- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Background
Postural hypotension, also known as orthostatic hypotension, is defined as a sustained reduction in systolic BP of at least 20mmHg, or diastolic BP of 10mmHg, that occurs within three minutes of standing.1 It is a significant contributor to morbidity and adverse events in older adults. In the community, the prevalence of postural hypotension in adults aged over 65 is estimated to be approximately 16%; however, can be as high as 50% for those living in organized spaces such as care homes.2 This article aims to provide an overview of postural hypotension, with a special emphasis on relevant considerations for adults aged 65 and above. The pharmacological and non-pharmacological approaches to managing postural hypotension will be discussed as well.
Physiology of postural hypotension
When we stand, blood shifts from the chest to below the diaphragm. This fluid shift reduces venous return, which reduces the filling of the ventricles in the heart. This decrease in preload thereby reduces cardiac output. This causes a reduction in blood pressure.3
The gravity-induced reduction in blood pressure is detected by baroreceptors in the aortic arch and carotid sinus. These baroreceptors trigger baroreflexes, including vasoconstriction and compensatory tachycardia in an attempt to restore blood pressure (Figure 1). There is an increase in sympathetic outflow and a decrease in vagal nerve activity; thereby reducing parasympathetic stimulation to the heart.1 The baroreceptors also send signals to the arterioles and venules in the circulatory system to increase total peripheral resistance.3 These measures overall work to increase and thus normalise blood pressure.
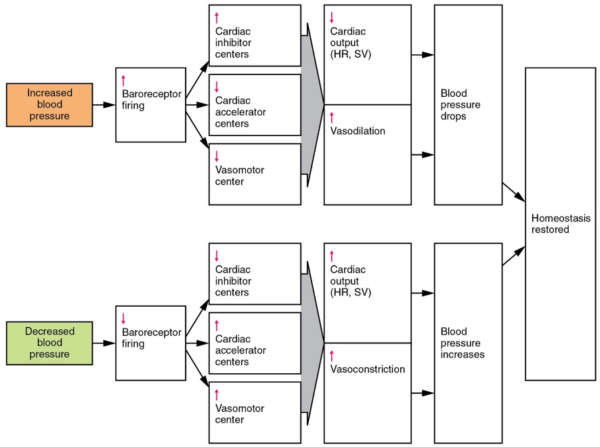
Postural hypotension occurs when these mechanisms to regulate blood pressure are impaired. The body is unable to maintain the same blood pressure on sitting up or standing.
Postural hypotension can occur due to one or more of the following:
- Failure of baroreflexes (autonomic failure)
- Volume depletion
- End-organ dysfunction5
Causes of postural hypotension
There are several underlying causes of postural hypotension. It is useful to break them down into neurogenic vs. non-neurogenic aetiologies.
Neurogenic
Neurogenic hypotension occurs when there is an insufficient release of noradrenaline from the sympathetic vasomotor neurons. This limits vasoconstriction, and so the body is unable to increase and normalise blood pressure on standing or sitting up.2 Neurogenic hypotension is most often seen in disorders that cause autonomic dysfunction including:
- Type 2 diabetes mellitus
- Parkinson’s disease
- Small cell lung carcinoma, monoclonal gammopathies, light chain disease, or amyloid. If a patient presents with a subacute onset of postural hypotension that is rapidly progressing, these conditions that cause autonomic failure need to be ruled out.1
Non-neurogenic
Non-neurogenic postural hypotension fundamentally arises from either hypovolaemia, cardiac failure or venous pooling.5
- Cardiac impairment (this includes myocardial infarction and aortic stenosis)
- Reduced intravascular volume (dehydration, adrenal insufficiency)
- States that induce vasodilation (including fevers)1
- Medications: It is vital to obtain a comprehensive medication history from patients presenting with postural hypotension. Common medications that can induce postural hypotension include the following:
- Diuretics
- Alpha-adrenoceptor blockers for prostatic hypertrophy
- Antihypertensive drugs,
- Insulin, levodopa, and tricyclic antidepressants can also cause vasodilation and postural hypotension in predisposed patients2
Clinical features of postural hypotension
The symptoms of postural hypotension are caused by cerebral hypoperfusion. They include:
- Dizziness
- Weakness
- Confusion
- Blurred vision
- Nausea
- In severe cases, syncope. When older patients present with syncope, a lying and standing blood pressure measurement is essential to identify postural hypotension as a potential contributor.1
Why are older adults more susceptible to postural hypotension?
