- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Constipation is a term used to describe the subjective complaint of the passage of abnormally delayed or infrequent dry, hardened faeces often accompanied by straining and/or pain.1
Constipation is a common problem in childhood and symptoms of constipation can be a source of considerable distress to patients and families.1
Aetiology
‘Normal’ bowel frequency varies widely from child to child and can be especially variable between breast- and bottle-fed babies.
In most cases, paediatric constipation is thought to be multifactorial and can be precipitated by factors such as changes in routine or diet, illness, toilet training, emotional upset or intentionally delayed defaecation (withholding).
Constipation frequently presents at three common stages in childhood:2
- Weaning in infants
- Toilet training in toddlers
- Starting school
In most cases, no functional or anatomical cause is identified, so-called idiopathic (functional) constipation. Constipation is defined as chronic when it has lasted for more than 8 weeks.
Organic causes of paediatric constipation
Constipation less commonly may be the presenting feature of a serious underlying disease arising in infants < 1 year of age.3
Constipation is termed organic when there is an identifiable physiological or anatomical cause.
Careful history-taking and physical examination can identify the ‘red flags’ that could suggest an organic cause.
Hirschsprung’s disease
Hirschsprung’s disease is defined as an absence of ganglion cells (aganglionosis) of the distal colon with variable proximal extension, resulting in failure of the internal anal sphincter and distal colonic muscles to relax in response to rectal distension.
Clinical features of Hirschsprung’s disease include:
- Delayed passage of meconium >48 hours after birth (in a term baby)
- Chronic abdominal distention and vomiting since first few weeks of life
- Family history of Hirschsprung’s disease
Spinal cord problems
Spinal cord problems including spinal cord compression and spina bifida can cause constipation. Clinical features may include:
- Leg weakness or abnormal reflexes
- Gluteal muscle asymmetry
- Sacral dimple/tuft of hair
Anorectal malformations
Anorectal malformations include imperforate anus, anal stenosis or mislocated anus. These can occur with or without fistulation. Clinical features may include:
- Lack of an anal opening
- Abnormally sited anus
- Meconium or gas in the urine
Metabolic conditions
Metabolic conditions including hypothyroidism, coeliac disease, cystic fibrosis, hypokalaemia or hypercalcaemia can cause constipation.
Clinical features will vary depending on the underlying condition, but may include:
- Faltering growth
- Sensitivity to cold, fatigue, dry skin, pallor
- Blood/mucus mixed with stool
Risk factors
Risk factors for paediatric constipation include:
- Diet low in fibre
- Low fluid intake
- Intercurrent illness
- Postoperative bed rest or analgesia (e.g. opioids)
- Psychological difficulty with toilet training
Clinical features
History
For more information on history taking, see the Geeky Medics guide to paediatric history taking.
Typical symptoms of constipation include:
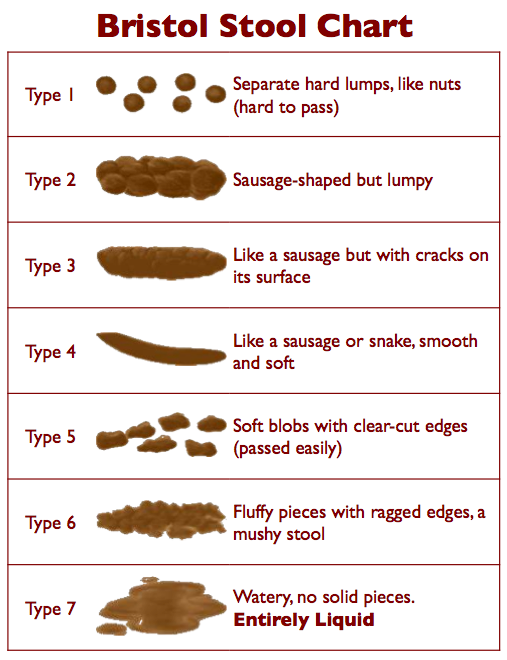
- Infrequent passage of hard stools, typically Bristol stool type one or two (Figure 1)
- Soiling: the involuntary passage of fluid or semi-solid stool into clothing because of overflow from a faecally loaded bowel
- Pain or bleeding when passing stool
- Straining
- Abdominal distention, nausea and/or vomiting
Straining
Signs of straining in children less than one-year-old do not usually suggest constipation provided they pass soft stool and are otherwise healthy. This is because children develop the pelvic muscles to assist bowel movements gradually.2.
Other important areas to cover in the history to cover include:
- Age at onset of symptoms
- Timing of meconium passage
- Dietary history, including fluid intake, type of milk and fibre intake
- Success or failure of toilet training and withholding behaviour
- Past medical/surgical history, current medications and any previous treatment of constipation
Clinical examination
In cases of paediatric constipation, a clinical examination should include:3
- Growth parameters
- Abdominal examination: muscle tone, distension, faecal mass
- Inspection of the perianal region: anal position, stool present around the anus or in underwear, skin tags, excoriations
- Examination of the lumbosacral region: dimples, hair tuft, gluteal cleft deviation, flat buttocks
- Lower limb neuromuscular examination
Digital rectal examination is not routinely necessary, although it may provide some useful information such as the presence of a rectal faecal mass, anatomical abnormalities, anal fissures and sphincter tone (tight in Hirschsprung’s disease or lax in chronic idiopathic constipation).1,4
If the urge to defecate is suppressed for too long (such as in withholding behaviour) stool in the rectum becomes harder and difficult to pass as more water is resorbed.
