- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Otitis externa (OE) is defined as inflammation of the external ear canal.1 It is estimated to affect 1% of the UK population each year.2 OE can be classified by the duration of symptoms:
- Acute: <3 weeks
- Chronic: >3 weeks
All ages can be affected; a study in General Practice demonstrated the highest incidence in patients aged 7-12 years, with a declining incidence in those over 50 years old.2 The same study demonstrated seasonal variation, with an increased presentation of OE in late summer, possibly due to warmer temperatures, increased humidity or more frequent exposure to water.2
Aetiology
The aetiology of otitis externa can be broken down into infectious and non-infectious causes.
Infectious
Bacterial
- Account for 90% of infections3
- Results from an overgrowth of bacteria in the external ear often due to increased moisture in the ear canal (e.g. increased humidity, swimming, perspiration) and/or local trauma to the ear canal which allows bacteria to enter through a break in the skin (e.g. use of cotton buds, itching).
- Most common pathogens are Pseudomonas aeruginosa or Staphylococcus aureus.
Fungal (otomycosis)
- Account for 10% of infections3
- Usually follow prolonged and extensive use of topical antibiotics with or without corticosteroids
- Most common pathogens are Candida albicans and Aspergillus niger
*Mixed bacterial and fungal infections are also common
Non-infectious
- Commonly caused by skin conditions such as atopic dermatitis, psoriasis and acne.
- These can both predispose to the development of OE by leading to breaks in the skin barrier, resulting in secondary bacterial infection, and also be the sole cause of otitis externa.
Risk factors
- Hot and humid climates
- Swimming
- Older age
- Dermatological issues (e.g. eczema)
- Narrow ear canals (e.g. Down’s syndrome)
- Previous ear surgery
- Previous radiotherapy to the head and neck
- Any history of immunosuppression including diabetes
- Previous topical treatments for otitis externa or otitis media
Clinical features
History
Typical symptoms of OE include:
- Ear pain
- Discharge
- Itch
- Hearing loss
- Fever
Other important areas to cover in the history include:
- Recent trauma to the ear.
- Exposure to water or humidity (e.g. swimming).
- Use of hearing aids or earplugs.
- Past medical history (e.g. eczema, ear canal issues).
Examination4
A thorough clinical examination for otitis externa needs to include:
- Examination of the external ear canal
- Otoscopy
- Hearing assessment (gross assessment including tuning fork tests)
- Assessment of regional lymph nodes
- Cranial nerve examination if concerns about necrotising otitis externa.
Examination of the external ear canal
Typical findings:
- Skin changes or tenderness at the tragus or pinna.
- Erythema, oedema and narrowing of the ear canal which may progress to complete occlusion.
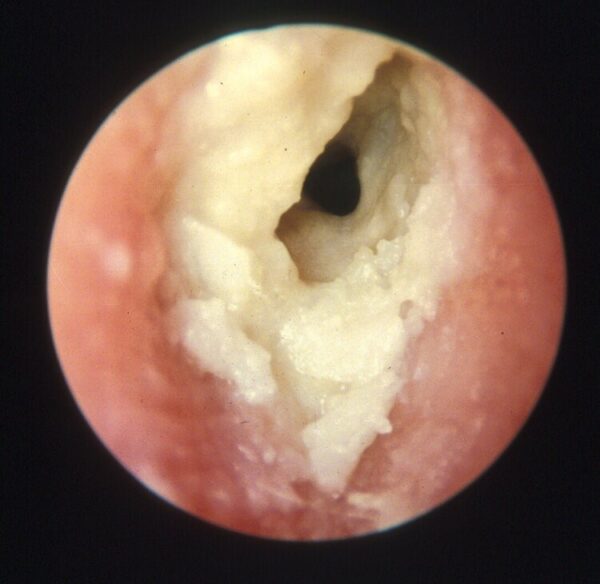
- Serous or purulent discharge (Figure 1).
Otoscopy
Typical findings:
- Inflammation of the tympanic membrane which may be difficult to visualise due to ear canal stenosis.
Regional lymph nodes
Typical findings:
- Regional lymphadenopathy in the pre/post-auricular nodes.
Hearing assessment
Typical findings:
- Tuning fork tests may demonstrate a conductive hearing loss secondary to obstruction of the ear canal with oedema and/or debris. See the Geeky Medics guide here.
Cranial nerve examination
- Consider neurological assessment including full cranial nerve exam if there is clinical suspicion of necrotising otitis externa.
- Necrotising otitis externa can cause cranial nerve palsy (e.g. facial nerve palsy).
- See the Geeky Medics guide for cranial nerve examination here.
Differential diagnoses
Several conditions can mimic OE, such as acute otitis media with a tympanic membrane rupture resulting in otorrhoea. Similarly, dermatological conditions such as eczema can be mistaken for OE. The most important diagnosis of exclusion is necrotising otitis externa (NOE), a serious complication of OE (more details in the complications section).
