- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Atrioventricular (AV) block (often referred to as “heart block”) involves the partial or complete interruption of impulse transmission from the atria to the ventricles.
This interruption of impulse transmission results in characteristic ECG findings that differ depending on the subtype of AV block.
The most common cause of AV block is idiopathic fibrosis and sclerosis of the conduction system.
Any patient presenting with AV block requires investigation to identify underlying causes:
- ECG: to help determine the subtype of AV block
- Laboratory investigations (e.g. FBC, U&Es, TSH, troponin): to rule out underlying causes
- Echocardiogram: to rule out structural heart disease
Some forms of AV block can be managed conservatively, whereas other sub-types require intervention.
This article will explore each of the sub-types of AV block including:
- First-degree AV block
- Second-degree AV block (type 1)
- Second-degree AV block (type 2)
- Third-degree (complete) AV block
For more information on ECG interpretation, see the Geeky Medics guide to how to read an ECG.
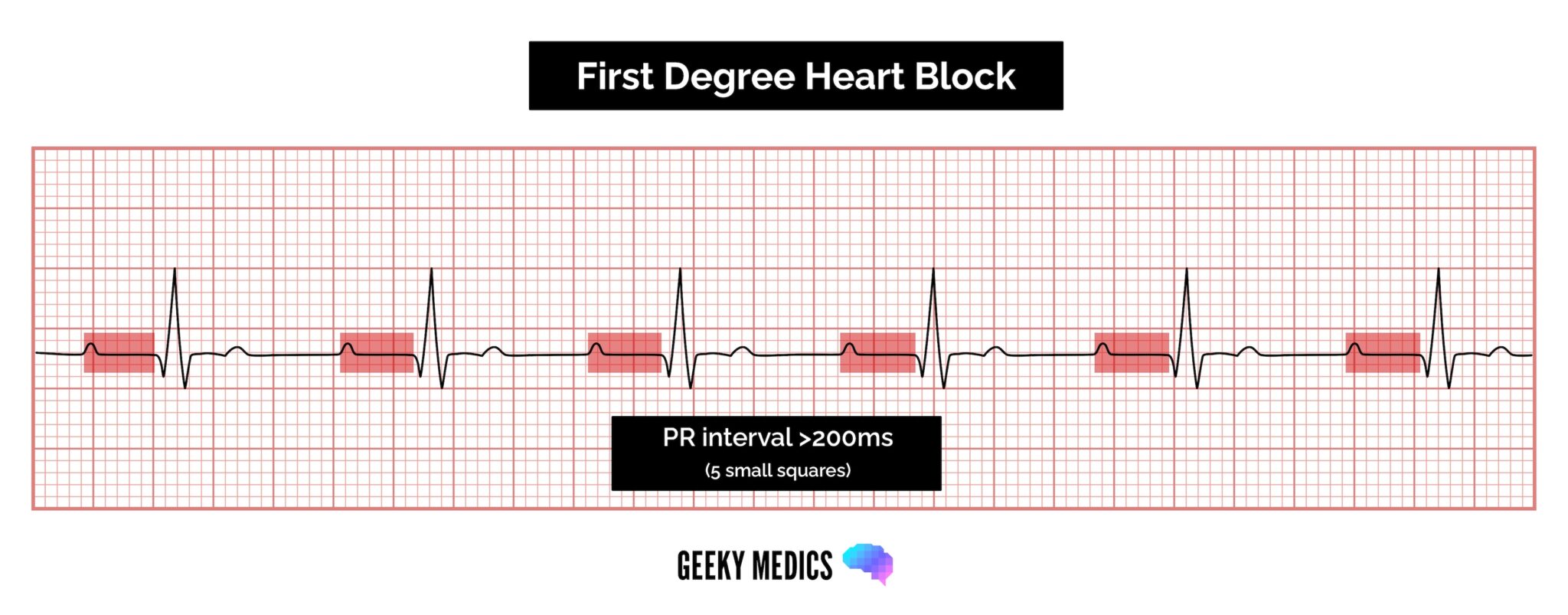
First-degree AV block
First-degree AV block involves the consistent prolongation of the PR interval (defined as >0.20 seconds) due to delayed conduction via the atrioventricular node.
Every P wave is followed by a QRS complex (i.e. there are no dropped QRS complexes, unlike some other forms of AV block discussed later).
