- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This guide provides a step-by-step approach to explaining a diagnosis of chronic obstructive pulmonary disease (COPD). You should also read our overview of how to effectively communicate information to patients.
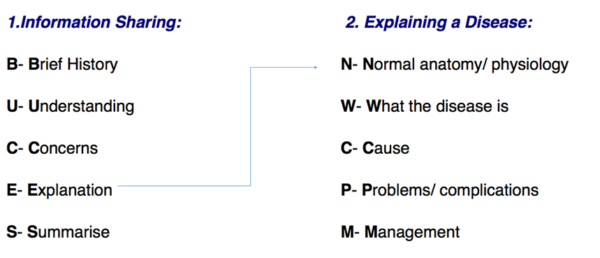
Structuring your explanation
Explaining a diagnosis requires structure and adequate background knowledge of the disease. Whether the information being shared is about a procedure, a new drug or a disease, the BUCES structure (shown below) can be used.
Opening the consultation
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
BUCES can be used to remember how to structure a consultation in which providing information is the primary focus. Before explaining the various aspects of a disease, it is fundamental to have a common starting point with your patient. This helps to establish rapport and creates an open environment in which the patient can raise concerns, ask questions and gain a better understanding of their problem. After introducing yourself, it is important to take a brief history (this is the first part of the BUCES structure):
- What has brought the patient in to see you today?
- What are their symptoms?
- Are there any risk factors that can be identified? (e.g. lifestyle/family history)
For example, a patient with COPD may describe episodes of shortness of breath, wheezing and cough.
Tip: Practice taking concise histories to get the timing right. In OSCE stations, timing is crucial and you do not want to spend all your time taking a history when you are meant to be explaining a diagnosis! A rough guide would be to keep the introduction and brief history between 1-2 minutes maximum.
What does the patient understand?
Following a brief history, it is important to gauge the patient’s knowledge of their condition. COPD is one of the most common respiratory diseases and ranks the third leading cause of death worldwide1. Patients may know someone with the condition, or this may be their first encounter with the disease. The patient sitting before you may not even know at this point that they have COPD – you may be the first person to inform them of the diagnosis.
Due to these reasons, it is important to start with open questioning. Good examples include:
- “What do you think is causing your symptoms?”
- “Have you heard of COPD before?”
- “What do you know about COPD?”
- “What has been explained to you about COPD so far?”
Open questioning should help you determine what the patient currently understands, allowing you to tailor your explanation to an appropriate level.
At this stage, primarily focus on listening to the patient. It may also be helpful to give positive feedback as the patient talks (i.e. should a patient demonstrate some understanding, reinforce this knowledge with encouraging words and non-verbal communication such as nodding).
Checking the patient’s understanding should not be solely confined to this point of the consultation but should be done throughout by repeatedly ‘chunking and checking’.
Tip: Try using phrases such as: “Just to check that I am explaining COPD clearly, can you repeat back to me what you understand so far?”. This is far better than only saying, “What do you understand so far?” as the onus is placed upon the quality of your explanation rather than an issue with the patient’s ability to understand.
What are the patient’s concerns?
The patient’s concerns should never be overlooked. A diagnosis of COPD can be a significant life event and provoke a variety of worries. Asking the patient if they have any concerns before beginning your explanation allows you to specifically tailor what is most relevant to the patient, placing them at the centre of the explanation. The ICE (ideas, concerns and expectations) format, can provide a useful structure for exploring this area further.
ICE
Ideas:
- What does the patient think is causing their symptoms?
- What is their understanding of the COPD?
Concerns:
- What are the patient’s concerns regarding their symptoms and diagnosis?
Expectations:
- What is the patient hoping to get out of the consultation today?
Explanation
After determining the patient’s current level of understanding and concerns, you should be able to explain their condition clearly. COPD can be confusing to medical students and doctors, let alone patients. Avoid medical jargon so as not to confuse your patient.
You should begin by signposting what you are going to explain to give the patient an idea of what to expect.
“I’m going to begin by talking about how the lungs work and then move on to discuss what COPD is, what causes it and how we can manage it together.”
