- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Hip X-rays are a frequently requested radiological investigation and the ability to interpret them is a key clinical skill. It should be noted that projectional radiography has limitations and other imaging modalities such as MRI and CT should be considered if further evaluation is required.
Some salient points to remember when interpreting any radiological scan include:
- Apply a systematic approach to interpretation
- Consider abnormalities in the broader clinical context of the specific patient
For the purpose of this article, we will concentrate on a systematic approach to interpreting hip X-rays with an antero-posterior (AP) view, which is the commonest and most likely to be presented to you in an exam situation.
Confirm details
Begin by confirming you have the correct patient and the correct radiograph by assessing the following:
- Patient details (name, date of birth, unique identification number)
- Date and time the radiograph was taken
- Anatomical site (e.g. left hip)
If previous radiographs are available, these should also be reviewed to provide a point of reference.
Views
There are two standard projections produced when a hip X-ray is performed:
- Antero-posterior (AP) view
- Lateral view (a.k.a. ‘frog leg view’)
Antero-posterior view
The AP view obtains a view of the whole pelvis, usually from the femoral shaft to above the ilium. The patient is either standing or supine, and usually, have both legs internally rotated so as not to obscure the femoral neck length.
Lateral view
The lateral view has the patient lying supine in a frog-leg position; the patient’s knees are flexed, with their hip abducted and externally rotated. This view is often used in paediatric patients for pathologies such as slipped upper femoral epiphysis (SUFE) and developmental dysplasia of the hip (DDH).
Interpretation (ABCS)
It is important to apply a systematic approach to the interpretation of any X-ray; a commonly used approach with musculoskeletal imaging is ABCS:
- Adequacy/alignment
- Bones
- Cartilage (and joint spaces)
- Soft tissue
Adequacy and alignment
Adequacy
Ensure the appropriate anatomy is visible within the borders of the image: usually above iliac crests to one-third down the femoral shaft.
Alignment
Ensure that the coccyx tip and pubic symphysis are in the midline.
Follow-up imaging
Not all hip fractures are visible on initial X-ray and follow-up cross-sectional imaging may be required if there is ongoing clinical concern.
Bones
General approach
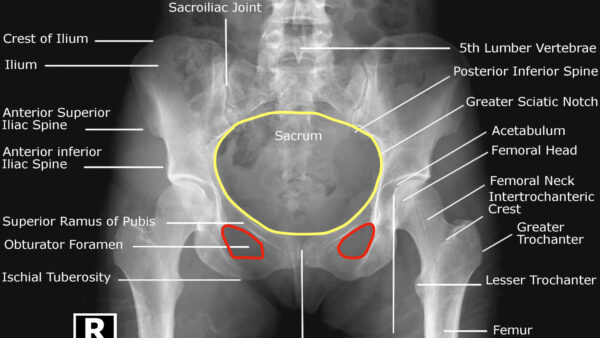
Assess the following characteristics of both the femur and visible pelvis:
- Cortical outline: identifying any bony fragments or fractures
- Bony texture: including trabecular lines of the femur that may indicate joint disruption
- Symmetry: absence of symmetry can allow identification of subtle abnormalities
Femur
Inspect all visible elements of the femur including:
- Proximal femur
- Femoral head
- The neck of the femur (NOF)
- Greater and lesser trochanters
Trace Shenton’s line (Figure 3):
- Shenton’s line runs anatomically along the medial edge of the femoral neck and the inferior edge of the superior pubic ramus (Figure 3).
- Interruption of Shenton’s line may suggest a neck of femur (NOF) fracture in adults or DDH in children.
It is important to note that loss of contour of Shenton’s line does not always mean there is an underlying fracture (and so an intact Shenton’s line does not always rule out a NOF fracture), and thus should be used with caution when interpreting pelvic X-rays.

