- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Lumbar spine X-rays are one of the most commonly requested radiographic investigations of the spine, however, it should be noted that projectional radiography has limitations and other imaging modalities such as MRI and CT should be considered if further evaluation is required.
A lumbar spine X-ray is a picture of the vertebrae in the lower part of the spine. This area includes the lumbar region and the sacrum. It is important to remember that lumbar spine X-rays involve a significant radiation dose (approximately 70 chest X-rays). The relevant literature suggests that lumbar spine X-rays are not routinely indicated for uncomplicated back pain which resolves in about 90% of cases within 2 months, regardless of treatment.
Indications for a lumbar spine X-ray
Appropriate clinical indications for lumbar spine X-ray include:1
- Significant trauma (not “lifting something” or “bending to pick up something” etc)
- Age less than 20 or greater than 50
- Past medical history of malignancy, ankylosing spondylitis or osteoporosis
- Chronic corticosteroid use (increased risk of fracture)
- An episode of back pain ongoing for 6 weeks or longer without improvement
Confirm the details
Begin by confirming you have the correct patient and the correct radiograph by assessing the following:
- Patient details (name, date of birth, unique identification number)
- Date and time the radiograph was taken
If previous radiographs are available, these should also be reviewed to provide a point of reference.
Acquire all necessary views
There are two standard projections produced when a lumbar spinal X-ray is performed:
- Lateral
- Anterior-posterior (AP)/posterior-anterior (PA)
In the case of trauma, additional views can be sought including oblique and horizontal beam lateral views.
Views and adequacy
Lateral view
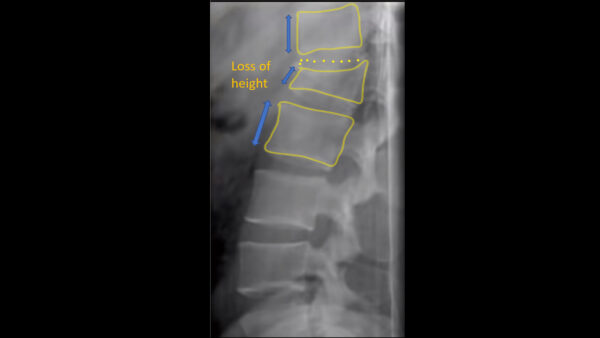
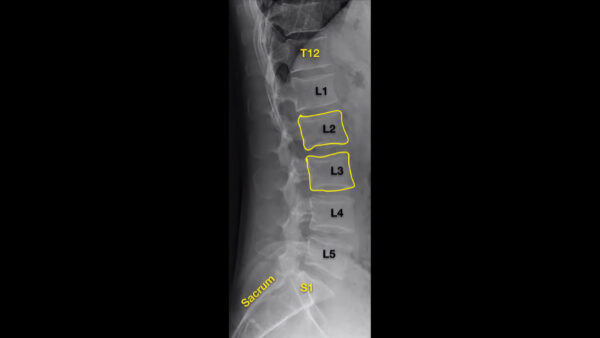
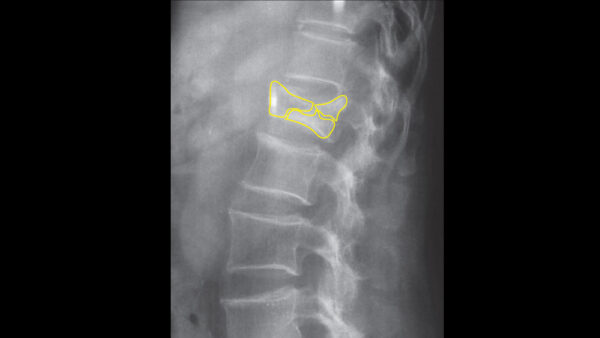
In a lateral view, the entire lumbar spine should be visible from T12-S1.
Lateral views are particularly useful for identifying fractures. Each vertebra (highlighted in yellow) should be examined looking for a loss of height which could indicate a compression fracture commonly associated with osteoporosis (see fractures section below).
Compression fractures are often seen in the upper lumbar or lower thoracic vertebrae.
