- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Hypertension (HTN) describes persistently raised arterial blood pressure and is a major risk factor for cardiovascular disease. Long-term raised blood pressure can lead to end-organ damage to the eyes, kidneys, heart and nervous system.1
In the eye, this manifests most commonly as a form of retinopathy and can lead to retinal vascular occlusion. The diagnosis of hypertensive retinopathy is made clinically from characteristic fundoscopic appearances.
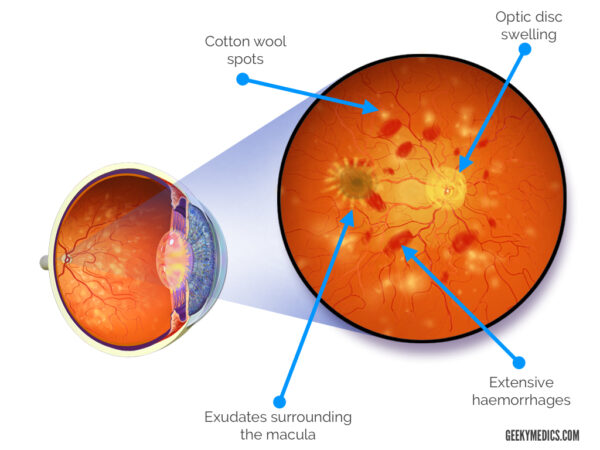
Malignant or accelerated hypertension describes an acute rise in blood pressure (>180mmHg systolic and >120mmHg diastolic) causing acute end organ damage. In the eye, this manifests as swelling of the optic disc and a form of retinopathy.
In 2015, the prevalence of hypertension in England was 31% in men and 26% in women, with more than 50% of people over 60 years affected. 10% of the adult population have hypertensive retinopathy.
Aetiology
There are several types of hypertension:2
- Primary (essential): the most common type of HTN occurring in 90% of people where no identifiable cause is found.
- Secondary: where a known cause is found, including kidney disease, obesity, pregnancy, endocrine disorders and drugs.
- Malignant or accelerated hypertension: severe increase in blood pressure to >180/120mmHg with signs of retinal haemorrhage and/or papilloedema.
- White-coat: existing only when measured during medical consultation.
- Masked: existing only with ambulatory or home blood pressure measurements and not during a clinic consultation
Hypertension is confirmed clinically by measuring a patient’s blood pressure.3
Further investigations for hypertension may include:
- Tests to confirm evidence of end-organ damage (e.g. urinalysis, ECG and U&Es)
- Tests to confirm the cause of hypertension (e.g. secondary causes)
HTN remains the biggest risk factor for cardiovascular disease, so it must be diagnosed and managed early and effectively.4
For more information, see the Geeky Medics guide to hypertension.
Clinical features
History
Hypertensive retinopathy due to chronic hypertension is usually asymptomatic and can only be diagnosed through clinical examination.
In contrast, patients with malignant or accelerated hypertension are usually symptomatic. Typical symptoms may include:
- Intermittent blurring of vision
- Visual field defects
- Headache
- Flushed and red appearance of the face
- Nausea and vomiting
- Sudden painless loss of vision due to vessel occlusion
- Signs of end-organ damage (e.g. heart failure, acute kidney injury and chest pain)
Clinical examination
Hypertensive retinopathy is a clinical diagnosis based on characteristic findings on fundoscopy. For more information, see our guide to fundoscopic appearances of retinal pathology.
There are numerous classification systems used to stage hypertensive retinopathy due to chronic hypertension.
