- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Hypertension (HTN) is defined as persistently elevated arterial blood pressure.1
HTN is the single biggest risk factor for cardiovascular disease. At least half of all heart attacks and strokes are associated with HTN hence the need for early diagnosis and management of this condition.1
Please note this article does not apply to the management of HTN in patients with type 2 diabetes.
Aetiology
There are several types of HTN:
- Primary: HTN where no identifiable cause is found; most common type of HTN; occurs in 90% of patients.
- Secondary: HTN where an underlying cause exists; occurs in 10% of patients.
- Accelerated or malignant HTN: Severe increase in blood pressure to ≥180/120mmHg, and often higher, associated with signs of retinal haemorrhages and/or papilloedema on fundoscopy.
- White-coat: HTN exists only when blood pressure is measured during medical consultations with a discrepancy of >20/10mmHg between clinic blood pressure measurements and ambulatory or home blood pressure measurements.
- Masked HTN: Clinic blood pressure measurements are <140/90mmHg but ambulatory or home blood pressure measurements are >140/90mmHg.
Causes of secondary hypertension
Kidney disease is the most common cause of secondary HTN.
Table 1. Causes of secondary hypertension.
| Causes of secondary hypertension | Examples |
|
Kidney disease |
|
|
Vascular disease |
|
|
Endocrine disease |
|
|
Drugs |
|
|
Other causes |
|
Risk factors
There are several risk factors that increase a person’s chance of developing HTN:2
- Sex: up to 65 years women tend to have lower blood pressures than men, however, between the ages of 65-74 years women tend to have higher blood pressures.
- Ethnicity: people of Black African and Black Caribbean origin are at a higher risk of developing HTN.
- Age: blood pressure rises with increasing age.
- Lifestyle factors: cigarette smoking, excess alcohol consumption, excess dietary salt intake, obesity and lack of physical activity.
Clinical features
History
Most cases of HTN will be asymptomatic. Often HTN is an incidental finding.
It is important to recognise the red flag symptoms of accelerated or malignant HTN. These include:
- Headache
- Visual disturbances
- Seizures
- Nausea and vomiting
- Chest pain
Symptoms suggestive of kidney disease as a secondary cause of HTN include:
- Haematuria
- ‘Frothy’ urine suggestive of proteinuria
- Dyspnoea (pulmonary oedema)
- Lower limb swelling (peripheral oedema)
- Flank tenderness and pain
- Weight loss is suggestive of renal cell carcinoma
Symptoms suggestive of coarctation of the aorta as a secondary cause of HTN include:
- Headache
- Epistaxis
- Intermittent claudication
- Lower limb weakness
- Cold legs and feet
Symptoms suggestive of endocrine disease as a secondary cause of HTN include:
- Muscle weakness, muscle spasms and paraesthesia are suggestive of hyperaldosteronism.
- Severe headache, palpitations and sweating are suggestive of phaeochromocytoma.
- Weight gain particularly abdominal, facial and on the back of the neck and shoulders is suggestive of Cushing’s syndrome.
- Tall statures, swelling of the hands and feet and deepening of the voice are suggestive of acromegaly.
- Weight gain, cold intolerance and low mood are suggestive of hypothyroidism.
- Weight loss, heat intolerance and palpitations are suggestive of hyperthyroidism.
Other important areas to cover in the history include:
- Menstrual history (e.g. date of last menstrual period): pregnancy-related hypertension and pre-eclampsia
- Family history: autosomal dominant polycystic kidney disease
- Medication history
Clinical examination
The majority of patients with HTN will have no findings on examination.
All patients with HTN should undergo fundoscopy looking for hypertensive retinopathy suggestive of accelerated or malignant HTN. See the Geeky Medics guide for examples of hypertensive retinopathy.
A number of examinations may be indicated in patients with HTN and the history should guide your examination choice.
Typical clinical findings in secondary causes of HTN include:
- Autosomal dominant polycystic kidney disease: enlarged palpable kidneys when balloting the kidneys.
- Renal artery stenosis: renal bruits heard when auscultating over the area of the renal arteries.
- Coarctation of the aorta: systolic murmur in the left infraclavicular region under the left scapula and radio-femoral delay.
- Cushing’s syndrome: moon facies, abdominal purple striae and bruising.
- Hypothyroidism: brittle nails, dry skin and thin hair.
- Hyperthyroidism: fine tremor, palmar erythema and a neck goitre.
Investigations
Diagnosis of hypertension requires the measurement of blood pressure. There are 3 types of blood pressure measurement to understand:
- Clinic blood pressure: patient’s blood pressure recorded during the consultation.
- Ambulatory blood pressure monitoring (ABPM): blood pressure during normal activities of daily living recorded using a 24-hour blood pressure monitor.
- Home blood pressure monitoring (HBPM): home blood pressure readings recorded by the patient twice a day, once in the morning and once in the evening.
Measuring blood pressure
The steps required to accurately measure blood pressure are described below. These are summarised from the NICE guidelines.1
The patient’s blood pressure should be measured with the patient quiet and seated with their outstretched arm supported.