Anterior-posterior (AP)/posterior-anterior (PA)
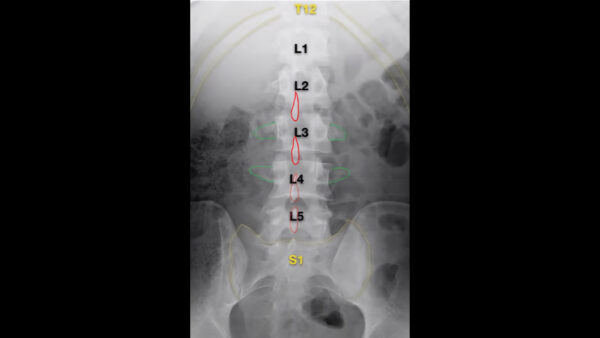
In an AP/PA view, the entire lumbar spine should be visible from T12 superiorly and the sacrum inferiorly.
The spinous processes (red) should be central and there should be equal distance between transverse processes (green). Transverse processes are often obscured by gas from the abdomen.
Spinal imaging should be taken erect in the non-trauma setting to give a functional overview of the lumbar spine. Patients with a suspected spinal injury must remain immobilised in the supine position.
Alignment
There are multiple lines that should be assessed across each of the two typical radiographic views of the lumbar spine (AP/PA & lateral). These lines should run uninterrupted in healthy individuals.
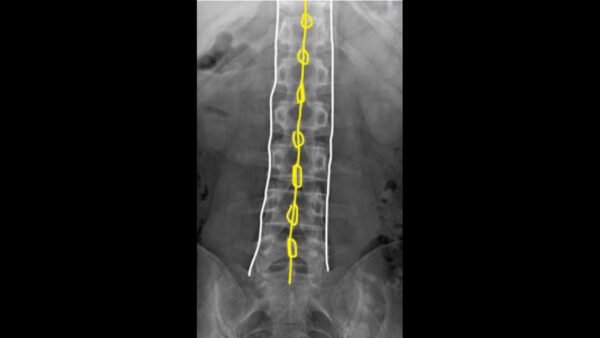
On the AP/PA view check that the vertebral bodies and spinous processes are aligned.
On the lateral view, check the alignment of the vertebral bodies.
Disruption of any of these lines may indicate an underlying fracture.
Interpretation
A structured approach to lumbar spine X-ray interpretation is essential.
Step 1
Assess alignment of the vertebral bodies and spinous processes including the lines discussed above and the distance between spinous processes.
Step 2
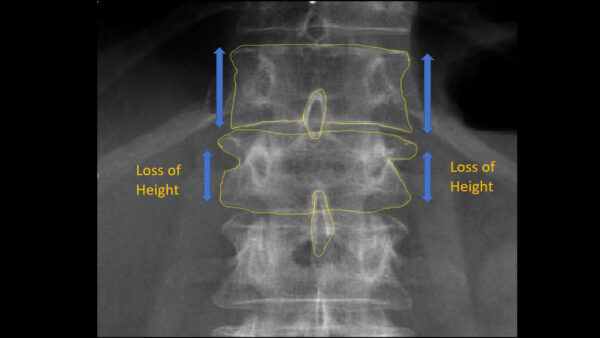
Inspect for loss of vertebral height:
- The height of vertebral bodies should be equal in healthy individuals
- Loss of vertebral height is suggestive of a fracture
Step 3
Inspect the vertebral spaces:
- In healthy individuals, the disc height should gradually increase from superior to inferior
- Note: the L5/S1 space is normally slightly narrower than L4/L5
Step 4
Inspect the vertebral endplates: the continuity of superior and inferior endplates should remain uninterrupted.
Step 5
Trace the posterior elements including:
- Pedicles
- Laminae
- Spinous processes
Ensure the vertebral and spinous processes are intact.
Pathology
Fractures
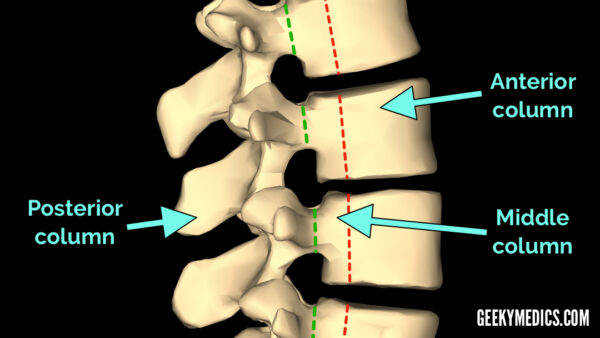
When describing and diagnosing spinal fractures, Radiologists divide the spinal column into 3 sections known as the ‘Three Column model’. This states that if any 2 columns are injured then the injury is ‘unstable’. If spinal instability is suspected further imaging with CT or MRI should be considered.
Anterior column
Involves the anterior two-thirds of the vertebral body/intervertebral disc and the anterior longitudinal ligament.
