- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
What is ultrasound?
Ultrasound is a common imaging modality that allows visualisation in real-time. As such it is becoming increasingly popular on the wards for diagnosis and management purposes. You should be familiar with its operation and know in which situations it may help your clinical decision making.
What is ultrasound used for?
Ultrasound can be used for:
- Assessment of jugular venous pressure (JVP)
- Venepuncture
- Focused assessment for screening in trauma (FAST)
- Lumbar puncture
- Thoracentesis
- Paracentesis
- Evaluation of abdominal organs
- Biopsy
- Pregnancy
Ultrasound basics
How does ultrasound work?¹
1. High-frequency sound waves are transmitted from a transducer.
2. These sound waves are then reflected by different tissue types in different ways.
3. The reflected sound waves are then picked up by the ultrasound transducer.
4. The sound waves are then transformed into an image by special software.
How do tissue types differ in their reflection of sound waves?
Bones, fat and stones
Bones, fat and stones produce a hyperechoic signal.
A hyperechoic signal is bright as most ultrasound waves are reflected.
Cartilage and muscle
Cartilage and muscle produce a hypoechoic signal.
A hypoechoic signal appears dark as most waves pass through the tissue.
Fluid and fluid-filled structures
Fluid and fluid-filled structures produce an anechoic signal.
An anechoic signal appears black as there is no reflection of ultrasound waves.
Other
A shadow may be noted on an ultrasound when a hypoechoic area is located behind a hyperechoic structure.
Getting started
The first steps of performing an ultrasound involve:
- Turning on the machine (easy, but often overlooked; often a button in the upper left or right corner of the keypad).
- Entering the patient’s information (e.g. name, date of birth, hospital number).
- Selecting an appropriate ultrasound probe for the area being examined.
Probe basics
How do I know which probe I should use?
Typically there are 3 different types of ultrasound probe: linear, curvilinear and phased.
Linear probe:
- High frequency (7-15MHz):
- High resolution but superficial (1-6cm) depth
- Good for vascular access, nerve blocks, assessment of testes and superficial lung tissue
Curvilinear:
- Low frequency (2-5MHz)
- Low resolution, but greater depth (10-20cm)
- Useful for abdominal, pelvic, obstetric and deep lung tissue
Phased:
- The lowest frequency (1-3MHz)
- Useful for echocardiography
How do I hold the probe?
The image below demonstrates how to appropriately hold an ultrasound probe.

Probe orientation
Typically, there is a dot or a cross on the probe, this correlates with a dot on the left side of the screen.
This marker should be toward the patient’s right in transverse and head in longitudinal.
If you are unsure, it is best to place your finger on one side of the probe and look for movement on the screen (the side that shows movement by the dot is the side that should face the patient’s right).
Next steps
Once you’ve chosen an appropriate probe and are holding it right, the next steps of performing an ultrasound involve:
- Applying gel to the probe and patient.
- Placing the probe onto the patient and observing the images on the screen.
- Adjusting the settings to achieve an optimal view.
Common settings for achieving an optimal view
Gain:
- Adjusting the gain of an ultrasound changes the brightness of the image.
- Gain is typically controlled by a knob.
- The gain should be adjusted until fluid appears black and soft tissue appears mid-grey with some parts of the image appearing white
Depth:
- Depth measures are shown in cm on the side of the ultrasound monitor.
- It is often best to begin deep to orientate yourself and then work more superficially to bring the object of interest into the middle of the screen.
General tips for achieving an optimal view
Some general tips for achieving an optimal view include:
- Use lots of gel
- Make good contact between the probe and skin (whilst ensuring the patient is comfortable)
- Dim the lights to improve your view of the monitor
- Ensure the probe is perpendicular to the skin
Measuring the JVP with ultrasound
1. Position your patient as you would when assessing the jugular venous pressure (JVP) in a clinical exam (e.g. supine, head of the bed at 45°, patient’s head laterally rotated to the side not being scanned)
2. Set the gain of the ultrasound to mid-range.
3. Apply gel to the patient’s neck.
4. Place the probe in a transverse orientation within 2cm of the clavicle.
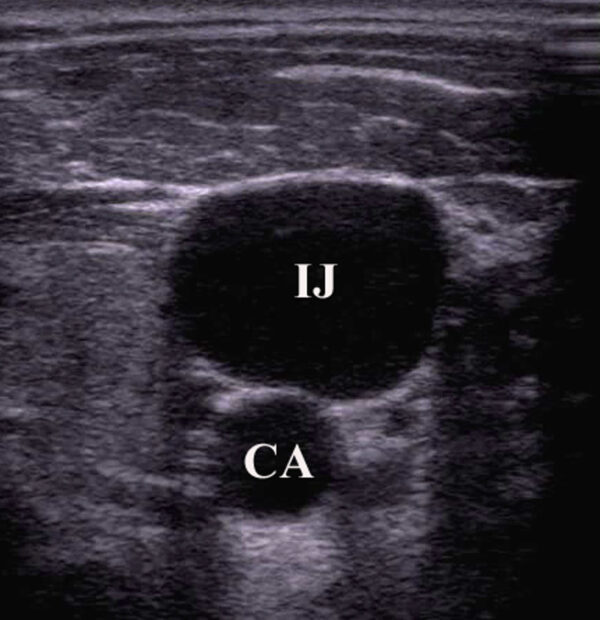
5. Identify the internal jugular vein (IJV) and the carotid artery, assessing the following:
- Wall thickness: arteries have thicker more muscular walls than venous structures.