As stool accumulates, dilatation of the smooth musculature reduces its contractility and desensitisation occurs. Eventually, fluid or semi-solid stool only passes by overflow around a faecal mass involuntarily through a lax anal sphincter (‘stooling’).4,5
Investigations
Investigations are rarely required for the diagnosis of paediatric constipation.3,8
Occasionally, plain X-rays are used to assess the extent of faecal loading but should not be used for diagnosis.3
The presence of red flags suggestive of an organic cause of paediatric constipation should trigger a prompt referral to specialist services for investigation, especially if standard diet and laxative therapy has failed.1
Diagnosis
The most widely accepted criteria for the diagnosis of childhood idiopathic constipation are the Rome criteria.
The Rome IV criteria are divided by the age of the patient:6,7
Management
Non-pharmacological
Non-pharmacological management of paediatric constipation includes:
- Dietary changes: increase fluid and optimise fibre intake, reduction of cow’s milk (excess cow’s milk satisfies baby’s thirst at the expense of water or juice, as well as suppresses appetite for other foods).4
- Behavioural training: encourage regular, unhurried toileting (especially after meals), bowel diaries which link to the use of reward systems.9
- Education: addressing the anxiety of parent and child, explanation of the involuntary nature of soiling which helps to address attitudes of guilt or blame.
Pharmacological
Pharmacological management is divided into disimpaction and maintenance.
Disimpaction
If a clinical assessment suggests faecal impaction of the rectum/colon, then an oral disimpaction regime should be commenced. An escalating dose of oral laxatives are given over a few days to clear the impaction:1
- First line: Movicol (polyethylene glycol 3350 + electrolytes)
- Second line: Lactulose (if Movicol is not tolerated)
Movicol and Lactulose are both osmotic laxatives that work by drawing water into the colon and softening the stool.5
A stimulant laxative (e.g. Senna) is added if disimpaction is not achieved within two weeks.1
An increase in soiling/diarrhoea is common after the initiation of laxatives due to spurious overflow. If this occurs, treatment should not be reduced or stopped.1
Maintenance
Maintenance therapy should be initiated straight away, or after disimpaction is completed, to encourage regular soft bowel motions and should be continued for at least several weeks alongside conservative measures until a healthy bowel habit is established:1,5,10
- First-line: Movicol (polyethylene glycol 3350 + electrolytes): started at half the disimpaction dose
- Second-line: stimulant (e.g. Senna) if tolerance is an issue or therapy isn’t working
Complications
Complications of paediatric constipation include:4
- Faecal impaction: chronic constipation may lead to a mass of stool unable to be evacuated from the rectum. Pain, distention, nausea, vomiting and obstruction may ensue.
- Anal fissure: tears in the rectal mucosa due to the passage of hard stool may cause pain on defaecation and lead to withholding behaviour.
- Rectal prolapse: straining against a hard stool can cause prolapse of the rectum. The prolapse may reduce spontaneously or may need to be reduced manually.
Key points
- Constipation is the passage of infrequent dry, hard stool often accompanied by pain.
- Symptoms become chronic in more than a third of patients and are a common reason for children presenting to primary and secondary care.
- Most cases are idiopathic and can be precipitated by illness, poor diet or significant life events.
- Suspicion of serious underlying pathology (such as Hirschsprung’s disease, cystic fibrosis or spinal cord defects) should trigger a prompt referral to tertiary specialist centres.
- Investigations are rarely necessary as a diagnosis is made from the history and clinical examination.
- Long term management is required with oral laxatives, lifestyle modifications and education to establish a healthy bowel habit.
Reviewer
Professor Ramnath Subramaniam
Consultant Paediatric Urologist
Editor
Dr Chris Jefferies
References
- NICE. Constipation in children and young people: diagnosis and management. 2010 Available from: [LINK]
- NHSGGC Paediatric Clinical Guidelines. Constipation in children. 2019. Available from: [LINK]
- Tabers WW et al. Evaluation and treatment of functional constipation in infants and children: Evidence-based recommendations from ESPGHAN and NASPGHAN. JPGN 2014. Available from: [LINK]
- Jones’ clinical paediatric surgery 6th edition. 2008. Blackwell publishing. ISBN: 978-1-4051-6267-8
- Zeshan Qureshi. The unofficial guide to paediatrics. 1st 2017. ISBN 978-0957 149953
- Hyams JS et al. Functional Disorders: Children and Adolescents. Gastroenterology 2016. Available from: [LINK]
- Benninga MA et al. Childhood functional gastrointestinal disorders: neonate/toddler. Gastroenterology 2016. Available from: [LINK]
- Koppen IJN et al. Childhood constipation: finally something is moving! Expert Review of Gastroenterology and Hepatology 2016 Available from: [LINK]
- Patient.info Constipation in children. 2016. [LINK]
- Afzal et al. Constipation in children. Italian Journal of Pediatrics 2011 Available from: [LINK]