In preparation for your OSCE, practice your explanation in patient-friendly terms. Consider using visual aids such as diagrams or drawings to help understanding.
Tip: Use the mnemonic “Normally We Can Probably Manage” to help you remember the structure of explaining a disease.
Normal anatomy and physiology1,2
“Your lungs are responsible for breathing, supplying your body with oxygen and removing waste carbon dioxide.”
“When you breathe in, air enters through your mouth or nose and goes down the windpipe (trachea). The trachea divides into smaller tubes called bronchi, which further branches into even smaller tubes called bronchioles.”
“At the end of the bronchioles, there are tiny stretchy air sacs called alveoli. These air sacs resemble bunches of grapes or a bundle of balloons. Oxygen enters your blood through the walls of the alveoli, while carbon dioxide, a waste gas, is removed.”
What is COPD?
Chronic Obstructive Pulmonary Disease (COPD) is a group of long-term conditions that affect the lungs. The patient should understand that COPD is not curable, but by avoiding smoking and receiving treatment, their symptoms can improve.1
COPD includes conditions such as emphysema and chronic bronchitis.
Explain to the patient that emphysema is where the air sacs (alveoli) are damaged. The once elastic walls weaken, resulting in larger sacs instead of numerous small air spaces. This impairs efficient gas exchange.
Additionally, explain that chronic bronchitis involves inflammation of the tubes (bronchi) responsible for carrying air to and from the lungs. The airway walls become scarred and narrowed. This inflammation makes it harder for air to enter the lungs and the ‘stale’ air to leave, leading to an increased risk of lung infections. This can also mean that patients bring up more phlegm or mucus.3, 4, 5
“Chronic obstructive pulmonary disease or COPD is a common condition affecting your lungs, making it harder for you to breathe. It includes conditions such as emphysema and chronic bronchitis.”
“In COPD, there is inflammation in the lungs (chronic bronchitis), which causes narrowing of the small tubes in your lungs. This makes it more difficult to breathe. In addition, the inflammation causes your lungs to produce lots of mucous, which you cough up as phlegm.”
“Also, in COPD, the air sacs in the lungs called alveoli are destroyed (emphysema). This makes it harder for your body to absorb oxygen from the air in the lungs.”
What are the causes of COPD?
Explain to the patient that COPD is usually caused by long-term exposure to harmful substances:6
- Smoking: the main risk factor for developing COPD is smoking or second-hand smoke. This risk increases the more the patient smokes and the duration of their smoking.
- Environmental pollutants: prolonged exposure to chemical fumes, dust and occupational smoke.
- Alpha-1-antitrypsin deficiency: a rare genetic condition causing a lack of a protective protein called alpha-1-antitrypsin; this normally helps protect lung tissue from damage caused by enzymes.1,4,7
“COPD is caused by long-term exposure to harmful irritants that damage the lungs over time.”
“The most common cause of COPD is smoking. This risk increases the more you smoke and the longer you’ve been smoking.”
“Some other things that cause COPD include breathing in chemical fumes, air pollution or rarely an inherited genetic condition.”
Problems/complications of COPD
Progressive symptoms
Explain to patients that COPD develops over several years and their symptoms may not be noticeable until recently. These symptoms worsen over time and make their activities of daily living more difficult, however, treatment can help slow the progression of COPD.
Common symptoms of COPD include:
- Breathlessness and wheeze: chronic bronchitis causes progressive narrowing of the airways, leading to increased resistance to airflow in and out of the lungs.
- Chronic cough: due to irritation and inflammation of the airways and is often productive of mucus or phlegm.
- Chest infections: damaged lung tissue and impaired clearance of mucus and bacteria making patients for susceptible to infections.
“The symptoms of COPD develop slowly usually over years; you may have not noticed your symptoms until recently. Unfortunately, symptoms like breathlessness and cough tend to worsen over time, making daily activities more challenging. While treatment can help slow the progression of symptoms, there is no cure for COPD.”