- Shape: the carotid will be circular whereas the IJV can be oval or irregularly shaped.
- Compressibility: veins are easily compressed (if you only see one vessel, use less pressure as you may have fully compressed the IJV).
- Respiratory variability: central venous structures will fluctuate in size with respiration.
- Position: the IJV is usually (but not always) lateral to the carotid.
6. Centre the probe so the IJV is centred on the monitor.
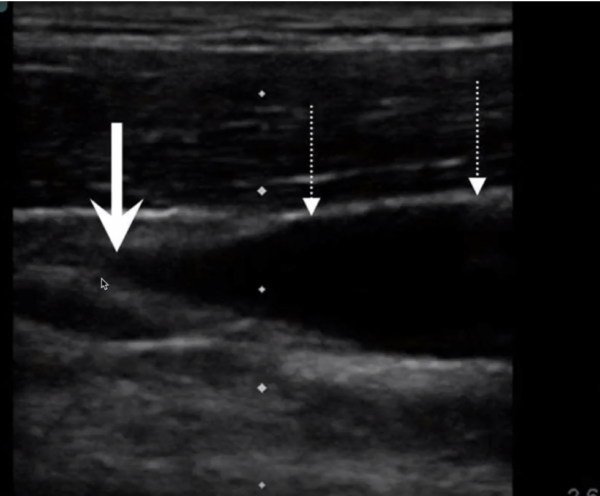
7. Slowly rotate the probe keeping the IJV in the centre until a sagittal view is achieved (ensure you are not foreshortening the vein by carefully moving the probe medially and laterally).
8. Locate the point of the initial collapse of the IJV (centre the probe over this point).
9. Measure the JVP height above the sternal angle as normal.
Ultrasound-guided intravenous access
In this section, we will be focusing on peripheral intravenous access, however, similar principles are applied for central venous line insertions.5,6
Indications
Indications for ultrasound-guided intravenous access include:
- Multiple failed attempts
- History of difficult cannulation
Contraindications
Ultrasound-guided IV access should not supplant intraosseous (IO) access in life-threatening situations.
Probe choice
A high frequency (5-12 MHz) linear transducer is typically used as high frequency permits a better resolution of structures close to the surface of the skin
A lower frequency curved probe may be more effective in obese patients.
Steps
1. Select a vein (as per non-ultrasound guided peripheral IV placement).
2. Machine set up:
- Turn on
- Choose appropriate examination pre-set: typically “peripheral vascular venous” or “superficial vascular, venous”
3. Clean the ultrasound probe.
4. Apply a tourniquet.
5. Apply gel to the ultrasound probe.
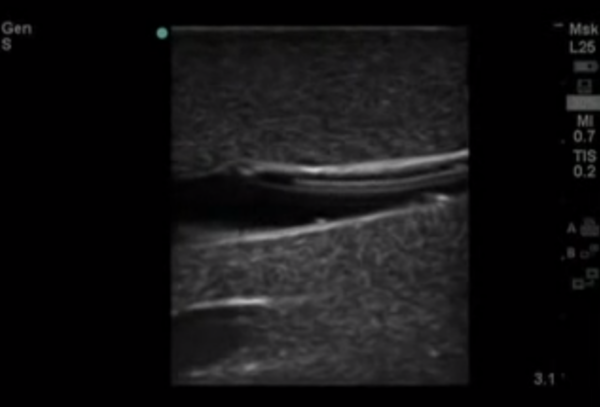
6. Identify the target vein in the transverse plane: note the depth of the anterior wall of the vein and pay attention to any adjacent structures.
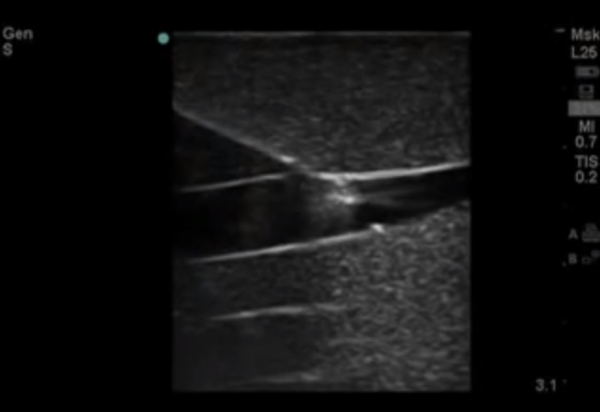
7. Once identified, rotate the probe into the longitudinal plane. Hold the probe with the thumb, index, and middle fingers as shown, using the remaining fingers as an anchor.

