- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
This nasogastric (NG) tube insertion guide provides a step-by-step approach to performing NG tube insertion in an OSCE setting with an included video demonstration.
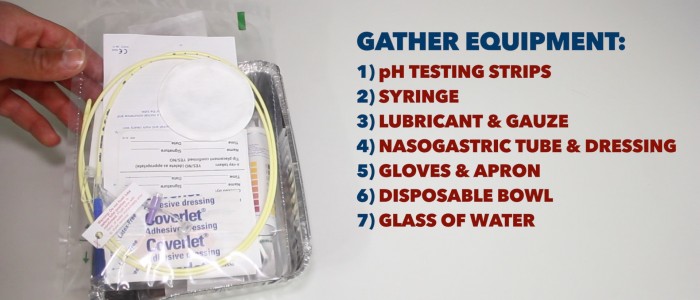
Gather equipment
Gather the relevant pieces of equipment and place into a tray:
- Nasogastric tube (fine bore)
- Disposable gloves
- Lubricant and gauze: to lubricate the tip of the NG tube.
- Disposable bowl: to be used in the event of vomiting.
- Paper towels: to allow the patient to wipe around their mouth if needed.
- Large syringe: to obtain an aspirate from the NG tube.
- pH testing strips: to assess the pH of the aspirate.
- Dressing: to secure the NG tube.
- A glass of water for the patient (if swallow is deemed safe).
- Local anaesthetic spray: to numb the oropharynx.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the procedure will involve using patient-friendly language: “At the moment you’re having trouble swallowing food in the normal way. Because of this, we need to place a fine tube through your nose going into your stomach to allow us to provide you with nutrition. The procedure will be uncomfortable, but it shouldn’t be painful or take very long. If at any point it becomes too uncomfortable and you want me to stop, just tap on my arm.”
Gain consent to proceed with NG tube insertion.
Check if the patient has any allergies (e.g. latex).
Ask the patient if they have any pain before continuing with the clinical procedure.
Position the patient sitting comfortably on a chair or bed.
If a patient has suffered head trauma and a base of skull fracture has not been ruled out, NG tube insertion should be avoided due to the potential risk of entering the cranial vault.
Measurement of the insertion length
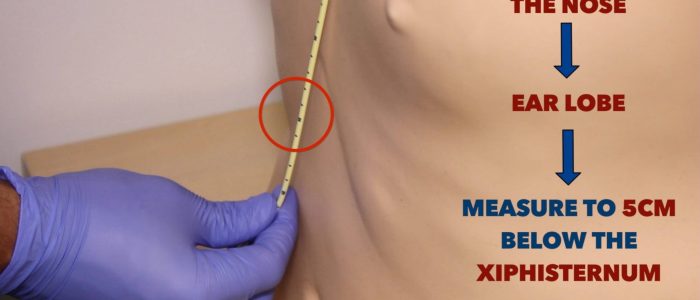
1. Position the patient sitting upright with their head in a neutral position.
2. Don a pair of non-sterile gloves.
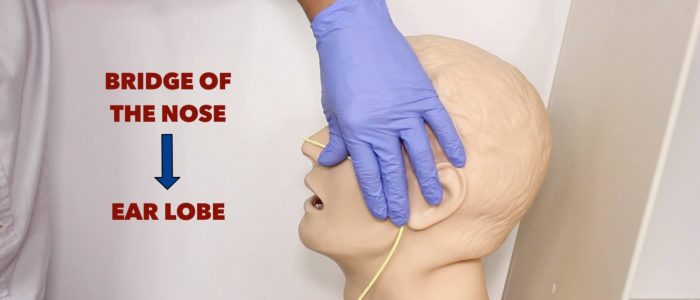
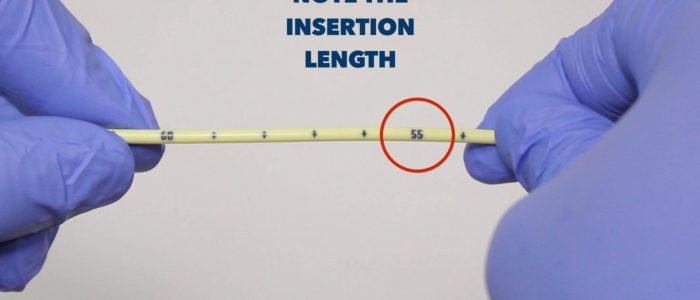
3. Estimate how far the NG tube will need to be inserted: measure from the bridge of the nose to the ear lobe and then down to 5cm below the xiphisternum.