Investigations
The diagnosis of OE is largely based on clinical findings from both the history and clinical examination. However, it may, in some cases, be useful to take microbiology swabs of any ear discharge prior to initiating treatment.
Management
General advice
- Advise strict water precautions to keep the ear dry. One suggestion is to roll a ball of cotton wool in Vaseline and gently place this in the conchal bowl when bathing to prevent water from entering the ear canal.
- Avoid itching or using cotton buds which further traumatise the ear canal.
Medical management
Prescribe topical antibiotic ear drops according to local policy:
- Topical treatments usually contain an antibiotic +/- steroid
- No evidence to suggest which product is most effective5
- Avoid using aminoglycosides in patients with a perforated tympanic membrane in the first instance; quinolone containing preparations can be used as an alternative.
- Treatment is administered for a minimum of 7 days but if symptoms persist the topical antibiotic course may be extended up to a maximum of 14 days, after which ear swab microbiology sensitivities or ENT opinion should be sought if there is no improvement.
Oral antibiotics are not effective in the majority of cases but may be considered in the following circumstances:4
- Cellulitis extending beyond the external ear canal
- People with compromised immunity and/or severe infection
- If recommended by ENT
Analgesia should be prescribed based on the severity of pain, however, the most significant reduction in pain occurs once the ear canal inflammation begins to resolve, which may take two to three days after starting topical therapy.
Further management
Some patients will continue to experience symptoms despite adequate primary care management and should be referred to ENT for assessment:
- ENT can perform microsuction to physically remove infected debris from the canal and can insert an otowick in patients whose ear canals are acutely stenosed or occluded due to inflammation. An otowick is a small tube of dry sponge that can be inserted into the external meatus. It expands on contact with fluid, enabling drops to be instilled deeper into the canal to improve treatment efficacy.
- Patients with possible OE complications should be referred to ENT for assessment.
Follow-up
Patients with recurrent episodes of acute OE often benefit from general advice to reduce their risk, including:
- Avoiding the use of cotton buds or insertion of foreign objects into the ear canal
- Applying strict water precautions long term
- Using occlusive earplugs if swimming
- Seeking treatment for underlying skin conditions
Complications
Complications of OE are uncommon, but can be serious and should, therefore, be considered in patients who do not respond to treatment and in those with known risk factors as above.
Necrotising otitis externa (NOE)
- The infection spreads beyond the soft tissue of the ear canal resulting in osteomyelitis of the temporal bone and skull base. 6
- Characterised by non-resolving otitis externa despite adequate topical treatment.
- There may be evidence of exposed bone or granulation tissue on the floor of the canal on examination.
- The diagnosis is made in cases with a high index of clinical suspicion and evidence of bony erosion on imaging.
- Pseudomonas aeruginosa is the most common causative organism.
- Patients are typically older and diabetic, with severe unremitting otalgia out of proportion to the examination findings.
Pinna or peri-auricular cellulitis
- Presents with painful erythema, warmth and swelling of the skin on or around the pinna, which may extend to surrounding tissues overlying the parotid gland, mastoid and sternomastoid.6
- Systemic features such as fevers, generalised illness and regional lymphadenopathy may be present.
Risk factors for complications
- Diabetes mellitus
- Age >65 years
- Recurrent otitis externa
- Immunosuppression (e.g. chemotherapy, chronic kidney disease)
- Radiotherapy to the head or the neck
Prognosis
- The majority of cases will improve within 48 – 72 hours of treatment initiation.
- Between 65 – 90% of patients with uncomplicated OE have clinical resolution within 7 – 10 days, regardless of the topical treatment used.1
Key points
- OE is a common condition involving inflammation of the ear canal.
- The most common cause is a bacterial infection with Pseudomonas aeruginosa or Staphylococcus aureus.
- Diagnosis is largely made based on clinical findings alone.
- Primary care management consists of preventing further trauma to the ear canal, applying strict water precautions, the use of topical antibiotic +/- steroid ear drops and provision of adequate analgesia.
- Some patients will require referral to ENT for consideration of aural microsuction, insertion of an otowick or for further assessment of suspected complications.
- Necrotising otitis externa should be considered in patients with diabetes or underlying immunosuppression who do not respond to topical treatment.
References
- Rosenfeld RM et al. Clinical Practice Guideline. Published in 2014. [LINK]
- Rowlands S et al. A. Otitis externa in UK general practice: A survey using the UK General Practice Research Database. Published in 2001. [LINK]
- Osguthorpe JD, Nielsen DR Otitis externa: Review and clinical update. Published in 2006. [LINK]
- NICE. Otitis externa – NICE CKS. Published in 2018. [LINK].
- Kaushik V et al. Interventions for acute otitis externa. Published in 2010. [LINK]
- ENT SHO. Complications of Otitis Externa — entsho.com. Published in 2019. [LINK].
- ENT SHO. Acute Otitis Externa. © AS Lau. [LINK]
Reviewer
Louise McMurran
ENT Registrar
Editor
Hannah Thomas