8. Clean the patient’s skin.
9. Align the needle prior to insertion.
10. Insert the needle just distal to the transducer probe:
- You should be able to see the needle throughout the procedure on the screen, if you cannot, you must realign.
- You can gently rock the probe to help see the flash of the needle tip if needed.
- Do not advance the needle unless you are able to clearly see the tip.
11. Advance the needle into the vein.
12. Hold the needle still and watch as you advance the catheter into the vein.
Common pitfalls
Common pitfalls for ultrasound-guided intravenous access include:
- Applying too much pressure and thus collapsing the vein.
- Choosing suboptimal settings on the ultrasound machine.
Focused assessment with sonography for trauma (FAST)
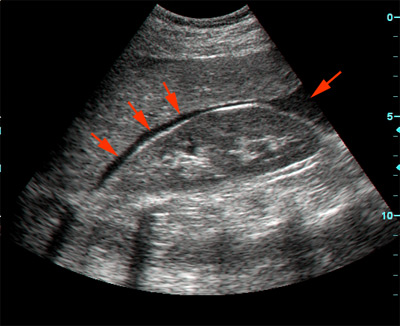
FAST is used in emergency settings to rule out free fluid in the abdomen as well as pericardial effusions using a curvilinear probe.
As discussed previously, fluid shows up as black, so the scanning clinician is inspecting for black lines surrounding organs.
Probe locations
The key probe locations for FAST are:
- Right upper quadrant
- Left upper quadrant
- Suprapubic region
- Sub-xiphoid region
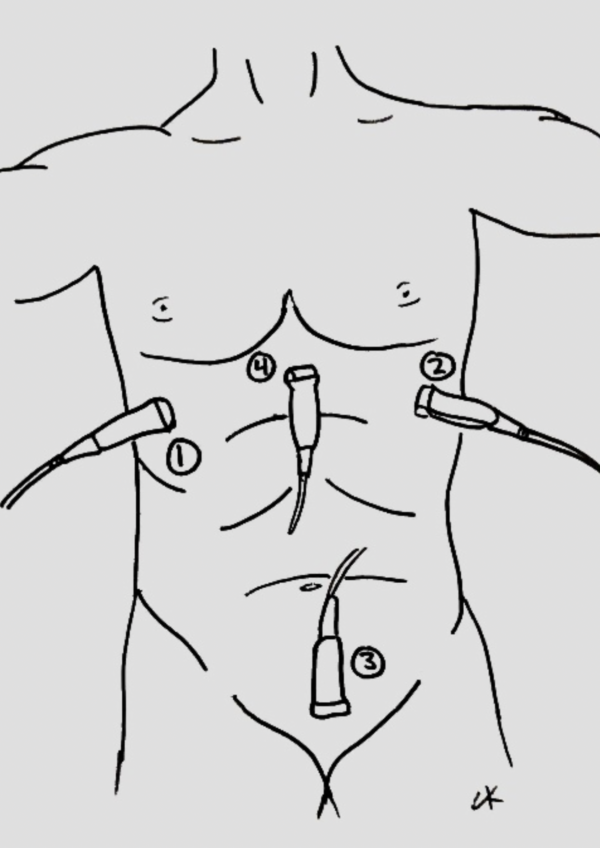
Right upper quadrant view (Morison’s pouch)
The ultrasound probe is positioned in the coronal plane in right mid-axillary line (between rib 11 and 12).
Once positioned correctly, the ultrasonographer inspects for evidence of free fluid between the liver and the kidney.
Ribs are often in the way; so the probe often requires some tilting/rotating to align it with an intercostal space.
Left upper quadrant view (perisplenic view)
Similar to Morison’s pouch, but the transducer is placed approximately half a probe length more superior and posterior (as the left kidney is more superior and posterior than the right).
The ultrasonographer inspects for free fluid between the kidney and spleen.
Cardiac view
The ultrasound probe is positioned in the transverse plane, within the sub-xiphoid region (with the probe aimed at the heart).
The ultrasonographer inspects for evidence of pericardial effusion.
Pelvic view (suprapubic)
The ultrasound probe is positioned in the suprapubic region, pointing towards the bladder.
The ultrasonographer inspects for free fluid outside of the bladder.
Both transverse and longitudinal images are typically assessed.
References
- Toronto Notes 2016: Medical Students Essential Med Notes.
- Clay Kurtz (Author’s own work)
- Emergency Ultrasonography. Resources and Tutorials on EM Ultrasound. Available from: [LINK].
- Canadian Internal Medicine Ultrasound (CIMUS). Available from: [LINK]
- Joing S, Strote S, Caroon L, et al. Ultrasound-guided peripheral IV placement. N Engl J Med. 2012;366(25):e38.
- UpToDate. Principles of ultrasound-guided venous access. Jeremiah J Sabado, MD and Mauro Pittiruti, MD. Available from: [LINK].
- Ltyore. Morison’s pouch. Public Domain.
- The POCUS Atlas. Available from: [LINK].