“Due to narrowing of the airways, it becomes harder for air to flow in and out of the lungs, resulting in a sensation of breathlessness or feeling unable to catch your breath.”
“Damage, irritation, and inflammation of the airways can lead to increased mucus production and a cough that doesn’t seem to go away.”
“Sounding wheezy occurs when the airways become narrowed, causing resistance to the airflow.”
Infections and exacerbations
Patients should be aware that they could experience a sudden worsening of their symptoms, known as an exacerbation. They may experience increased breathlessness, wheezing, coughing, and a change in the colour or amount of sputum (phlegm). Exacerbations can occur spontaneously or be triggered by viral or bacterial infections.3,9,10
“People with COPD are more prone to developing chest infections, especially during the wintertime, as it becomes harder for the lungs to effectively clear mucus and bacteria that may have settled in the lungs.”
“You may sometimes get a flare-up or attack, when your COPD symptoms get a lot worse than usual. Doctors call these exacerbations. You may experience worsening breathlessness, coughing, wheezing, and more mucus production. These can be triggered by infections, exposure to irritants or changes in weather.”
Management
Stopping smoking
Emphasise to the patient that stopping smoking is the most important thing to do. While any damage done to the airways cannot be reversed, quitting smoking is the most effective measure to slow the progression of COPD and improve lung function.11,12
“The most important thing you can do for your COPD and your overall health is to stop smoking. This is the most effective way to prevent your COPD getting worse, even though the existing damage to your lungs cannot be reversed. By quitting smoking, can help prevent further damage and improve your breathing.”
If the patient is a smoker offer smoking cessation advice. For more information, see the Geeky Medics guide to smoking cessation counselling.
Vaccines
Patients with COPD should ensure they stay up to date with their vaccines. They are encouraged to have the annual influnza vaccination and a one-off pneumococcal vaccination. This is important as they are more vulnerable to infections, worsening symptoms and leading to complications.12
“As a patient with COPD, you are entitled to free vaccinations. You should have a one-off pneumococcal vaccination and keep up to date with your annual flu jabs. These viruses can cause severe illness and make you very unwell.”
Pulmonary rehabilitation
Pulmonary rehabilitation is a programme of exercise and education to help patients with chronic lung conditions such as COPD. These programmes last six to eight weeks, with two sessions of two hours each week. They encompass physical exercise, dietary advice, education on COPD and emotional support.
The goals of pulmonary rehabilitation are to help patients understand and manage COPD, improve overall well-being, increase exercise tolerance, improve lung function, reduce the chance of hospital admission and improve patients’ quality of life.11,15
“Pulmonary rehabilitation is a treatment programme made up of exercise classes, information about looking after your lungs, how to eat well, advice on managing COPD and techniques to improve your breathlessness.”
“This will help you understand COPD, reduce breathlessness and improve both your physical and mental health.”
Inhalers
For most patients, short-acting bronchodilators are the first treatment used. Explain to patients that this inhaler is used when they feel breathless. The inhaler delivers a small dose of medicine directly to the lungs, relaxing the smooth muscles in the airways, causing bronchodilation, and making breathing easier. These work quickly and effects last for up to six hours.11,13,14
“When you use this inhaler, it delivers a small amount of medicine directly to your lungs. This medication works by relaxing the muscles in your airways, which helps them to open up. Breathing will become easier, and you will get relief from breathlessness.”
Other inhalers (e.g. long-acting bronchodilators and corticosteroids) may also be used to manage COPD.12,14
“Long-acting bronchodilator inhalers are used to provide sustained relied of breathlessness and other COPD symptoms throughout the day. You typically use these inhalers twice a day as they have longer lasting effects.”
“You might also be prescribed a steroid inhaler. These work to reduce swelling and inflammation in the airways improving your symptoms. These should be used consistently, even when you are feeling well to help maintain your airways and prevent flare-ups of your COPD.”
For more information on inhaler counselling, see the Geeky Medics guide to inhaler technique.
Other medications
If a patient develops an exacerbation of COPD, they may be prescribed a short course of steroid tablets. The course typically lasts five days to reduce inflammation in the airways and get the flare-up under control. Antibiotics are used if the patient develops a bacterial chest infection or exacerbation.
