- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Keratitis or corneal ulcer refers to sight-threatening infection and inflammation of the cornea.
Bacterial and viral keratitis represent the most common forms of microbial keratitis, but rarely the cause may be fungal or protozoan (acanthamoeba).
The following article aims to provide an overview of microbial keratitis at the level expected of final-year medical students and foundation doctors.
Bacterial keratitis
Aetiology
The corneal epithelium forms the primary barrier to microbes and the tear film on the corneal surface contains immunoglobulins and other antimicrobial compounds.
Most cases of bacterial keratitis are caused by Staphylococcus, Streptococcus and Pseudomonas species in patients with a disrupted corneal epithelium.
However, Neisseria gonorrhoeae, Neisseria meningitides, and Corynebacterium diphtheria can penetrate an intact epithelium.
Infections may be polymicrobial (e.g. bacterial and fungal co-infection).
Risk factors
Risk factors for bacterial keratitis are those which disrupt the healthy corneal epithelium. These include:
- Contact lens wear: most common risk factor, especially in prolonged use and poor lens hygiene
- Corneal trauma: including previous ocular surgery, foreign body, chemical injury
- Ocular surface disease: dry eye, lid malposition, chronic blepharitis
- Immunosuppression: drugs, immunodeficiency syndromes, diabetes
Clinical features
History
Bacterial keratitis commonly causes unilateral symptoms. Typical symptoms may include:
- Ocular pain: this may be moderate or severe and include symptoms of irritation and foreign body sensation
- Red eye
- Reduced visual acuity: this may be near normal to markedly reduced
- Photophobia: intolerance to sunlight or normal room lighting
- Purulent discharge
A history of contact lens wear is essential:
- Type of contact lenses used: daily disposable, monthly or extended-wear
- Duration of wear per day
- If they have ever slept, showered, or swam with their lenses in
For more information, see the Geeky Medics guide to ophthalmic history taking.
Clinical examination
All patients with keratitis (regardless of underlying aetiology) should undergo visual acuity testing with a Snellen chart and anterior segment examination (ideally with a slit lamp, but a direct ophthalmoscope with high magnification or an Arclight can be used).
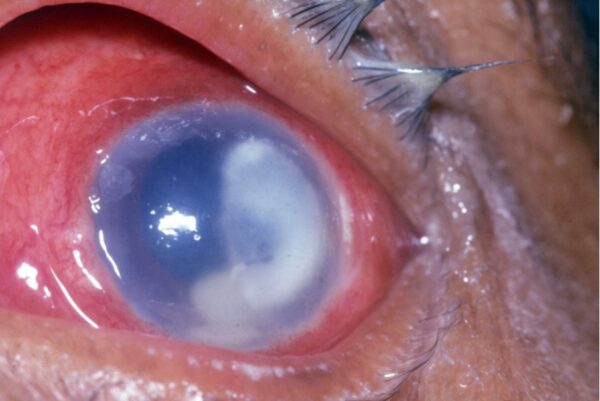
Typical clinical findings may include:
- Lids and lashes: eyelid oedema in moderate to severe cases
- Conjunctiva: pattern of injection may be circumlimbal (around the cornea) or diffuse
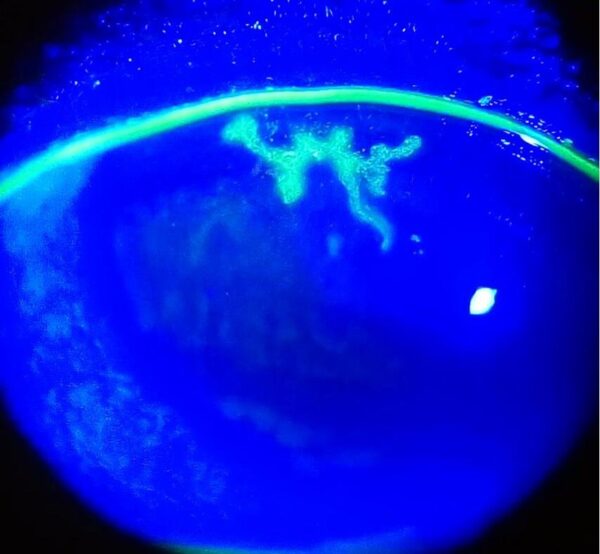
- Cornea: a yellow-white opacity which represents the area of inflammation (infiltrate) with clearly defined margins. The overlying epithelial defect will stain green upon application of 2% fluorescein drops and viewed under blue light.