Keith-Wagener-Barker classification of hypertensive retinopathy
The Keith-Wagener-Barker classification grades hypertensive retinopathy as follows:5,6
- Grade 1: mild, generalised constriction of retinal arterioles
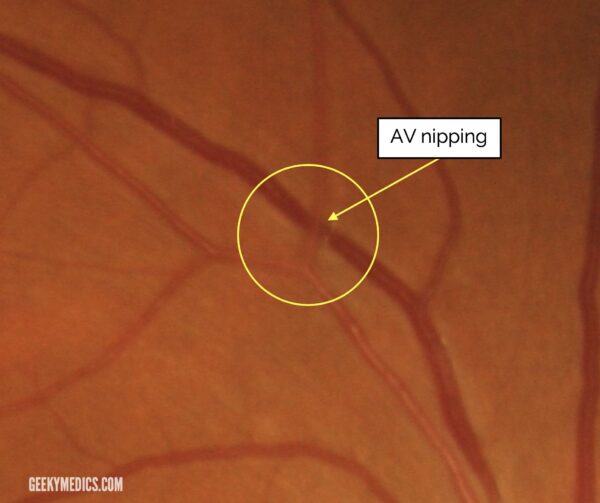
- Grade 2: definite focal narrowing of retinal arterioles and AV nicking
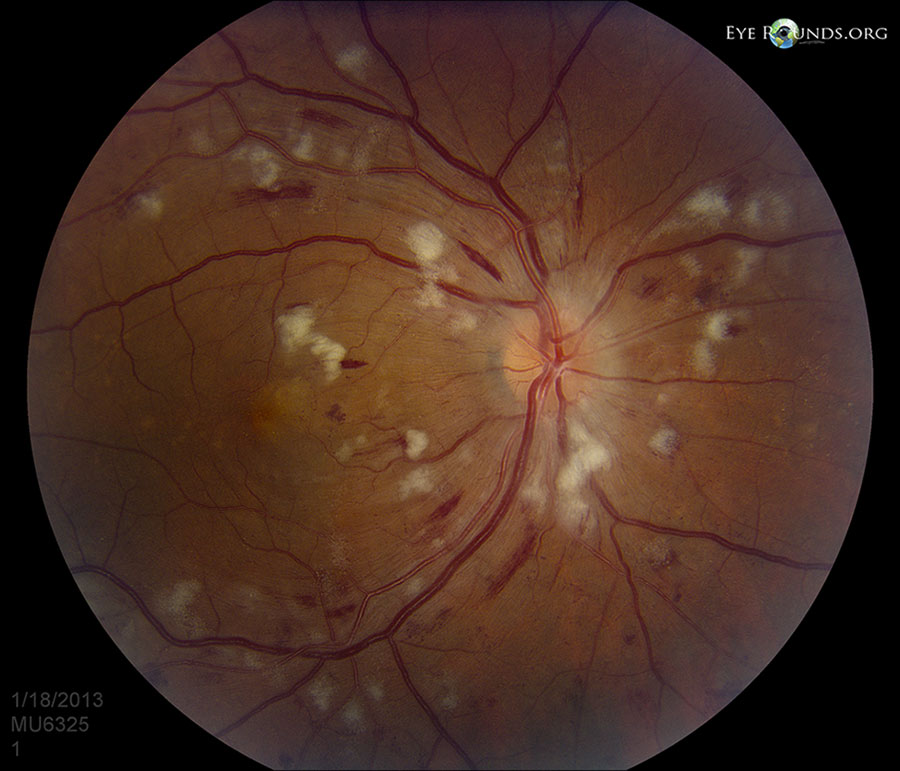
- Grade 3: grade 2 with flame-shaped haemorrhages, cotton-wool spots and hard exudates
- Grade 4: severe grade three retinopathy with papilloedema (optic disc swelling) or signs of retinal oedema
Malignant hypertension typically presents with grade four hypertensive retinopathy with evidence of papilloedema (optic disc swelling secondary to raised intracranial pressure).7,8
Investigations
Further specialised ophthalmological investigations may be used to investigate hypertensive retinopathy including optical coherence tomography (OCT) and intravenous fluorescein angiography (IVFA).
Differential diagnoses
An important differential to consider is diabetic retinopathy as many patients with hypertension may also have type one or type two diabetes mellitus.
Differences between these conditions can be distinguished through clinical history and examination findings.
Typical fundoscopic findings in diabetic retinopathy include microaneurysms, dot and blot haemorrhages, cotton wool spots and neovascularisation (new vessels on the retina).
Management
The treatment for hypertensive retinopathy primarily focuses on reducing blood pressure.
Management of chronic hypertension
Management of chronic hypertension may be split into conservative and medical management.
Conservative measures include lifestyle changes (e.g. healthy diet, regular exercise and reduced alcohol and smoking).