First-degree AV block is common and can often be an incidental finding.1
Aetiology
Causes of first-degree AV block include:
- Enhanced vagal tone: often seen in athletes (non-pathological)
- Post myocardial infarction
- Lyme disease
- Systemic lupus erythematosus
- Congenital
- Myocarditis
- Electrolyte derangements
- Drugs: particularly AV blocking drugs such as beta-blockers, rate-limiting calcium-channel blockers, digoxin and magnesium1
- Thyroid dysfunction
ECG findings
ECG findings in first-degree AV block include:
- Rhythm: regular
- P wave: every P wave is present and followed by a QRS complex
- PR interval: prolonged >0.2 seconds (5 small squares)
- QRS complex: normal morphology and duration (<0.12 seconds)
Clinical features
History
Patients are usually asymptomatic.
Clinical examination
Clinical examination is normally unremarkable.
Management
Any AV blocking drugs should be stopped. No intervention is usually required if the patient is asymptomatic.
If the patient is symptomatic, a pacemaker may be considered.
Complications
First-degree AV block does not usually progress to higher grade AV blocks. Those with first-degree AV block may be at an increased risk of atrial fibrillation.1
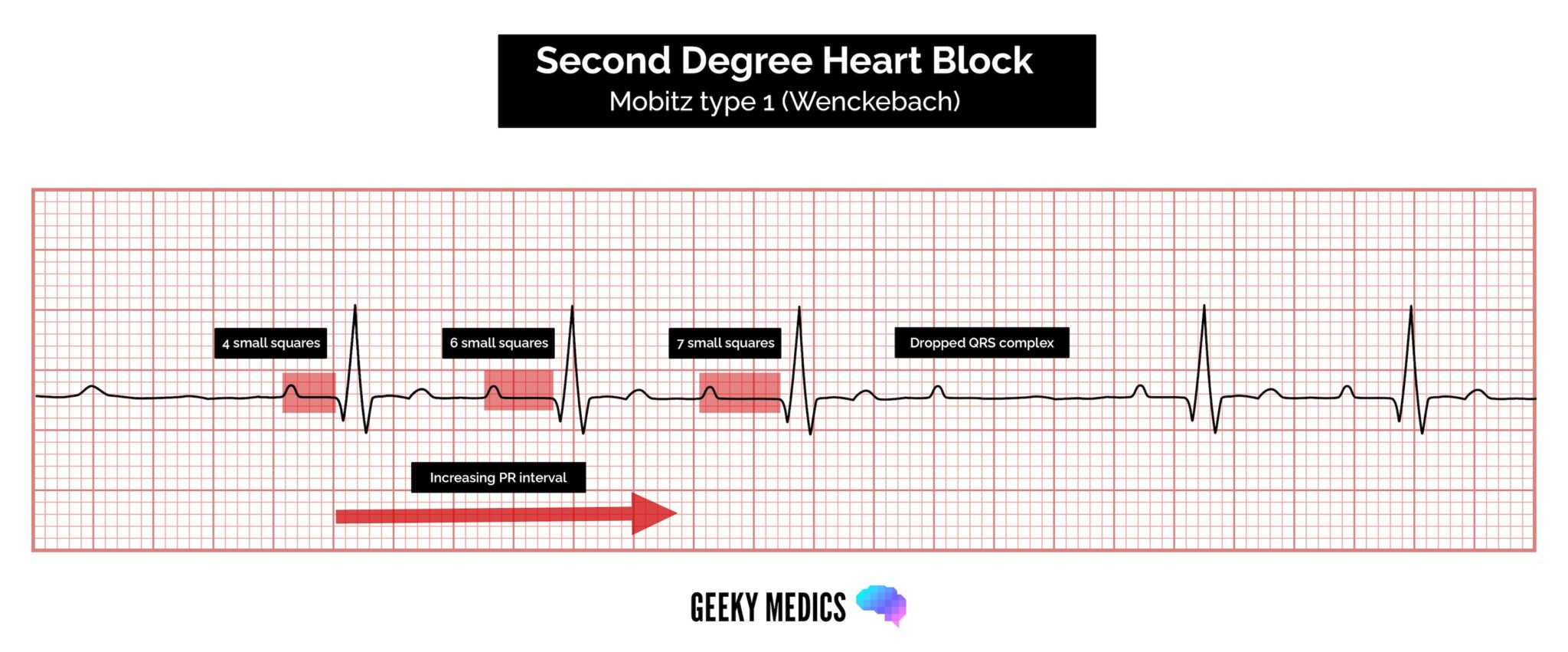
Second-degree AV block (type 1)
Second-degree AV block (type 1) is also known as Mobitz type 1 AV block or Wenckebach phenomenon.
Typical ECG findings in Mobitz type 1 AV block include progressive prolongation of the PR interval until eventually the atrial impulse is not conducted and the QRS complex is dropped.
AV nodal conduction resumes with the next beat and the sequence of progressive PR interval prolongation and the eventual dropping of a QRS complex repeats itself.