- Anterior chamber and pupil: hypopyon (pus-level) and posterior synechiae (adhesion between the pupil margin and anterior lens surface) in severe cases
- Pupil assessment for direct and consensual response to light: may show a relative afferent pupillary defect
Investigations
Bacterial keratitis is a clinical diagnosis.
Relevant investigations may include:
- Corneal scrapes and conjunctival swabs: these are performed in severe or treatment-resistant cases to allow identification of the causative organism and determine antibiotic sensitivities
- Contact lenses, cases and solutions should also be sent for culture and sensitivity
Management
Contact lens use should be discontinued immediately.
Antibiotic therapy should be commenced:
- Topical antibiotics: initially with broad spectrum cover (e.g. fluoroquinolone monotherapy or cefuroxime and gentamicin duo therapy) until culture results return. Instillation may be up to hourly for the first 24-48 hours depending on severity, this can then be tapered off given response to treatment
- Oral antibiotics: may be required in severe cases
Surgery (e.g. corneal transplantation) is rarely required, it is considered only in complicated (e.g. perforation) or medically refractory cases.
Complications
Complications of bacterial keratitis include:
- Spread of infection: the infection may spread beyond the cornea into the sclera or within the deeper tissues of the eye, leading to endophthalmitis.
- Corneal perforation in severe cases
- Residual dense corneal scarring
- Irregular astigmatism
- Formation of cataract: secondary lens opacification is common following severe inflammation
The overall visual outcome is very variable and dependent on a number of factors which include the size and depth of the infection, time to diagnosis and initiation of treatment, and compliance with therapy.
Viral keratitis
Herpes simplex epithelial keratitis
Aetiology
Herpes simplex virus (HSV) is a dsDNA virus which has two serotypes: HSV-1 and HSV-2. HSV-1 principally affects the eyes, lips, and face, while HSV-2 causes genital infection with rare ophthalmic involvement.
Primary infection with HSV is usually acquired in childhood and is commonly subclinical or mild with symptoms of blepharoconjunctivitis and upper respiratory tract infections.
Following the resolution of the primary infection, HSV travels through the sensory nerve to the trigeminal ganglion, establishing latency. Subsequent reactivation where the virus replicates and travels back to the periphery, such as the corneal epithelium, results in epithelial keratitis.
Risk factors
Risk factors for herpes simplex virus infection include:
- Primary infection: direct contact with infected secretions or lesions
- Reactivation/ recurrent disease: trauma involving the trigeminal nerve, stress, immunosuppression, previous reactivation
Each attack is associated with a greater risk of recurrence.
Clinical features
Typical symptoms of herpes simplex epithelial keratitis include:
- As with other forms of keratitis: discomfort, grittiness, red eye, reduced visual acuity and photophobia
- Epiphora (watering of the eye) as opposed to purulent discharge seen in bacterial ulcer
- A previous history of cold sores
Typical clinical findings on examination may include:
- Lids and lashes: mild eyelid erythema and oedema
- Conjunctiva: diffuse or circumlimbal injection
- Cornea: dendritic ulcer (pathognomonic sign) with linear branching morphology and terminal bulbs. The bed of the ulcer will stain green with fluorescein, while the ulcer margin will stain with rose Bengal
- Reduced corneal sensation
Investigations
HSV keratitis can be diagnosed clinically with the identification of a dendritic ulcer.
Conjunctival and corneal swabs can be sent for a confirmatory viral PCR. It is however important to investigate other microbial causes of keratitis when the diagnosis is equivocal.
