- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Endometriosis is a condition where endometrium-like tissue grows outside of the uterine cavity. It is the second most common gynaecological condition after uterine fibroids.
Endometriosis affects approximately 10% of women of reproductive age in the UK and takes an average of 7.5 years from first symptoms to diagnosis.1
Aetiology
Endometriosis has no single definitive cause. Multiple theories have been put forward, but it is likely multifactorial, including genetic factors and retrograde menstruation (blood flows backwards into the pelvis instead of out of the vagina during menstruation).
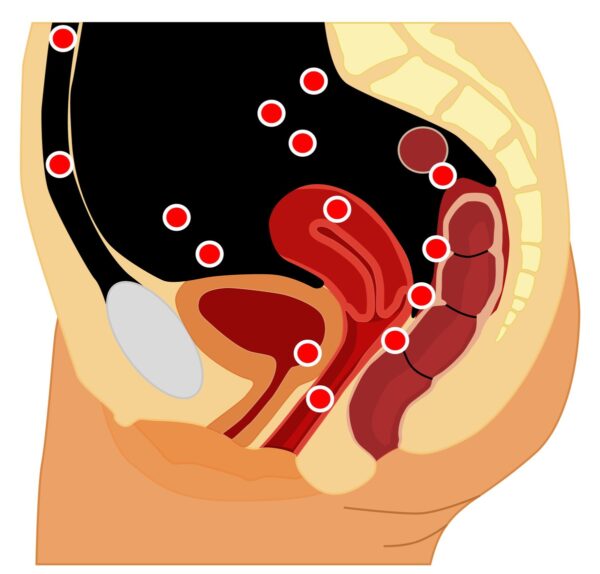
The most common location for endometriosis is the pelvis, ovaries, peritoneum, uterosacral ligaments, and the pouch of Douglas (Figure 1).
Risk factors
Risk factors for endometriosis include:3
- Early menarche
- Late menopause
- Delayed childbearing
- Nulliparity
- Family history
- Vaginal outflow obstruction
- White ethnicity
- Low body mass index
- Autoimmune disease
- Smoking
Clinical features
History
Clinical presentation is variable, with some women experiencing several severe symptoms and others having no symptoms at all.
Typical symptoms of endometriosis may include:
- Chronic pelvic pain: pelvic pain lasting for 6 months or longer
- Dysmenorrhoea: pain often starts days before bleeding
- Deep dyspareunia
- Non-gynaecological: dysuria, urgency, haematuria and dyschezia (painful bowel movements)
- Subfertility
Other important areas to cover in history include:
- Risk factors for endometriosis
- Menstrual history (e.g. date of last menstrual period)
- Medication history (e.g. contraceptives, anticoagulants)
- Fertility plans: important when considering management options
Clinical examination
Typical findings on abdominal examination may include:
- Abdominal tenderness
Typical findings on pelvic/bimanual examination may include:
- Reduced organ mobility
- Tender nodularity in the posterior vaginal fornix
- Visible vaginal endometriotic lesions may be seen
A normal pelvic or abdominal examination does not exclude endometriosis.
Differential diagnoses
Differential diagnoses to consider in the context of endometriosis include:
- Pelvic inflammatory disease
- Ectopic pregnancy
- Torsion of an ovarian cyst
- Appendicitis
- Irritable bowel syndrome
- Primary dysmenorrhoea
- Uterine fibroids
Investigations
Bedside investigations
Relevant bedside investigations include:
- Urine pregnancy test (hCG urine dipstick): performed on all women of reproductive age to rule pregnancy in or out.
Laboratory investigations
Relevant laboratory investigations include:
- Baseline blood tests (FBC, U&Es, CRP): white cells may be raised in appendicitis or pelvic inflammatory disease.
Imaging
Consider a transvaginal ultrasound scan which can be helpful to show endometriomas, however, a normal scan does not exclude endometriosis.