Aetiology
Causes of second-degree AV block (type 1) include:2
- Increased vagal tone: often seen in athletes (non-pathological)
- Drugs: beta-blockers, calcium channel blockers, digoxin, amiodarone
- Inferior myocardial infarction
- Myocarditis
- Cardiac surgery (mitral valve repair, Tetralogy of Fallot repair)
ECG findings
ECG findings in second-degree AV block (type 1) include:
- Rhythm: irregular
- P wave: every P wave is present, but not all are followed by a QRS complex
- PR interval: progressively lengthens before a QRS complex is dropped
- QRS complex: normal morphology and duration (<0.12 seconds), but are occasionally dropped
Clinical features
History
Patients are usually asymptomatic, but some can develop symptomatic bradycardia and present with symptoms such as pre-syncope and syncope.
Clinical examination
Typical clinical findings may include:
- Irregular pulse
- Bradycardia
Management
AV blocking drugs should be stopped. Second-degree AV block (type 1) is usually benign and rarely causes haemodynamic compromise.2
Usually, no intervention is required if the patient is asymptomatic. If the patient is symptomatic a pacemaker may be considered.
Complications
The patient may become haemodynamically compromised, although this is rare.2
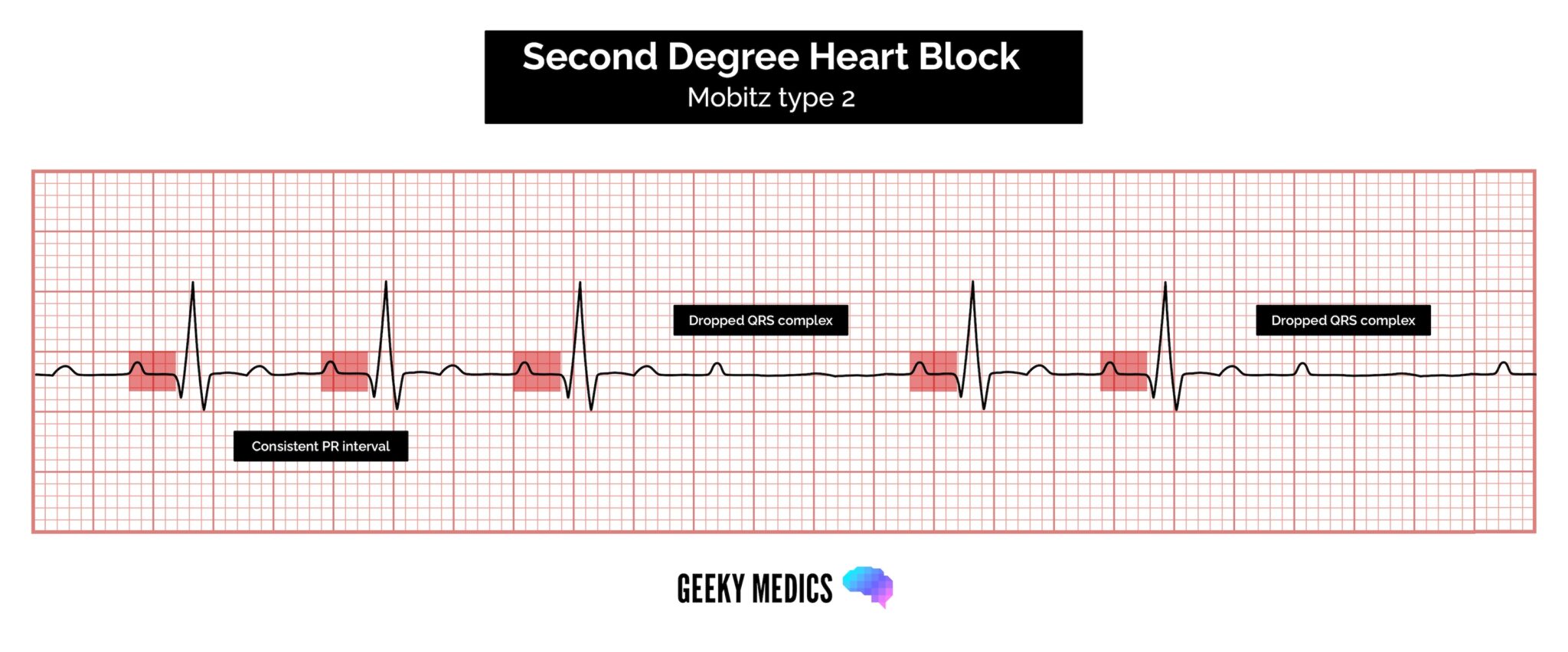
Second-degree AV block (type 2)
Second-degree AV block (type 2) is also known as Mobitz type 2 AV block.