Insertion of the NG tube
1. Lubricate the tip of the NG tube.
2. If available, a local anaesthetic should be sprayed towards the back of the patient’s throat.
3. Warn the patient you are about to insert the NG tube.
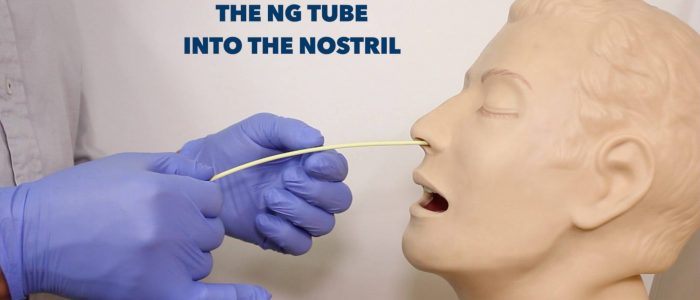
4. Insert the NG tube through one of the patient’s nostrils.
5. Gently advance the NG tube through the nasopharynx:
- This is often the most uncomfortable part for the patient.
- If resistance is met, rotating the NG tube can aid insertion. Avoid forcing the NG tube if significant resistance is encountered.
- If the patient becomes distressed, pause to give them some time to recover.
- Intermittently inspect the patient’s mouth to ensure the NG tube isn’t coiling within the oral cavity.
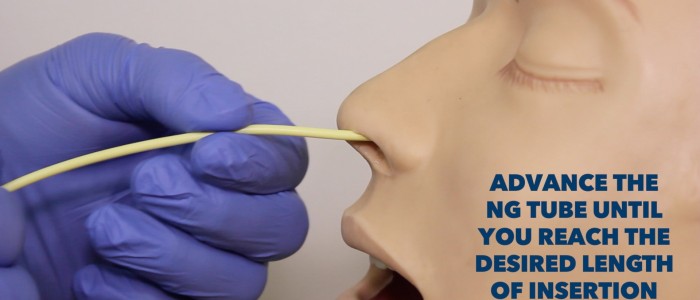
6. Continue to advance the NG tube down the oesophagus: ask the patient to take some sips of water and then swallow as this can facilitate the advancement of the NG tube. Avoid giving patients a drink if their swallow is deemed unsafe, due to the risk of aspiration.
7. Once you reach the desired nasogastric tube insertion length, fix the NG tube to the nose with a dressing.
Aspiration of the NG tube
1. Attempt to aspirate gastric contents:
- If aspiration is successful, test the pH: a value of <4 suggests correct placement.
- If aspiration is unsuccessful or the pH is >4 the patient will require a chest x-ray (CXR).
- Some hospitals require a CXR regardless of pH, so check your local guidelines.
- Acceptable pH ranges also vary between hospitals, so always check your local guidelines.
2. Once the NG tube is deemed safe for use, the radiopaque guidewire can be removed.
To complete the procedure…
Explain to the patient that the procedure is now complete and reassure them that the NG tube will become more comfortable over the next few hours.
Thank the patient for their time.
Offer the patient paper towels to clean their face and nose.
Dispose of used equipment, including PPE, into a clinical waste bin.
Wash your hands.
Let the nursing staff know if the NG tube is currently safe to use.
Document the details of the procedure in the patient’s notes:
- Your personal details including your name, job role and GMC number.
- The date and time the procedure was performed.
- Confirmation that verbal consent was obtained.
- The indication for NG tube insertion.
- The insertion length of the NG tube.
- The pH of the aspirate or the failure to obtain an aspirate.
- CXR interpretation (if performed): “NG tube visible dissecting the carina and sitting below the left hemidiaphragm”.
- Any complications experienced during the procedure.
- Whether the NG tube is currently safe to use.
Reviewer
Dr Ally Speight
Consultant Gastroenterologist