- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Condom counselling often features in OSCEs, so it’s important to be familiar with the various methods of contraception available and forms of sexual health promotion.
This article focuses on counselling patients about the external condom (also called the male condom), including the common questions patients ask, the information you’ll be expected to give and how best to structure the consultation.
Opening the consultation
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient, including your name and role.
Confirm the patient’s name and date of birth.
Explain the reason for the consultation: “I understand you are interested in learning about using condoms for contraception. Is that correct?”.
It is important to establish a good rapport and an open line of communication with the patient early in the consultation: “If you have any questions at any point, or if something is not clear, please feel free to interrupt and ask me.”
Make sure to check the patient’s understanding at regular intervals throughout the consultation and provide opportunities to ask questions (this is often referred to as ‘chunking and checking’).
Ideas, concerns and expectations
A key component of a counselling station involves exploring a patient’s ideas, concerns and expectations (often referred to as ICE).
In a contraceptive consultation, it is important to explore ICE, as many patients will have researched or have prior experience with contraceptive methods. This will help you tailor the consultation and the advice you give regarding specific methods. It is important to identify any patient concerns and expectations early in the consultation, as this may affect the tolerability of the method and subsequent contraceptive efficacy.
It can sometimes be challenging to use the ICE structure in a way that sounds natural in your contraceptive consultation, but we have provided some examples for each of the three areas below.
Ideas
Explore what the patient currently understands about condoms:
- “What do you already know about using condoms?”
Concerns
Ask if the patient has any concerns about using condoms:
- “Is there anything that worries you about using condoms?”
Expectations
Explore the patient’s expectations of using condoms and the consultation:
- “What factors have made you consider using condoms?”
- “Is there anything you want me to focus on today?”
What is a condom?
Using patient-friendly language, explain that condoms are rubbery sheaths that are worn over the penis to protect against pregnancy and/or sexually transmitted infections. Condoms are designed to be used for all penetrative sexual activity including oral, vaginal and anal sex.
As a contraceptive method, condoms provide a physical barrier which prevents semen from entering the vagina during sexual activity. As the sperm cannot pass through the latex or alternative material, this prevents the sperm from fertilising an egg. Condoms are also used to reduce the risk of transmission of sexually transmitted infections, as the barrier reduces skin and genital contact between sexual partners.
Condoms come in various sizes, colours, textures and flavours to provide options for the user based on intended use and preference. While they’re usually made of latex, other materials such as polyurethane are available for those with allergies or different preferences.
Explain to the patient that while there are a wide variety of contraceptives available, barrier methods, including condoms, are the only methods that prevent both pregnancy and sexually transmitted infections.
Example
“Condoms are stretchy, rubbery sheaths that can be worn over a penis, a bit like a sock. They act as a physical barrier to stop sperm from entering the vagina, which helps to prevent pregnancy. They also provide a barrier between you and your partner’s genital skin, helping to stop the spread of sexually transmitted infections.”
“Condoms come in all sorts of sizes, colours, textures, and even flavours. This means you can choose one that you like and feel comfortable using. Some people have allergies to latex, which is a common material used in condoms so there are non-latex options available as well.”
How effective are condoms?
When counselling patients regarding contraception, it is very important to explain how effective any method is and highlight any factors which may impact efficacy.
Preventing pregnancy
Explain to the patient that with perfect use, external condoms are 98% effective at preventing pregnancy. However, with typical (‘real world’) use, they are around 82% effective.
Example
“When used perfectly, condoms are 98% effective at preventing pregnancy. This means that in a year, only around 2 out of 100 people who use condoms perfectly will get pregnant.”
“However, with typical use, we find condoms are around 82% effective. This means 18 out of 100 people who use condoms perfectly will get pregnant.”
Preventing sexually transmitted infections
Explain to the patient that condoms are highly effective at preventing sexually transmitted infections, especially those transmitted via genital fluid (e.g. HIV, chlamydia, gonorrhoea).
However, they can be less effective at preventing STIs transmitted mainly by skin-to-skin contact (e.g. scabies) as areas of skin not covered by a condom may still transmit the infection.
Example
“Condoms, are very effective at preventing sexually transmitted infections as they provide a physical barrier. However, they might not prevent you from some infections which are passed on by skin to skin contact, such as scabies”
Advantages and disadvantages of condoms
When discussing contraceptive options, it is important to give the patient enough information to make an informed decision and direct them to reputable sources of further information.
When explaining potential advantages and disadvantages, you should consider the patient’s ideas, concerns and expectations (identified earlier in the consultation).
Signposting is important to help you structure the consultation: “Next, I’d like to talk about some of the additional benefits of using condoms and some of the potential disadvantages. Is that ok?.”