Typical ECG findings in Mobitz type 2 AV block include a consistent PR interval duration with intermittently dropped QRS complexes due to a failure of conduction.
The intermittent dropping of the QRS complexes typically follows a repeating cycle of every 3rd (3:1 block) or 4th (4:1 block) P wave.
Aetiology
Mobitz type 2 AV block is always pathological, with the block typically occurring at either the bundle of His (20%) or the bundle branches (80%).
Causes of second-degree AV block (type 2) include:3
- Myocardial infarction
- Idiopathic fibrosis of the conducting system (Lenegre’s or Lev’s disease)
- Cardiac surgery (especially surgery occurring close to the septum such as mitral valve repair)
- Inflammatory conditions (rheumatic fever, myocarditis, Lyme disease)
- Autoimmune (SLE, systemic sclerosis)
- Infiltrative myocardial disease (amyloidosis, haemochromatosis, sarcoidosis)
- Hyperkalaemia
- Drugs (e.g. beta-blockers, calcium channel blockers, digoxin, amiodarone)
- Thyroid dysfunction
ECG findings
ECG findings in second-degree AV (type 2) include:
- Rhythm: irregular (may be regularly irregular in 3:1 or 4:1 block)
- P wave: present but there are more P waves than QRS complexes
- PR interval: consistent normal PR interval duration with intermittently dropped QRS complexes
- QRS complex: normal (<0.12 seconds) or broad (>0.12 seconds)
- The QRS complex will be broad if the conduction failure is located distal to the bundle of His 3
Clinical features
History
Symptoms may include:
- Palpitations
- Pre-syncope
- Syncope
Clinical examination
Clinical examination may detect a ‘regularly irregular’ pulse, where there is a pattern of how many atrial depolarisations (P waves) lead to ventricular depolarisation (QRS waves) such as 3:1 block.1
Management
Because of the risk of progression to complete AV block, patients should be placed on a cardiac monitor as soon as possible.
The underlying cause of the AV block should be investigated.
Temporary pacing or isoprenaline may be required if the patient is haemodynamically compromised due to bradycardia.
A permanent pacemaker is usually inserted if there are no reversible causes identified.
Complications
Patients are at risk of progressing to symptomatic complete AV block, in which the escape rhythm is likely to be ventricular and thus too slow to maintain adequate systemic perfusion.
Patients are also at risk of developing asystole.3
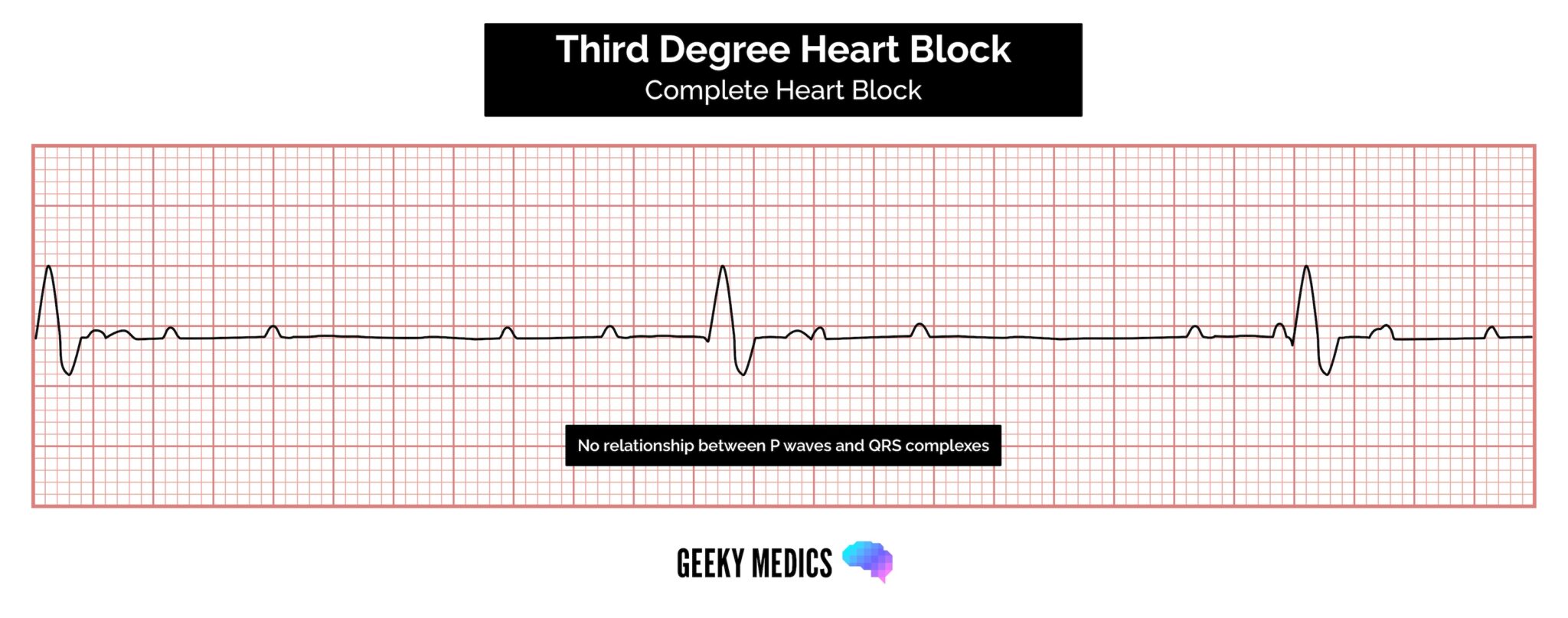
Third-degree (complete) AV block
Third-degree (complete) AV block occurs when there is no electrical communication between the atria and ventricles due to a complete failure of conduction.4
Typical ECG findings include the presence of P waves and QRS complexes that have no association with each other, due to the atria and ventricles functioning independently.