Firstly, older adults are more prone to hypovolaemia. This is due to an increase in natriuretic peptides, and the reduction in renin, angiotensin and aldosterone with age. They have an impaired ability to conserve water and sodium; this is exacerbated by a diminished thirst response.5
Changes to the cardiovascular system also contribute to postural hypotension in older adults. Older adults have decreased baroreflex sensitivity, with impaired a1-adrenergic vasoconstriction and affected heart rate responses.6 Chronic hypertension, which is seen in a large proportion of adults over the age of 65, also results in reduced baroreflex sensitivity and left ventricular compliance.1 Older adults have a blunted response to the recruitment of the sympathetic nervous system in blood pressure control.6
Older adults are more likely to be on medications that are associated with inducing postural hypotension, such as furosemide and terazosin. Polypharmacy is an issue with this demographic, as many individuals will be on multiple anti-hypertensives as well.7 In parallel, older adults tend to have a higher prevalence of co-morbidities such as chronic hypertension and diabetes, which are known contributors to postural hypotension.2 Finally, older adults are more likely to experience greater severity of the symptoms from postural hypotension, due to deconditioning from lack of exercise.1
Exacerbating factors
Several factors may predispose or worsen postural hypotension. These factors need to be addressed and discussed with patients as part of the management of postural hypotension.5 Lifestyle-related factors should be discussed with patients using appropriate motivational interviewing techniques:
- Rising quickly after prolonged sitting or recumbency
- Prolonged motionless standing
- Time of day (early morning after nocturnal diuresis)
- Dehydration
- Physical exertion
- Alcohol intake
- Carbohydrate-heavy meals
- Straining during micturition or defecation
- Fever
Management of postural hypotension
It is important to consider postural hypotension as a syndrome, rather than simply emphasising and treating singular causes.
Overall, the aims of managing postural hypotension in older adults are:
- To raise standing blood pressure without also raising supine blood pressure
- To reduce orthostatic symptoms
- To increase the time the patient can stand
- To improve the ability of patients to perform activities of daily living5
In order to address these aims, the management of postural hypotension targets three main physiologic processes:
- Reducing venous pooling
- Increasing blood volume
- Increasing vasoconstriction2
Non-pharmacological management
Non-pharmacological measures are recommended as the first-line strategy in the management of postural hypotension. Firstly, education about the condition is an important aspect of management. A simple way of explaining postural hypotension to an older patient could be as follows:
“Postural hypotension is a drop in blood pressure when you sit up or stand. Normally our bodies are able to restore this blood pressure. But in postural hypotension, your blood pressure doesn’t go back to normal, which is why you may feel dizzy, nauseous or have blurry vision on standing. There are several things that can contribute to postural hypotension, such as diabetes, Parkinson’s disease and various medications. Let’s discuss some strategies to try and prevent your blood pressure from dropping so much when standing.”
Furthermore, avoidance of high-risk situations should be emphasised to patients. This includes situations include rising quickly from sitting or supine positions, prolonged standing, hot environments and large meals.6
Strategies to reduce venous pooling include the use of compression stockings and abdominal binders. These prevent backward blood flow but can be costly and uncomfortable for patients.1 Physical activity should also be encouraged wherever possible to reduce venous pooling.
In patients with enough cognition, counter-manoeuvres against postural hypotension can be taught. These include exercises such as toe raising, leg elevation and leg crossing. These involve contraction of the muscles below the waist; reducing venous capacitance, thereby increasing total peripheral resistance, and facilitating venous return to the heart.6 These countermeasures can help maintain blood pressure during activities of daily living.
Measures to expand blood volume include keeping the head of the bed elevated (reverse Trendelenburg). This increases plasma volume by decreasing overnight diuresis, with activation of the renin-angiotensin-aldosterone system.6 Increasing salt and water intake, including the use of regular boluses of water, are other possible measures to increase blood volume.8
Pharmacological management
Pharmacological management should be considered after non-pharmacological interventions have been trialled, and approached cautiously for polypharmaceutical patients. Prior to prescribing any new medication, a thorough review of the patient’s past and present medications and allergies should be performed. In this regard, you may consider stopping potential exacerbating medications.7 After this has been completed, you may consider prescribing some of the medications discussed below.
