be applied to the eyelid margin for a few weeks to reduce bacterial colonisation.
An extended course of low-dose oral tetracyclines and regular omega-3 fatty acid supplements may have a useful anti-inflammatory effect.
Hordeolum
An external hordeolum is caused by a staphylococcal infection of an eyelash follicle. External hordeolum tend to affect children and young adults and are also known as a stye.
An internal hordeolum is an infection of a meibomian gland and is far less common.
External hordeola present as tender, red eyelash follicle swellings (Figure 4).

Hordeola often resolve spontaneously. Patients should be encouraged to perform warm compression of the eyelid multiple times a day to reduce swelling.
Other treatment options include:
- Removal of the eyelash associated with external hordeolum
- Incision of the hordeolum with a fine sterile needle
- Topical antibiotics (e.g. chloramphenicol) or oral antibiotics (e.g. co-amoxiclav) if the hordeolum is recurrent or severe
Chalazion
A chalazion is a granulomatous inflammatory lesion that forms in an obstructed meibomian gland.
Unlike hordeola, chalazion are non-infectious. Chalazion are often associated with blepharitis and acne rosacea.
Chalazia present as painless red eyelid cysts in the internal eyelid (Figure 5). If chalazia are infected, they become internal hordeolum.
A chalazion and external hordeolum can be easily distinguished as chalazia are not painful or tender to touch. In contrast, an external hordeolum is associated with pain (i.e. ‘styes sting’).
Chalazia often resolve spontaneously. Patients should be encouraged to perform warm compression of the eyelid (to loosen meibomian gland content) and eyelid massage (to express meibomian gland content) twice a day.
A persistent chalazion requires referral to ophthalmology for consideration of incision and curettage.
Entropion
Entropion is inward turning of the eyelid. Inward-turning eyelashes may irritate the cornea causing ulceration and risking sight loss.
The most common cause is age-related degenerative changes to the lower eyelid. Entropion can also be caused by eyelid irritation or scarring. Trachoma (a bacterial eye infection caused by Chlamydia trachomatis) is a common cause of entropion in places that have limited access to sanitation and water.
The management of entropion includes:
- Examination for corneal abrasions and ulcers (keratitis)
- Patients should be prescribed frequent lubricants to reduce the risk of corneal abrasions and advised on how to perform eyelid taping as a temporising measure
- Referral to ophthalmology for surgical correction
Ectropion
Ectropion is an outward turning of the eyelid.
Ectropion is mostly caused by age-related degenerative changes to the lower lid and presents with a sore red eye. The eye is often watery due to disrupted tear drainage.
Another common cause is facial nerve palsy (Bell’s palsy) which concurrently causes incomplete upper eyelid closure. This is a risk factor for the development of exposure keratopathy, which is damage to the cornea due to ocular dryness caused by inadequate lid closure.8 Exposure keratopathy can cause sight loss.
The management of ectropion is typically conservative with lubricating eye drops and taping the eyes shut at night. Severe cases may require corrective surgery.
Patients should be referred to ophthalmology urgently if there are any features of exposure keratopathy (clinical features are similar to a corneal abrasion).
Trichiasis
Trichiasis is when eyelashes grow inwards due to damaged eyelash follicles. Inward-growing eyelashes may irritate the cornea causing corneal ulceration and risking sight loss.
Most cases of trichiasis are caused by eyelid inflammation (chronic blepharitis).
When assessing trichiasis, it is important to examine for evidence of corneal damage.
Trichiasis can be treated by epilating the eyelash however recurrence may occur within a few weeks. Electrolysis or laser ablation can destroy the lash follicle and may provide a more permanent solution.
Key points
- Eyelids comprise skin, muscle, connective tissue, glands and conjunctiva.
- Blepharitis is inflammation of the eyelid and presents with bilateral sore, gritty eyes.
- An external hordeolum (style) is caused by a staphylococcal infection of an eyelash follicle.
- A chalazion is a granulomatous inflammatory lesion of an obstructed meibomian gland.
- Blepharitis, hordeolum and chalazion can often be treated conservatively with eyelid hygiene.
- Entropion and trichiasis can cause corneal ulceration, which can lead to sight loss.
- Ectropion can cause exposure keratitis, which can result in sight loss.
- Any indication of risk to cornea or risk of sight loss requires referral to ophthalmology.
Reviewer
Dr Sahib Tuteja
Opthalmology trainee
Editor
Dr Chris Jefferies
References
- Henry Vandyke Carter (modified by Jonathan Malcolm). Eyelid anatomy. License: [Public domain]. Available from: [LINK]
- NICE CKS. Blepharitis. Published in 2019. Available from [LINK]
- Clubtable (Wikipedia user). Blepharitis. License: [Public domain]. Available from: [LINK]
- Imran Kabir Hossain. Anterior blepharitis. License: [CC BY-SA]. Available from: [LINK]
- Andre Riemann. Hordeolum externum. License: [Public domain]. Available from: [LINK]
- Michal Klajban. Chalazion. License: [CC BY-SA]. Available from: [LINK]
- Poupig (Wikipeida user). Chalazion. Licence: [CC BY-SA]. Available from: [LINK]
- Wanjiku Mathenge. Emergency management: Exposure keratopathy. Published 2018. Available from: [LINK]
- Mary Lowth. Chalazion. Published in 2016. Available from: [LINK]
- Mary Lowth. Conditions Affecting the External Eye. Published in 2016. Available from: [LINK]
- Mary Harding. Blepharitis. Published in 2014. Available from: [LINK]
- Mostafa Khalil, Omar Kouli. The Duke Elder Exam Of Ophthalmology: A Comprehensive Guide for Success. Book published in 2020.
- The College of Optometrists. Clinical Management Guidelines. Published in 2018-2020. Available from: [LINK]