Cardiac function is maintained by a junctional or ventricular pacemaker.4
Narrow-complex escape rhythms (QRS complexes of <0.12 seconds duration) originate above the bifurcation of the bundle of His. A typical heart rate would be >40bpm.
Broad-complex escape rhythms (QRS complexes >0.12 seconds duration) originate from below the bifurcation of the bundle of His. These escape rhythms produce slower, less reliable heart rates and more significant clinical features (e.g. heart failure, syncope).
Aetiology
Causes of third-degree (complete) AV block include:4
- Congenital: structural heart disease (e.g transposition of the great vessels), autoimmune (e.g maternal SLE)
- Idiopathic fibrosis: Lev’s disease (fibrosis of the distal His-Purkinje system in the elderly) and Lenegre’s disease (fibrosis of the proximal His-Purkinje system in younger individuals)
- Ischaemic heart disease: myocardial infarction, ischaemic cardiomyopathy
- Non-ischaemic heart disease: calcific aortic stenosis, idiopathic dilated cardiomyopathy, infiltrative disease (e.g. sarcoidosis, amyloidosis)
- Iatrogenic: post-ablative therapies and pacemaker implantation, post-cardiac surgery
- Drug-related: digoxin, beta-blockers, calcium channel blockers, amiodarone
- Infections: endocarditis, Lyme disease, Chagas disease
- Autoimmune conditions: SLE, rheumatoid arthritis
- Thyroid dysfunction
ECG findings
ECG findings in third-degree (complete) heart block include:
- Rhythm: variable
- P wave: present but not associated with QRS complexes
- PR interval: absent (as there is atrioventricular dissociation)
- QRS complex: narrow (<0.12 seconds) or broad (>0.12 seconds) depending on the site of the escape rhythm (see introduction)
Clinical features
History
Typical symptoms of third-degree heart block may include:
- Palpitations
- Pre-syncope/syncope
- Confusion
- Shortness of breath (due to heart failure)
- Chest pain
- Sudden cardiac death
Clinical examination
Typical clinical findings in third-degree heart block may include:
- Irregular pulse
- Profound bradycardia
- Haemodynamic compromise (e.g. prolonged capillary refill time and hypotension)
Management
Patients should be placed on a cardiac monitor.
Transcutaneous pacing/temporary pacing wire or isoprenaline infusion may be required. Some rhythms (particularly narrow-complex escape rhythms) may respond to atropine.
A permanent pacemaker is usually required.
Complications
The main complication is sudden cardiac death due to ventricular arrhythmias.4
Reviewer
Professor Faizel Osman
Cardiology Consultant
UHCW NHS Trust
Editor
Dr Chris Jefferies
References
- Patient.info. ECG Identification of Conduction Disorders. Published in 2016. Available from: [LINK].
- Life In The Fast Lane. AV Block: 2nd degree, Mobitz I (Wenckebach Phenomenon). Published in 2019. Available from: [LINK].
- Life In The Fast Lane. AV Block: 2nd degree, Mobitz II (Hay block). Published in 2019. Available from: [LINK].
- Parveen Kumar and Michael Clarke. Kumar & Clark’s Clinical Medicine. Published in 2017.
- Adapted by Geeky Medics. James Heilman, MD. Delta wave. Licence: [CC BY-SA]