Management
Contact lens use should be discontinued immediately.
Management of HSV keratitis should include:
- Topical antivirals (e.g. aciclovir 3% ointment five times daily for up to two weeks)
- Epithelial debridement: in conjunction with a topical antiviral agent (aims to reduce viral load and promote healing)
- Steroids are contraindicated in active epithelial disease: steroids are only used in close supervision by ophthalmologists to suppress the immune response in cases with corneal stromal involvement
- Patients may need long-term oral antiviral prophylaxis in recurrent disease
Complications
The majority of dendritic ulcers will resolve even without treatment. Prolonged or recurrent disease may result in corneal scarring, glaucoma, and cataracts.
Other forms of HSV keratitis that involve deeper corneal layers require a longer duration of treatment and their prognosis is more variable
Herpes zoster ophthalmicus (HZO)
Herpes zoster ophthalmicus refers to the reactivation of the varicella-zoster virus (shingles) affecting the ophthalmic branch of the trigeminal nerve (V1).
Conjunctivitis and epithelial keratitis occur secondary to direct viral invasion. On examination under fluorescein, small dots (punctate keratitis) or pseudo-dendrites (lacking terminal bulbs, in contrast to HSV keratitis) may be visible on the cornea.
HZO can affect any part of the eye or the orbit with potentially disastrous visual outcomes. For more information, see the Geeky Medics guide to herpes zoster ophthalmicus.
Protozoan and fungal keratitis
Fungal keratitis
Aetiology
Fungal keratitis is an uncommon but aggressive corneal infection.
It is a major cause of visual loss in developing and tropical countries. It is commonly associated with fusarium and aspergillus species (filamentary fungi) in the context of ocular trauma, and candida species (yeasts) in the immunocompromised.
Risk factors
Risk factors for fungal keratitis include:
- Corneal trauma: especially with contamination of organic/agricultural matter
- Contact lens wear
- Immunosuppression: topical steroids, systemic immunosuppression, diabetes
- Ocular surface disease: dry eyes
Clinical features
Typical symptoms of fungal keratitis are similar to other corneal infections. There is a gradual onset of pain, redness, reduced visual acuity, photophobia and epiphora.
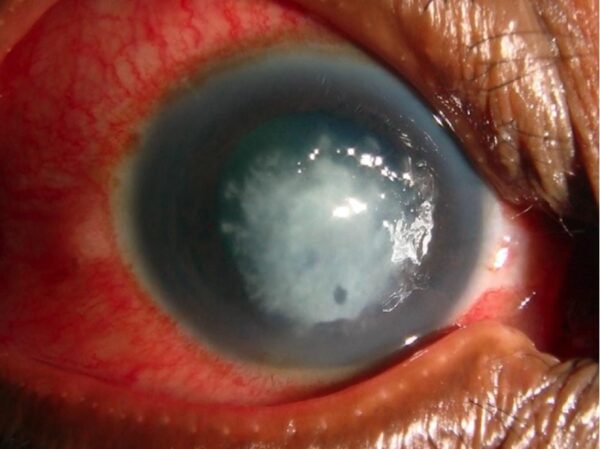
Typical clinical findings on examination may include:
- Lids and lashes: redness and periocular oedema
- Conjunctiva: diffuse injection
- Cornea: grey-white stromal infiltrate with fluffy margins. Satellite lesions may be seen. Rapid progression may occur with necrosis and corneal thinning
- Anterior chamber: inflammation, evidenced by the presence of cells, or hypopyon in severe cases
Investigations
Relevant investigations may include:
- Corneal scraping, performed early, before commencing treatment: for Gram and Giemsa staining and for culture, plated on Sabouraud dextrose agar
- PCR analysis
Management
Contact lens use should be discontinued immediately.
Management of fungal keratitis should include:
- Topical antifungals: hourly installation initially, then tapered according to response
- Systemic antifungals: in severe cases, suspected endophthalmitis and immunocompromised patients
- Oral analgesia and topical cycloplegia for pain management
- Topical steroids should be avoided in the acute phase, but they may be considered during stages of healing
Penetrating keratoplasty (full-thickness corneal transplant) may be required in progressive disease.