Ideally, the blood pressure should be measured manually using a sphygmomanometer. This is particularly important in patients with an irregular pulse as automated devices can be inaccurate in these patients. See the Geeky Medics guide for further information.
Measure the blood pressure in both arms:
- If the difference between arms is >15mmHg repeat both measurements.
- If the difference remains >15mmHg on the second measurement, measure subsequent blood pressures in the arm with the high readings.
If the clinic blood pressure is ≥140/90mmHg take a second measurement:
- If the second measurement is significantly different from the first measurement take a third blood pressure measurement.
- Record the lower of the second and third measurements as the clinic blood pressure.
If the patient’s blood pressure is between 140/90mmHg and 180/120mmHg offer ABPM or HBPM to confirm the diagnosis of HTN.
ABPM
Ensure at least two blood pressure measurements are taken per hour during the person’s usual waking hours.
Use the average value of at least 14 measurements to confirm a diagnosis of HTN.
HBPM
Ensure blood pressure is measured twice daily; ideally once in the morning and once in the evening.
For each blood pressure measurement, advise the patient to record two consecutive measurements taken at least one minute apart whilst seated.
The patient should record their blood pressure recording for at least four days but ideally for seven days.
After 7-14 days discard the measurements taken on the first day and use the average value of all the remaining measurements to confirm a diagnosis of HTN.
Stages of hypertension
Classify the stage of HTN as either 1, 2 or 3.
Table 2. The stages of hypertension according to blood pressure.
| Stage | Clinic Blood Pressure | Ambulatory Blood Pressure Monitoring (ABPM) Home Blood Pressure Monitoring (HBPM) |
| Stage 1 | ≥140/90mmHg | ≥135/85mmHg |
| Stage 2 | ≥160/100mmHg | ≥150/95mmHg |
| Stage 3 | ≥180/120mmHg | – |
Common errors in blood pressure measurement
Errors in blood pressure measurements can arise from:
- Incorrect patient positioning
- Poor understanding of measuring technique
- Incorrect cuff size: the bladder should encircle at least 80% of the arm
- Incorrect cuff position: the cuff should be placed 2cm above the brachial artery and the ‘artery mark’ on the cuff should be aligned with the brachial artery
Bedside investigations
Relevant bedside investigations include:
- Urinalysis: to look for haematuria and proteinuria which could suggest kidney disease.
- Urine albumin creatinine ratio (uACR): albuminuria suggests end-organ damage.
- ECG: to look for signs of cardiac arrhythmias and heart failure.
Laboratory investigations
Relevant laboratory investigations include:
- Urea and electrolytes: derangement suggests a renal impairment.
- HbA1c: indicates blood glucose concentration over the previous 3 months; high levels may suggest diabetes.
- Lipid profile: useful to assess future cardiovascular disease risk.
Assessing cardiovascular disease risk
Cardiovascular disease risk can be assessed using the online tool QRISK3.
This considers factors such as patient sex, age, ethnicity, smoking status and presence of comorbidities to generate an overall percentage that estimates the risk of a patient having a heart attack or stroke in the next 10 years.
Management
Blood pressure targets
The target blood pressure for patients aged <80 years is a clinic blood pressure <140/90mmHg or ABPM/HBPM <135/85mmHg.
The target blood pressure for patients aged ≥80 years is a clinic blood pressure <150/90mmHg or ABPM/HBPM <145/85mmHg.
Conservative management
Conservative management should be offered to all patients with HTN:
- Advising patients to follow a healthy diet and exercise regularly.
- Encouraging patients to reduce dietary salt intake.
- Encouraging patients to reduce caffeine consumption.
- Advising patients to stop smoking.
- Advising patients to reduce their alcohol consumption.
Medical management
The decision to commence anti-hypertensive medication depends upon the stage of HTN.
For stage one hypertension:
- Discuss anti-hypertensive drug therapy with patients aged <80 years who have ≥1 of the following: established cardiovascular disease, kidney disease or an estimated 10-year risk of cardiovascular disease of ≥10%.
- Consider anti-hypertensive drug therapy for patients aged ≥80 years who have a clinic blood pressure >150/90mmHg.
- Consider anti-hypertensive drug therapy for patients aged <60 years with an estimated 10-year risk of cardiovascular disease <10%.
For stage two and three hypertension:
- Offer antihypertensive drug therapy to all patients.