Middle column
Involves the posterior aspect of the vertebral body/intervertebral disc and the posterior longitudinal ligament.
Posterior column
Involves the posterior elements including the lamina, facet joints, spinous processes, and the associated ligaments.
Anterior column – anterior compression fracture
An anterior compression fracture is a fracture in which the front part of the vertebral body is crushed, resulting in a wedge shape.
Anterior compression fractures are the most common type of lumbar spine fracture.
Middle column- ‘burst fracture’
A burst fracture occurs when the vertebral body is crushed in all directions simultaneously (e.g. sudden axial loading force). This type of fracture can result in bone fragments being projected outwards anteriorly into the spinal canal causing secondary spinal cord injury.
A burst fracture involves two columns and is therefore typically considered to be unstable.
Posterior column – flexion-distraction fracture
Flexion-distraction fractures (a.k.a. chance fractures) occur when any part of the spinal column breaks away from another part. This type of fracture is often caused by sudden severe compression or rotation of the spine (e.g. use of a lap-only seat belt during a deceleration injury, resulting in forceful forward flexion of the spine).
The result is a fracture of the vertebral body with associated transverse/horizontal fractures of the posterior elements. This type of fracture is unstable and carries a high risk of spinal cord injury.

Spondylosis
Spondylosis involves degeneration of the interverbal disc leading to disc space narrowing, endplate sclerosis and osteophyte formation.
In some cases, osteophytes can cause neural impingement.
Spondylolysis
Spondylolysis occurs when a fracture (acute or chronic) extends from the inferior facet across the pars interarticularis (area of the lamina that lies within the facets), to the superior facet.
This defect can in some cases be bilateral and lead to spondylolisthesis (see below). Spondylolysis is often best identified on an oblique radiograph, appearing (with the eye of faith) to represent a “Scotty dog”:4
- Nose: transverse process
- Eye: pedicle
- Ear: superior facet
- Front leg: inferior facet
- Neck: pars interarticularis
- Collar across the neck: fracture

Spondylolisthesis
Spondylolisthesis occurs when one vertebra is displaced forward upon another.
This can occur secondary to trauma or as a result of degenerative disease such as osteoarthritis. If severe it may lead to foraminal stenosis, causing nerve root impingement.

Vertebral bone lesions
Vertebral bone lesions can often be asymptomatic in patients and thus are often identified incidentally.
These lesions typically become symptomatic when they present as a pathological fracture with or without neurological deficits secondary to extension into the spinal canal.
Differential diagnoses for a lytic spinal lesion include:6
- Prostate cancer metastases
- Breast cancer metastases
- Thyroid cancer metastases
- Renal cell carcinoma metastases
- Lung cancer metastases
- Multiple myeloma

Summary
When interpreting a lumbar spine X-ray, remember the following key points:
- Begin by confirming the patient’s details, reviewing the clinical history and ensuring the radiographs are adequate
- Compare to previous X-rays where possible to provide additional context.
- Assess alignment of the vertebral bodies and spinous processes carefully for inconsistencies indicative of underlying pathology (e.g. fracture)
- Inspect for loss of vertebral height which may be indicative of a vertebral fracture.
- Inspect the vertebral spaces: in healthy individuals, the disc height should gradually increase from superior to inferior.
- Inspect the vertebral endplates: the continuity of superior and inferior endplates should remain uninterrupted.
- Trace the posterior elements including pedicles, laminae and spinous processes.
- Inspect for signs of fracture and determine how many columns of the ‘Three Column Model’ are affected to determine fracture stability.
- Inspect for other important pathologies such as spondylosis, spondylolysis, spondylolisthesis and vertebral body lesions.
- Projectional radiography has limitations and other imaging modalities such as MRI and CT should be considered if further evaluation is required.
Reviewer
Professor James Meaney
Consultant Radiologist
St James’s Hospital, Dublin, Ireland
References
- Clinical Indications for Lumbar Spine Radiographs. Available from: [LINK].
- St. James’s Hospital, Radiology Dept 2021
- Anatomography. Adapted by Geeky Medics. Licence: [CC-SA-2.1].
- Dr Mohammad Taghi Niknejad, Radiopaedia.org, rID: 20547
- Jojo. Adapted by Geeky Medics. Spondylolisthesis in the lumbar region.
- Subramanian S, Viswanathan VK. Lytic Bone Lesions. 2020 Jun 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan–. PMID: 30969659. [Accessed 9 June 2021].