- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The neurological examination helps you localise a lesion in the nervous system.
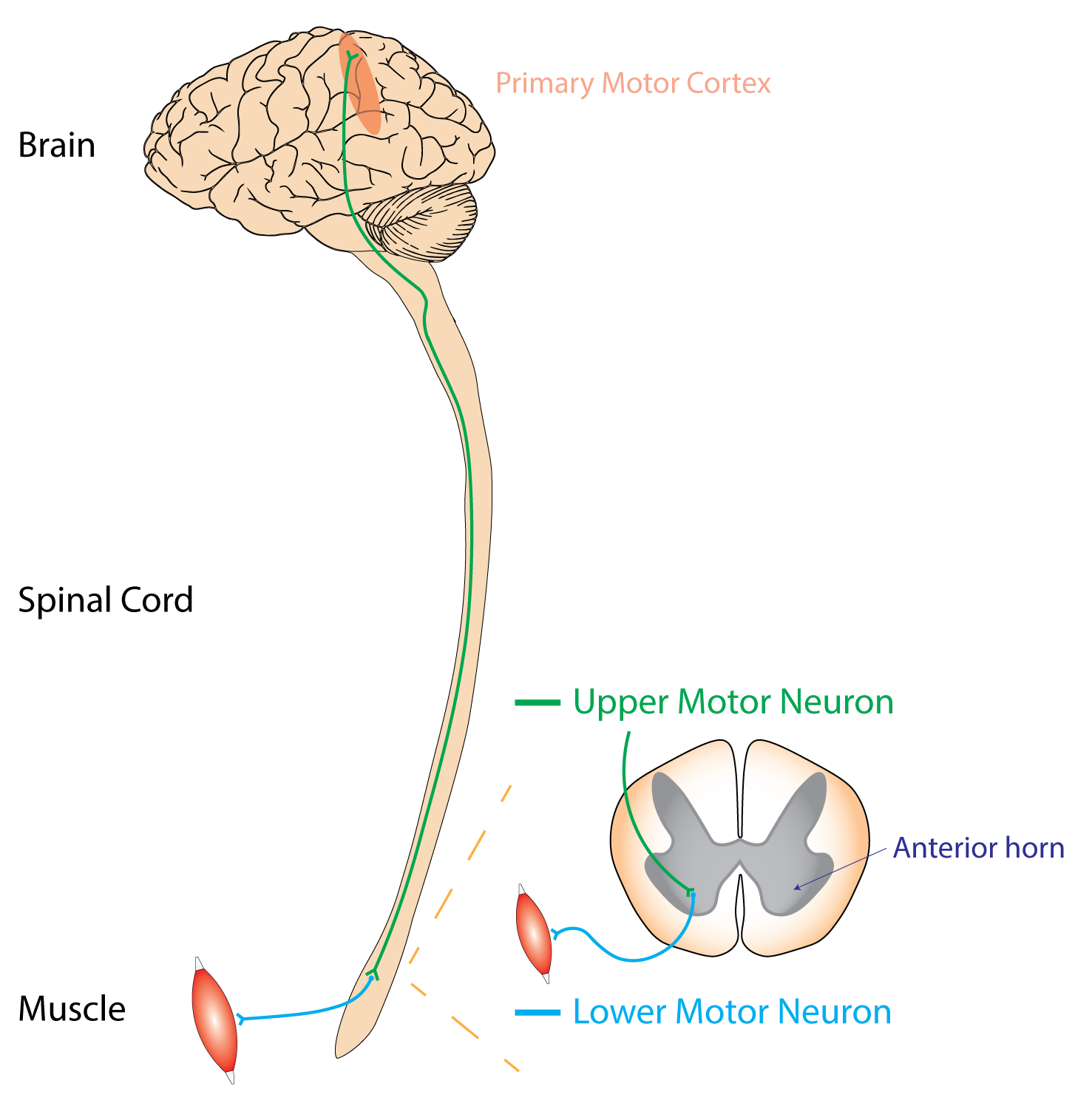
A helpful starting point can be differentiating between an upper (brain or spinal cord) or lower (anterior horn cell, motor nerve roots or peripheral motor nerve) motor neurone lesion.
Upper motor neurone lesions
An upper motor neurone (UMN) lesion will be in the central nervous system (brain and spinal cord).
On neurological examination, typical signs of an upper motor neurone lesion include:
- Disuse atrophy (minimal) or contractures
- Increased tone (spasticity/rigidity) +/- ankle clonus
- Pyramidal pattern of weakness (extensors weaker than flexors in arms, and vice versa in legs)
- Hyperreflexia
- Upgoing plantars (Babinski sign)

Lower motor neurone lesions
A lower motor neurone (LMN) lesion affects anywhere from the anterior horn cell to the muscle.
On neurological examination, typical signs of a lower motor neurone lesion include:
- Marked atrophy
- Fasciculations
- Reduced tone
- Variable patterns of weakness
- Reduced or absent reflexes
- Downgoing plantars or absent response
Upper vs lower motor neurone lesions
Upper motor neurone lesions present with hypertonia and spastic paralysis, whereas lower motor neurone lesions are usually associated with hypotonia and flaccid paralysis.
This is because of the impaired ability of motor neurons to regulate descending signals, giving rise to disordered spinal reflexes.
The central nervous system is involved in suppressing pathway activity. That is, the corticospinal tract helps in the conscious inhibition of muscle. If we damage UMNs, there is a loss of inhibitory tone of muscles leading to constant contraction of muscles.
This leads to the typical hypertonia, spastic paralysis and hyperreflexia seen when examining patients with UMN lesions.
In contrast, if LMNs are damaged or lost, there is nothing to tell the muscles to contract, resulting in hypotonia and flaccid paralysis.
Table 1. A summary of upper motor neurone (UMN) vs lower motor neurone (LMN) lesions.
| Upper motor neurone | Lower motor neurone | |
| Site of the lesion | Cerebral hemispheres, cerebellum, brainstem, spinal cord | Anterior horn cell, motor nerve roots, peripheral motor nerves |
| Inspection | No fasciculations or significant wasting (however there may be some disuse atrophy or contractures) | Wasting and fasciculation of muscles |
| Tone | Increased (spasticity or rigidity) +/- ankle clonus | Decreased (hypotonia, flaccid) or normal |
| Power | Reduced with pyramidal pattern of weakness (extensors weaker than flexors in arms, and vice versa in legs) | Reduced in distribution of affected motor root/nerve |
| Reflexes | Exaggerated or brisk (hyperreflexia) | Reduced or absent (hyporeflexia or areflexia) |
| Plantar reflex | Upgoing/extensor (Babinski positive) | Normal (downgoing/flexor) or no movement |
| Examples of conditions |
|
|
References
- Rcchang16. UMN vs LMN. License: [CC BY-SA]