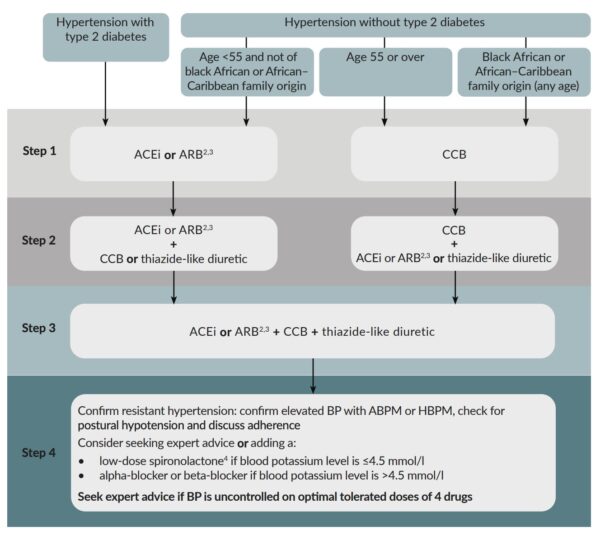
A single anti-hypertensive drug is often inadequate to control HTN so a stepwise approach is used to add further drugs until controlled is achieved (Figure 1).3 A minimum of 4 weeks should be allowed to determine whether a drug or combination of drugs have been successful at reducing the blood pressure.
Step 1
Patients aged <55 years who are not of Black African or African-Caribbean descent: offer an ACE inhibitor such as ramipril. If an ACE inhibitor is not tolerated offer an angiotensin-II receptor blocker such as losartan.
Patients aged ≥55 years and patients of Black African or African-Caribbean descent: offer a calcium channel blocker such as amlodipine.
Step 2
Patients already taking an ACE inhibitor or angiotensin-II receptor blocker: offer a calcium channel blocker such as amlodipine or a thiazide-type diuretic such as indapamide.
Patients already taking a calcium channel blocker: offer an ACE Inhibitor such as ramipril or a thiazide-type diuretic such as indapamide.
- If an ACE Inhibitor is not tolerated offer an angiotensin-II receptor blocker such as losartan.
- Angiotensin-II receptor blockers preferred in patients Black African or African-Caribbean descent.
Step 3
Offer a combination of an ACE inhibitor or angiotensin-II receptor blocker plus a calcium channel blocker and thiazide-type diuretic.
Step 4
Patients whose blood pressure is not adequately controlled using steps 1-3 are said to have resistant HTN. Management options at this stage depend upon the serum potassium.
- Serum potassium ≤4.5mmol/l: offer low-dose spironolactone.
- Serum potassium of >4.5mmol/L: offer an alpha-blocker such as doxazosin or a beta-blocker such as atenolol.
Patients should be referred for specialist assessment if they remain hypertensive despite 4 anti-hypertensive drug therapies.
Managing accelerated or malignant HTN
Accelerated or malignant HTN are referred to as hypertensive emergencies and some patients will require admission to hospital. NICE recommends the following management if a patient’s clinic blood pressure is ≥180/120mmHg.
Refer for same-day specialist assessment if there are:
- Signs of retinal haemorrhage and/or papilloedema on fundoscopy.
- Life-threatening symptoms such as new-onset confusion, chest pain, signs of heart failure or signs of acute kidney injury.
If none of the above are present, investigate for signs of complications associated with HTN as soon as possible:
- If complications are present you should start medical management without waiting for ABPM/HBPM.
- If complications are not present you should repeat blood pressure measurements within 7 days.
The aim of managing accelerated or malignant HTN is to reduce the blood pressure over a 24 – 48 hour period. If blood pressure is reduced too quickly this can lead to organ hypoperfusion.
If hospital admission is required, an arterial line is often inserted in patients with accelerated or malignant HTN as this allows for continuous blood pressure monitoring.
Intravenous anti-hypertensive agents such as nitroprusside, labetalol and nicardipine can be used to control blood pressure in accelerated or malignant HTN.4
Complications
The complications of HTN can be grouped according to the organs affected:
- Brain: stroke (both ischaemic and haemorrhagic) and vascular dementia
- Eye: hypertensive retinopathy
- Heart: coronary artery disease, peripheral vascular disease, cardiac arrhythmias and heart failure
- Kidneys: chronic kidney disease
Key points
- HTN is defined as a persistently elevated arterial blood pressure and is the single biggest risk factor for cardiovascular disease.
- In the majority (90%) of patients, no underlying (secondary) cause of HTN is found.
- Kidney disease is the most common cause of secondary HTN.
- Diagnosing HTN involves measuring a patient’s ambulatory blood pressure or asking a patient to regularly measure their blood pressure at home.
- HTN cannot be diagnosed from a single blood pressure reading.
- The management of HTN comprises both conservative measures and medical measures; the latter is set out in the NICE anti-hypertensive medications algorithm.
- Complications of HTN can be grouped according to the organ affected; these include brain, eyes, heart and kidneys.
Reviewer
Dr Lindsay Muscroft
General Practitioner & Senior Clinical Teaching Fellow
Editor
Dr Chris Jefferies
References
- NICE. Hypertension – not diabetic. Published October 2019. Available from: [LINK]
- Public Health England. Health matters: combating high blood pressure. Published January 2017. Available from: [LINK]
- NICE. Choice of antihypertensive drug, monitoring treatment and BP targets. Published October 2019. Available from: [LINK]
- Patient. Hypertensive Emergencies. Published January 2016. Available from: [LINK]