Complications
Visual prognosis is generally poor due to the high rate of complications. Recurrence is common following tapering of treatment.
Other complications may include:
- Severe inflammatory response leading to scleritis and endophthalmitis
- Corneal perforation
Acanthamoeba keratitis
Acanthamoeba keratitis is a rare form of microbial keratitis associated with poor visual outcomes.
Aetiology
Acanthamoeba are free-living protozoa commonly isolated from soil, pond, sea, tap water and chlorinated water. In developed countries, the vast majority of patients with acanthamoeba keratitis are contact lens wearers.
Risk factors
Risk factors for acanthamoeba keratitis include:
- Contact lens wear: especially associated with swimming with contact lenses and poor hygiene
- Corneal trauma
Clinical features
Symptoms are variable but may be severe, including reduced visual acuity, pain, redness, foreign body sensation, photophobia, epiphora
Characteristically, pain is severe and disproportionate to relatively mild clinical findings.
Typical clinical findings on examination may include:
- Lids and lashes: mild swelling and erythema
- Conjunctiva: diffuse injection
- Cornea: classically a ring-shaped infiltrate with radial perineural infiltrates
- Pseudodendrites (similar to HZO)
- Reduced corneal sensation

Investigations
The diagnosis of acanthamoeba keratitis is difficult and can often be delayed. Early cases may mimic HSV keratitis.
Relevant investigations may include:
- Corneal scrape: samples for PCR, culture (non-nutrient agar with E. coli overlay) and histology
- Contact lenses, cases, and solutions should be sent for culture
- Confocal microscopy (if available): direct visualisation of acanthamoeba cysts
- A corneal biopsy may be considered in culture-negative cases
Management
Contact lens use should be discontinued immediately.
Management of acanthamoeba keratitis should include:
- Topical antiamoebic agents: topical PHMB (polyhexamethylene biguanide) 0.02% or chlorhexidine 0.02%. Hourly installation initially, then taper according to the response.
- Involved corneal epithelium can be debrided to reduce disease burden and to increase penetration of topical drops
- Oral NSAIDs for pain management
- Topical steroids
- Penetrating keratoplasty (full-thickness corneal transplant): considered in cases with severe corneal scarring or extensive necrosis. Recurrence may occur in grafted tissue.
Complications
Complications of acanthamoeba keratitis include:
- Extension of disease to involve the sclera
- Recurrent infection
- Corneal perforation
Overall, the prognosis is poor compared to other forms of microbial keratitis. Prevention is therefore vital. Contact lens wearers should be educated on avoidable risk factors and be encouraged to seek medical attention early when symptoms develop.
Summary table
Table 1. Summary of keratitis.
| Pathogens | Clinical features | Management | |
|
Bacterial |
|
|
|
|
Viral |
|
|
|
|
Fungal |
|
|
|
|
Protozoan |
|
|
|
Reviewer
Dr Vishal Vohra
Editor
Dr Chris Jefferies
References
Reference texts
- Kanski JJ, Bowling B. Clinical Ophthalmology: A Systematic Approach. Edinburgh, Elsevier/Saunders; 2015
- Denniston A, Murray P. Oxford Handbook of Ophthalmology. 4th ed. OUP Oxford; 2018.
- American Academy of Ophthalmology. 2019-2020 Basic and Clinical Science Course, Section 02: Fundamentals and Principles of Ophthalmology. 2019
Image references
- Figure 1. Community Eye Health Journal. Bacterial keratitis caused by Pseudomonas. License: [CC BY-NC 2.0]
- Figure 2. Imran Kabir Hossain. HSV Keratitis. License: [CC BY-SA 4.0]
- Figure 3. Community Eye Health Journal. Fungal keratitis. License: [CC BY-NC 2.0]
- Figure 4. Community Eye Health Journal. Acanthamoeba keratitis. License: [CC BY-NC 2.0]