These medications are best taken as the flare-up starts, so patients may have courses to be kept at home and should be made aware of the signs and symptoms of an exacerbation.11,12,14
“During a flare-up, your GP may prescribe you a short course of steroid tablets. These will help reduce inflammation in your airways and bring the flare-up under control. Typically, the course lasts for five days.”
“If you experience symptoms suggesting a bacterial chest infection like worsening breathlessness, cough or a change in colour like it becoming brown, green or yellow or a change in consistency like it getting thicker your doctor may prescribe you a short course of antibiotics.”
“It’s important to start taking these medications as soon as you notice a flare-up. Your GP may provide you with a supply of these tablets to keep at home as it is best to treat the flare-up as soon as it starts.”
Patients who experience a lot of phlegm production, persistent coughing and frequent exacerbations may be prescribed a mucolytic (e.g. Carbocisteine). Mucolytics work by loosening the mucus in the airways, making it easier for patients to cough up. This improves breathing and reduces coughing.12,15
“You may be prescribed a type of medicine called a mucolytic, this helps you cough up mucus or sputum by making your phlegm less thick and sticky. This will make it easier to cough up and clear mucus from your lungs keeping your airways clear.”
Other treatments
Long-term oxygen therapy (LTOT) is used in specific patients where COPD causes a low oxygen level in the blood. Patients must have stopped smoking to be eligible for this treatment.12,13,16
“If oxygen levels in your blood are low and you meet specific criteria, you may benefit from Long-term oxygen therapy. This involves receiving air with a higher oxygen level through a nasal tube or mask for at least 15 hours per day. This will improve your breathing, and the aim is to extend your life.”
Surgical treatments include lung reduction surgery and lung transplantation. These are only used in specific circumstances, and most patients with COPD will not undergo these procedures.
Closing the consultation
Summarise the key points back to the patient.
“We have discussed quite a lot today, including what COPD is, the symptoms you might experience and how the condition is managed. I realise this is a lot of information to take in and therefore I have a leaflet which summarises everything we’ve discussed. It is also important that you seek a review if you notice your symptoms worsening. If you begin to feel very short of breath, despite using your treatments, you should call an ambulance.”
Ask the patient if they have any questions or concerns that have not been addressed.
“Is there anything I have explained that you’d like me to go over again?”
“Do you have any other questions before we finish?”
Direct the patient to further information about the condition using websites and leaflets.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Reviewer
Dr Sundari Ampikaipakan
Consultant Respiratory Physician
References
- WHO. Chronic Obstructive Pulmonary Disease (COPD). March 2023. Available from: [LINK]
- OpenStax. Organs and structures of the respiratory system. October 2020. Available from: [LINK]
- Asthma and the lung UK. What is COPD?. May 2022. Available from: [LINK]
- Patient info. Chronic Obstructive Pulmonary Disease. November 2018. Available from: [LINK]
- Patient info. Emphysema. May 2018. Available from: [LINK]
- NHS.uk. Causes chronic obstructive pulmonary disease (COPD). April 2016. Available from: [LINK]
- NHS inform. Causes of COPD. January 2023. Available from: [LINK]
- BMJ Best Practice. Patient leaflet COPD. December 2021. Available from: [LINK]
- NHS inform. Symptoms of COPD. January 2023. Available from: [LINK]
- NHS.uk. COPD – Symptoms. April 2023. Available from: [LINK]
- NHS inform. Treating COPD. January 2023. Available from: [LINK]
- NHS.uk. COPD – Treatment. April 2023. Available from: [LINK]
- Asthma and lung UK. What are the treatments for COPD? May 2022. Available from: [LINK]
- Asthma and lung UK. Medications for COPD. May 2022. Available from: [LINK]
- NHS.uk. About Carbocistine. March 2023. Available from: [LINK]
- NHS.uk. Home oxygen therapy. August 2023. Available from: [LINK]
- Asthma and lung UK. Lung Volume reduction procedures. November 2022. Available from: [LINK]