Fludrocortisone
Fludrocortisone is a synthetic mineralocorticoid that expands plasma volume.8 This medication can be useful if non-pharmacological measures and cessation of exacerbating medications have proved unsuccessful. It has demonstrated good efficacy for patients whose plasma volume fails to adequately increase with salt and bolus fluids. Fludrocortisone is contraindicated in patients who have heart failure, ascites and chronic renal failure. Side effects include supine hypertension and severe hypokalaemia, so it is vital that a patient’s potassium levels are monitored when commenced on fludrocortisone.1 Fludrocortisone can be started at 100mcg once daily in the morning.*
Midodrine
Midodrine is a vasopressor that is short-acting and can be useful in neurogenic postural hypotension.6 It has a short duration of action and the literature suggests that it can be effective when used in conjunction with fludrocortisone. However, it is largely ineffective in patients with low plasma volume.8 Caution should be exercised in patients with severe heart failure, urinary retention and underlying hypertension. Midodrine has unique side effects including supine hypertension, scalp paraesthesia and pilomotor reactions, such as goosebumps.6 Midodrine can be titrated for dosing up to three times daily, with a starting dose of 2.5mg.*
Pyridostigmine
Pyridostigmine is an acetylcholinesterase inhibitor, that can be used for postural hypotension as it has a vasoconstrictive effect only while standing. However, its effect on managing postural hypotension is modest.6 It also exacerbates supine hypertension in a dose-dependent manner.5 Pyridostigmine has a starting dose of 30mg.*
* Consult your local BNF before prescribing these medications
Complications & prognosis
Postural hypotension is a significant contributor to falls in older adults. The symptoms tend to have a tremendous impact on patients’ confidence with mobility, as well as their ability to perform the activities of daily living (ADLs) independently. It is also important to recognise that postural hypotension can be a barrier against a patient being able to live independently in their own home. The prognosis of postural hypotension is dependent on the contributing factors being identified and managed appropriately. One study found that at the 5-year follow-up, individuals with postural hypotension had significantly increased all-cause mortality by 1.5 times compared to those without postural hypotension.9 Postural hypotension is considered an independent risk factor for both mortality and cardiovascular disease.10
Take-home messages
- Postural hypotension is associated with significant morbidity and mortality in older adults
- Consider postural hypotension as a syndrome, rather than focusing on and treating singular causes
- Management should be directed at increasing blood volume, decreasing venous pooling, and increasing vasoconstriction, while minimizing supine hypertension as able.
- Patient education and non-pharmacological measures are vital aspects of managing postural hypotension and should be instituted prior to any pharmacological measures.
References
- MacDonald MJ, Clair A, Khoury L, Molnar FJ. 4D-AID: a practical approach to the assessment of orthostatic hypotension in older patients. Published in 2016. [LINK]
- Shibao C, Lipsitz LA, Biaggioni I. ASH position paper: evaluation and treatment of orthostatic hypotension. Published in 2013. [LINK]
- Lanier JB, Mote MB, Clay EC. Evaluation and management of orthostatic hypotension. American family physician. Published in 2011. [LINK]
- Roholts, N. File: Baroreceptor reflex. Published in 2020. [LINK]
- Figueroa JJ, Basford JR, Low PA. Preventing and treating orthostatic hypotension: as easy as A, B, C. Published in 2010. [LINK]
- Klair A, MacDonald MJ, Molnar FJ, Khoury L. Treatment of orthostatic hypotension in older patients: the geriatric perspective. Published in 2017. [LINK]
- Mills PB, Fung CK, Travlos A, Krassioukov A. Nonpharmacologic management of orthostatic hypotension: a systematic review. Published in 2015. [LINK]
- Ryan DJ, Cunningham CJ, Fan CW. Non-pharmacological management of orthostatic hypotension in the older patient. Published in 2012. [LINK]
- Ricci F, Fedorowski A, Radico F, Romanello M, Tatasciore A, Di Nicola M, Zimarino M, De Caterina R. Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies. Published in 2015. [LINK]
- Aronow WS. Prognosis of Orthostatic Hypotension. Published in 2016. [LINK]
Reviewer
Dr Bodhi Wimalasena
Consultant Geriatrician