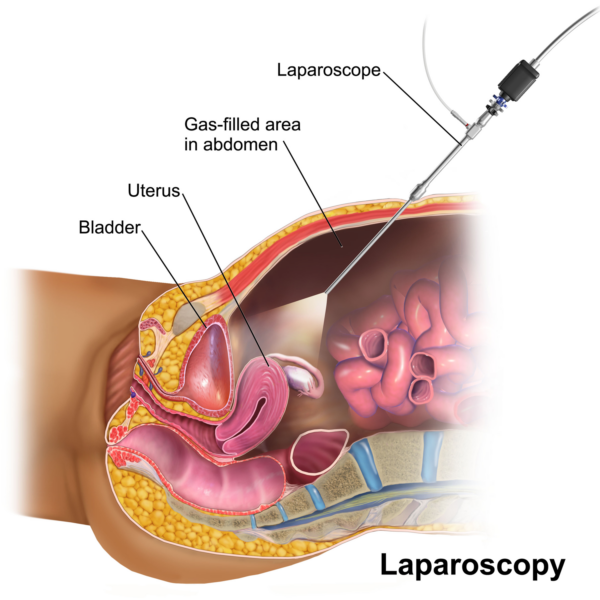
Diagnostic laparoscopy
Diagnostic laparoscopy is the gold standard investigation (Figure 2). However, this is still an invasive procedure with a small risk of major complications (e.g. bowel perforation).
Pelvic MRI (magnetic resonance imaging) and serum CA-125 (cancer antigen) are not routinely recommended investigations. MRI may be requested by specialist teams to look for deep endometriosis.
Management
Endometriosis can be a chronic disease affecting women throughout their reproductive lives. Some patients may have complex needs and require long term support.
Therefore, it is important to assess each individual circumstances, symptoms, priorities, desires for fertility, background and the patient’s physical, psychosexual and emotional needs.
If fertility is a priority, management of endometriosis-related subfertility should have multidisciplinary team involvement with input from a fertility specialist.
Initial management
Initial management of endometriosis may include:
- A short trial of paracetamol or non-steroidal anti-inflammatory alone or in combination
- Hormonal treatment (combined contraceptive pill or progesterone)
Referral to gynaecology service should be considered if:
- Initial management is not effective, not tolerated or contraindicated
- There are severe, persistent or recurrent symptoms
- There are pelvic signs of endometriosis
Surgical management
Surgical management options depend on the impact on fertility.
If fertility is not a priority:
- Laparoscopic treatment of peritoneal endometriosis. Hormonal treatment can be used as an adjunct for deep endometriosis (involving bowel, bladder or ureter).
- Hysterectomy performed laparoscopically (with or without oophorectomy) in combination with surgical management. Indications for this include adenomyosis or heavy menstrual bleeding resistant to other treatments.
If fertility is a priority:
- Excision or ablation of endometriosis, adhesiolysis and removal of endometriomas can be offered because this may improve chances of spontaneous pregnancy.
Psychological support
Endometriosis can have a significant impact on women’s quality of life and daily living with repercussions for their relationships, sexuality, work productivity, fitness and mental health. It is important to holistically support women with endometriosis.
Resources are available like Endometriosis UK who help women take back control by providing vital support services, reliable information and a community for those affected.5
Complications
Complications of endometriosis may include:
- Infertility is commonly associated with endometriosis, but the mechanism is not well understood.
- Endometriomas (ovarian cysts containing blood and endometriosis-like tissue) which may rupture or affect fertility
- Adhesions: secondary to endometriosis or surgery
- Bladder obstruction secondary to the adhesions
- Haematuria / rectal bleeding
Key points
- Endometriosis involves the growth of endometrium-like tissue anywhere outside of the uterine cavity.
- The most common location for endometriosis is distributed in the pelvis; on the ovaries, peritoneum, uterosacral ligaments and pouch of Douglas.
- The most common symptoms include chronic pelvic pain, dysmenorrhea, dyspareunia and infertility.
- Possible clinical findings include reduced organ mobility, tender nodularity in the posterior vaginal fornix and visible vaginal endometriotic lesions may be seen.
- Diagnostic laparoscopy is the definitive diagnostic investigation.
- Medical management involves paracetamol, NSAIDs and hormonal treatment (combined contraceptive pill or progesterone).
- Surgical management options include laparoscopic treatment, hormonal adjunct and hysterectomy (according to women’s symptoms, preferences and priorities).
- Complications of endometriosis can include infertility, endometriomas, adhesions, chronic pelvic pain and reduced quality of life.
Reviewer
Dr Rachel Greenwood
Obstetrics & Gynaecology Registrar
Editor
Dr Chris Jefferies
References
- Endometriosis UK. It takes an average 7.5 years to get a diagnosis of endometriosis – it shouldn’t. Available from: [LINK]
- Tsaitgaist derivative work: Hic et nunc. Female anatomy. Licence: [CC-BY-SA]
- NICE CKS. Endometriosis. Available from: [LINK]
- Blausen.com staff / Medical gallery of Blausen Medical 2014. Laparoscopy. Licence: [CC BY-SA]
- Endometriosis UK. Home page. Available from: [LINK]