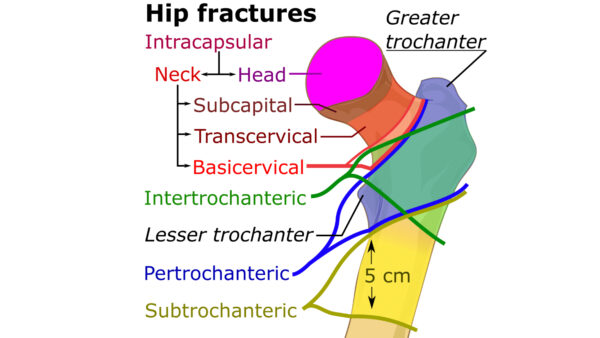
Intracapsular vs extracapsular fractures
It is important to understand the difference between intracapsular and extracapsular fractures (Figure 4), as the management and prognosis differ significantly.
Intracapsular fractures
Intracapsular fractures are located at the neck of the femur (NOF):
- Sub-capital (just distal to femoral head – Figure 5)
- Transcervical (mid-femoral neck)
- Basicervical (distal femoral neck at the NOF base)
This fracture type disrupts the joint capsule and therefore potentially the blood supply to the femoral head (branches of the profunda femoris, most importantly the lateral circumflex arteries).
This means there is a higher chance of avascular necrosis (AVN) as well as fracture non-union/poor healing.
Remember that AVN is not just limited to NOF fractures, highlighting the importance of clinical context (e.g. long-term steroid use can result in spontaneous avascular necrosis).
Extracapsular fractures
Extracapsular fractures do not involve the neck of the femur and are located below the intertrochanteric line:
- Intertrochanteric (fracture runs between the lesser/greater trochanters)
- Subtrochanteric (fracture is distal to the trochanters)
Pelvic bones
Assess the pelvic bones including the:
- Ischium
- Ilium
- Pubis (including pubic rami)
- Sacrum (including sacral foramina)
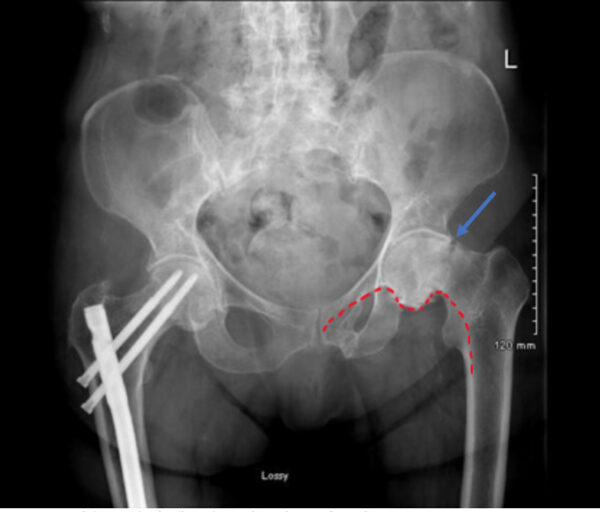
Trace the borders of the 3 pelvic rings (Figure 6):
- Pelvic brim
- Obturator foramina (x2)
Comment on the continuity of the borders of these rings; remember, the rings are unlikely to be broken in only one place.
Pubic rami fractures are sometimes diagnosed in elderly patients who have fallen and present with non-specific ‘hip pain’ and/or difficulty mobilizing. These can be quite subtle on a hip X-ray and therefore systematic assessment is essential (Figure 7).
Bony metastases
Bony metastases are most commonly found in areas of bone with a rich blood supply such as the pelvis, vertebrae, proximal femur, proximal humerus and skull. Bony metastases can promote local bone formation, resulting in sclerotic areas on X-ray (i.e. increased opacity) as well as bone resorption, resulting in lytic areas on X-ray (i.e. decreased opacity).