Medical management includes oral antihypertensives (e.g. ACE inhibitors, angiotensin receptor blockers and calcium channel blockers).
Blood pressure targets
- Target blood pressure for patients <80 years is a clinic blood pressure <140/90mmHg or ABPM/HBPM <135/85mmHg.
- Target blood pressure for patients aged >=80 years is a clinic blood pressure <150/90mmHg or ABPM <145/85mmHg.
Management of malignant or accelerated hypertension
Malignant or accelerated hypertension is a hypertensive emergency.
In a patient suspected of malignant or accelerated hypertension, NICE recommends referral for same-day specialist assessment if there are:
- Signs of retinal haemorrhage and/or papilloedema on fundoscopy
- Life-threatening symptoms such as new-onset confusion, chest pain, signs of heart failure or signs of acute kidney injury
If these complications are present, medical management should be started without waiting for ambulatory or home blood pressure monitoring to confirm.
In malignant hypertension, the aim is to reduce blood pressure over 24-48 hours. Lowering blood pressure too quickly may result in organ hypoperfusion.
An arterial line may be inserted to allow continuous blood pressure monitoring.
Intravenous anti-hypertensives such as nitroprusside, labetalol and nicardipine may be used to further control blood pressure.
Complications
Hypertension predisposes patients to other retinal vascular diseases, including central or branch retinal vessel occlusion. Ischaemia secondary to vessel occlusions can lead to further complications such as neovascularisation, vitreous haemorrhage and tractional retinal detachment.
Uncontrolled hypertension may also contribute to the progression of pre-existing diabetic retinopathy.
Delayed management of malignant hypertension may result in irreversible visual loss and changes, without treatment it carries a 90% mortality at one year.
Most retinal changes secondary to malignant hypertension will improve within six months once hypertension is well managed, but any arteriosclerotic changes in the retina will not regress.
Key points
- Hypertension describes persistently raised arterial blood pressure and is a major risk factor for cardiovascular disease
- The retina can be damaged if blood pressure rises suddenly to very high levels or if blood pressure is moderately raised over a prolonged period of time, this is known as hypertensive retinopathy.
- Hypertensive retinopathy is a clinical diagnosis with characteristic fundoscopic appearances (arteriolar narrowing, AV nicking, hard exudates and cotton wool spots)
- Grade 4 hypertensive retinopathy is diagnosed by evidence of papilloedema (optic disc swelling due to raised intracranial pressure)
- The management of hypertensive retinopathy focuses on reducing blood pressure
- Delayed management of hypertensive retinopathy may result in irreversible vision loss
- Complications include further retinal vascular disease and the progression of diabetic retinopathy
Reviewer
Dr Anne Gobbett
Speciality Doctor in Ophthalmology
Sunderland Eye Infirmary
Editor
Dr Chris Jefferies
References
- NICE CKS. Hypertension Clinical Knowledge Summaries. July 2022. Available from: [LINK]
- Wade, E. Geeky Medics. 2021. Available from: [LINK]
- Potter, L. Geeky Medics. Blood Pressure Measurement – OSCE Guide. November 2021. Available from: [LINK]
- NICE CKS. Scenario: Assessing cardiovascular risk. August 2020. Available from: [LINK]
- Bhagat, N. EyeWiki. Hypertensive Retinopathy. June 2022. Available from: [LINK]
- Bhargava, M., Ikram, M., Wong, T. Journal of Human Hypertension. 26(2):71-83. How does hypertension affect your eyes? February 2012. Available from: [LINK]
- Knott, L. Patient. Hypertensive Emergencies. June 2020. Available from: [LINK]
- Tuteja, S. Geeky Medics. Fundoscopic Appearances of Retinal Pathologies. November 2021. Available from: [LINK]
Image references
- Figure 1. Adapted by Geeky Medics. Blausen.com staff (2014). Medical gallery of Blausen Medical 2014. Licence: [CC BY 3.0].
- Figure 2. Adapted by Geeky Medics. Photograph of AV nipping originally provided by Frank Wood. License: [CC BY 3.0]
- Figure 3. Adapted by Geeky Medics. Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa. License: [CC-ND-NC 3.0]