Advantages of condoms
Advantages of condoms include:
- Prevent both pregnancy and sexually transmitted infections
- Easily accessible and can often be collected for free from sexual health clinics
- Only need to be used at the time of intercourse
- Non-hormonal method of contraception
- No long-term side effects
- Accessible to any gender for purchase/collection
- No pre-planning is needed, meaning they are suitable for unplanned sex
Example
“As we’ve discussed, condoms can prevent sexually transmitted infections and pregnancy. This is unlike other forms of contraception, such as the pill or implant, which only prevent pregnancy. Other advantages are that condoms are easily accessible to anyone, non-invasive, and have no side effects.”
Disadvantages of condoms
Potential disadvantages of condoms include:
- Some people feel putting on condoms interrupts the flow of sex; however, this can be prevented by making putting on a condom part of foreplay
- Some people feel condoms are uncomfortable
- External condoms can only be placed on a penis; internal condoms (also known as female condoms) are available but are less effective
- Greater failure rate than in some other forms of contraception
- May break or leak, especially with incorrect use
- Not suitable for those with latex allergy (however, there are alternative materials available)
Example
“There are some disadvantages of condoms, they are less effective at preventing pregnancy than some other forms of contraception such as the implant and the IUD. They also need to be used correctly to be effective, and we’re going to cover how to use a condom shortly. There is a risk of the condom breaking or leaking, especially if they are not used correctly. Some people can find using condoms uncomfortable or feel it interrupts sex.”
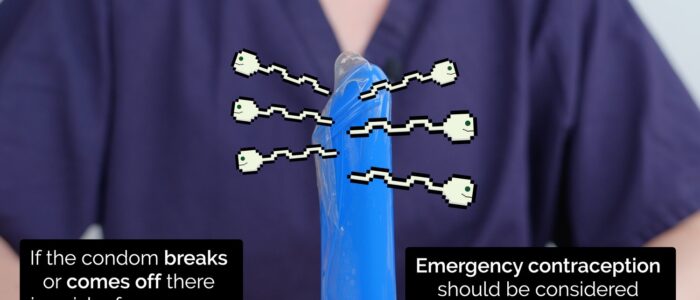
Demonstrate how to use a condom
Ensure you clearly explain and demonstrate each of the following steps to the patient using condoms and a training model of an erect penis.
Applying a condom
1. Inspect the condom packaging:
- There should be no breaks, tears or evidence of tampering
- Check the expiry date to ensure the condom is in date
- Check for a BSI kite mark and European CE mark
2. Tear open the packet and remove the condom:
- Condoms can tear easily- do not use teeth, and be careful with nails and jewellery
3. Check you are holding the condom the right way up:
- You need to be able to roll the condom downwards- if you have tried to to apply the condom upside down, discard and use a new condom.
4. Pinch the tip of the condom to expel any air
5. Pull back the foreskin if the penis is uncircumcised
6. Place the condom on the tip of the erect penis and roll it down the shaft using your other hand until it is fully unrolled. The fit should be snug.
Tip
Condoms should only be applied to an erect penis.
Whilst water or silicon-based lubricants are safe to be used with a condom, oil-based lubricants are NOT. Oil based lubricants can degrade latex and damage a condom’s integrity.
Removing a condom
1. When withdrawing the penis, secure the condom at the base of the penis to ensure the condom does not slide off
2. It is good practice to check the condom after intercourse for any breakages. If a break or tear is noted after sex, advice should be sought regarding whether any treatment is required or advised to prevent pregnancy or STI transmission.
3. Remove the condom from the penis, taking care not to spill any semen or allow the penis to touch the other person’s genitals
4. Discard the condom in a bin (condoms should not be put down the toilet as they can cause a blockage)
Tip
Once removed, condoms should never be reused, and a new condom should be used for each sexual encounter.
Assess the patient’s condom technique
Observe the patient’s technique using the condom training model.
Provide feedback to allow the patient to refine their technique.
Continue to repeat the cycle of observation and feedback until the patient can use a condom effectively.
Closing the consultation
Close the consultation by summarising what you have discussed. This allows you to emphasise the key points of the consultation to ensure patient understanding.
Ask the patient if they have any further questions or concerns that haven’t been addressed.
If relevant, offer an STI screen, and/or further information about other contraceptive methods.
Finally, thank the patient for their time and offer them a leaflet summarising the key information related to using condoms and how to access condoms locally (e.g. Sexwise condom leaflet).
Dispose of PPE appropriately and wash your hands.
Reviewer
Dr Grace Farrington
References
- British Association for Sexual Health and HIV (BASHH). Condoms. Available from: [LINK]
- Contraception Choices. Condoms. Available from: [LINK]
- Faculty of Sexual and Reproductive Healthcare (FSRH). FSRH Clinical Guideline: Barrier Methods for Contraception and STI Prevention. Published in 2015. Available from: [LINK]