Cartilaginous joints
Acetabular joint
Assess the characteristics of the acetabular joint including:
- Location of the femoral head in relation to the acetabulum (e.g. dislocation)
- Joint space (typically 3-5mm)
Osteoarthritis
Osteoarthritis commonly affects the hip joint, so it is worth looking for typical radiographic features of the disease including:
- Reduced joint space
- Osteophytes (small bony outgrowths)
- Subchondral sclerosis (sclerotic changes at the joint margin)
- Subchondral cysts (fluid-filled cysts – most commonly occur in the femoral head)
Pubic symphysis
Assess the joint space of the pubis symphysis which differs depending on age:
- ~10 mm at 3 years
- ~6 mm at 20 years
- ~3 mm at 50 years
During pregnancy, the joint space can increase by up to 3mm as a result of hormones such as relaxin to assist with childbirth.
Pubic diastasis
Pubic diastasis involves separation of the pubic symphysis without associated fracture. Typical clinical features include pain in the symphyseal region aggravated by weight-bearing/walking and a waddling gait. A joint space of greater than 10mm is considered diagnostic in adults.
Sacroiliac joint
Assess the characteristics of each sacroiliac joint including:
- Joint space (should be 2-4mm in healthy individuals)
- Joint end-plates (should appear smooth/regular)
Sacroiliitis
Sacroiliitis involves inflammation of one or both sacroiliac joints and typically presents with buttock and/or lower back pain. The condition is typically associated with ankylosing spondylitis.
X-ray has low diagnostic sensitivity, but potential radiographic features include:
- Sclerosis of the endplates particularly on the iliac side
- Irregular joint end plates
- Widening of joint spaces

Soft tissue & other
Inspect the soft tissue surrounding the bones and joints for:
- Effusion: hyperdensity, fluid-level (e.g. inflammatory joint disease)
- Periosteal reaction: nonspecific radiographic finding that indicates periosteal irritation (e.g. healing fracture, bone tumour)
- Calcification of soft tissues (e.g. phleboliths, panniculitis, atherosclerotic vascular calcifications)
- Foreign bodies (e.g. total hip replacement)
Summary
When interpreting a hip X-ray, remember the following key points:
- Begin by confirming the patient’s details, reviewing the clinical history and checking the radiographs are of the correct anatomical site (e.g. left hip).
- Compare the images to previous radiographs where possible to provide additional context.
- Assess the adequacy of the radiograph (above iliac crests to one-third down the femoral shaft).
- Assess the alignment of the radiograph (e.g. location of the tip of the coccyx and pubic symphysis).
- Inspect the femur and bones of the pelvis (ischium, ilium, pubis, sacrum) for abnormalities including interruptions to the cortical outline, changes to the bony texture or asymmetry.
- Inspect the acetabular joint for abnormalities including displacement of the femoral head or loss of joint space.
- Inspect the joint space of the pubic symphysis for widening (e.g. pubic diastasis).
- Inspect the sacroiliac joints for loss of joint space and changes to joint-end plates (e.g. sacroiliitis).
- Inspect the soft tissues that surround the hip joint for abnormalities such as effusion, periosteal reaction, calcification or foreign bodies.
- Projectional radiography has limitations and other imaging modalities such as MRI and CT should be considered if further evaluation is required.
References
- Wikiradiography.net. Adapted by Geeky Medics. Pelvic radiographic anatomy.
- Wikiradiography.net. Adapted by Geeky Medics. Shenton’s line example.
- Mikael Häggström. Adapted by Geeky Medics. Classification of hip fractures.
- St. James’s Hospital, Radiology Dept 2021
- James Heilman, MD. Adapted by Geeky Medics. Superior & inferior pubic rami fractures. Licence: CC BY-SA 4.0. Available from: [LINK].
- James Heilman, MD. Adapted by Geeky Medics. Bony metastases in the pelvis. Licence: CC BY-SA 3.0. Available from: [LINK].
- Nevit Dilmen. Adapted by Geeky Medics. Sacroiliitis. Licence: CC BY-SA 3.0. Available from: [LINK].