- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
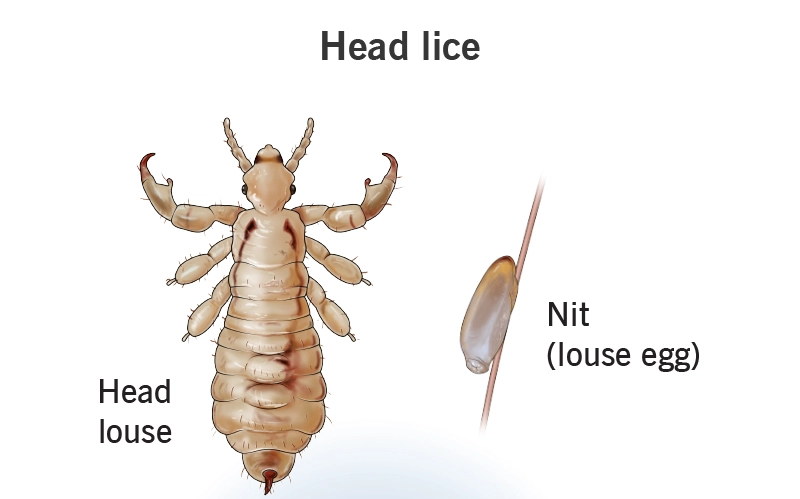
Head lice are a common parasite infestation known as pediculosis capitis. The head louse (Pediculus humanis capitis) infests the hairs on the scalp and feeds on human blood.
Anyone can catch head lice, but typically, it affects primary school-age children and their families.
Aetiology
Head lice are most commonly spread by direct head-to-head contact, allowing the lice to crawl from one host to another. Head lice cannot fly or jump; they are restricted to the scalp or hair of the infected person.
A louse can only survive 1-2 days away from a human host.
Head lice life cycle
Adult lice are 2-3mm in length, with six legs to cling to hair shafts. They inject the scalp with saliva and feed on human blood, which causes itching and irritation. The females lay up to 10 eggs daily, and adult lice live up to 30 days.
Louse eggs (ova or nits) are oval and brown but become yellowish-white once hatched. They can be easier to spot than adults. Eggs are laid close to the scalp and attached to hair shafts, taking just over a week to hatch.
Nymphs (baby lice) take 7-10 days to mature. After maturing, they mate, and the females lay eggs, restarting the cycle. Untreated, the cycle repeats every three weeks.
Risk factors
Risk factors for head lice include:
- Age 4-11 years
- Female sex
- Sharing beds, clothing, and hairbrushes
- A greater number of children in the family
- Overcrowded living conditions
Clinical features
History
Typical symptoms of head lice include:
- Scalp pruritus (itching)
- The feeling of things moving in the hair
- Scratching, causing crusting and scale
Clinical examination
On visual inspection of the scalp, there may be visible live nymphs or adult lice and eggs visible on the hair shaft within 1cm of the scalp (Figure 4).

There may be small red papules under the hairline at the nape of the neck and behind the ears. These are louse bites. Severe cases can also cause cervical lymphadenopathy.
Differential diagnoses
Head lice can appear similar to the following dermatological conditions:
- Seborrheic dermatitis
- Tinea capitis
- Folliculitis
Investigations
Head lice are a clinical diagnosis on discovering a live nymph or adult louse. This can be done by combing the hair with a fine-tooth comb.
Management
Managing head lice involves treatment to eliminate the lice and their eggs and preventative measures to avoid re-infestation.
Most cases of headlice do not need medical input and can be treated with over-the-counter topical insecticides in combination with a wet combing regimen.
Headlice should be treated as soon as they are spotted. Close contacts (including daycare/school) should be informed. Other household members should be checked for headlice and, if infected, treated simultaneously to prevent re-infestation.
Topical therapy
A physical insecticide is recommended, such as dimeticone. This kills the louse by coating it with a physical barrier, causing suffocation. This means resistance is unlikely to develop.
Other treatments include insecticides like malathion, pyrethrin, permethrin or ivermectin. Although these are still recommended treatments in the UK, there is widespread resistance to these insecticides, and they are highly flammable.
There should be at least two applications of insecticide. The second application should be 7-10 days after the first, as eggs may survive, allowing new nymphs to hatch.
When other treatments have failed, consider ivermectin either orally or topically.
Wet combing
Wet combing is the systematic combing of wet hair with a fine-tooth comb. This is the most effective way to physically remove head lice. This can be used as an adjunct with topical therapy or first-line in patients wishing to avoid insecticides.
It is recommended to repeat wet combing in four sessions spaced over two weeks to catch any newly hatched head lice. This should be repeated until no lice are found on consecutive occasions.
Wet combing or dimeticone should be used in pregnant or lactating women.
Complications
Head lice is not usually associated with severe complications. However, along with discomfort, it can cause:
- Secondary bacterial infection (impetigo)
- Dermatitis: red scaly, itchy plaques
- Anxiety and distress
- Lymphadenopathy
Key points
- Head lice is a common condition in the community characterised by live lice, pruritis, scratching and louse bites.
- Risk factors include age 4-11, female, overcrowded living conditions and sharing beds, clothing and hair brushes.
- Treatment is with a combination of a topical physical insecticide (e.g. dimeticone) and wet combing.
- It is important to repeat the treatments to prevent new lice from hatching and re-infestation.
- Complications are rare but secondary bacterial infection and dermatitis can occur.
Reviewer
Dr Katie Birks
General Practitioner
Editor
Dr Chris Jefferies
References
- BMJ Best Practice. Pediculosis capitis. Last updated Dec 2022. Available from: [LINK]
- Public Health England. Head lice (pediculosis). Last updated Jan 2018. Available from: [LINK]
- Dermnet. Head lice. Last updated 2017. Available from: [LINK]
- NHS.uk. Head lice and nits. Last updated March 2021. Available from: [LINK]
Image references
- Figure 1. Cleveland Clinic. Head lice. License: [CC BY-SA]
- Figure 2. Gilles San Martin. Female human head louse. License: [CC BY-SA]
- Figure 3. Gilles San Martin. Human head louse egg. License: [CC BY-SA]
- Figure 4. KostaMumcuoglu. Louse nits. License: [CC BY-SA]