- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Antepartum haemorrhage (APH) is defined as genital tract bleeding from 24+0 weeks’ gestation and complicates 3-5% of pregnancies.1
The three most important causes of APH are placenta praevia, placental abruption and vasa praevia, these result in high morbidity and mortality for both mother and baby.
Other causes of APH include lower genital tract sources such as cervical polyps, vaginitis and cervicitis.
Placenta praevia
Introduction
Placenta praevia occurs when the placenta lies in the lower uterine segment. It can lead to the complete or partial covering of the internal cervical os.
Placenta praevia increases the likelihood of APH due to poor attachment of the placenta to the uterine wall.
Aetiology
Figure 1 shows the classical grading of placenta praevia.
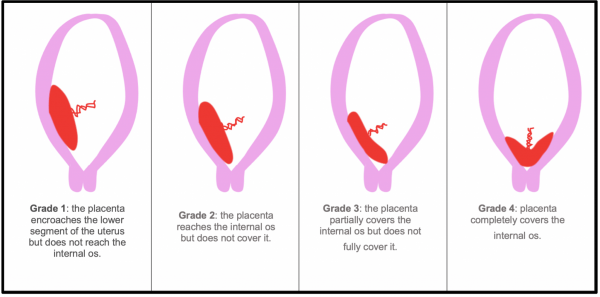
Placenta praevia can also be grouped into two subtypes:
- Minor placenta praevia (grade 1 and 2): the placenta is low but does not cover the internal cervical os
- Major placenta praevia (grade 3 and 4): placenta lies over the internal cervical os
Risk factors
Risk factors for placenta praevia include:2
- Previous caesarean section
- Previous termination of pregnancy
- Multiparity
- Advanced maternal age (over 40)
- Multiple pregnancy
- Smoking
- Deficient endometrium (e.g. due to manual removal of the placenta)
- Assisted conception
Clinical features
History
Typical symptoms of placenta praevia include:1
- Painless vaginal bleeding
- Light contractions may be present
Clinical examination
Typical clinical findings in placenta praevia include:
- Non-tender uterus
- Vaginal bleeding
- Lie and presentation may be abnormal
- Low lying placenta on 20-week anomaly scan
Investigations
Relevant bedside investigations include:
- Vital signs: respiratory rate, BP, oxygen saturations, pulse and temperature
Relevant laboratory investigations include:
- Full blood count, urea and electrolytes and LFTs: helps to exclude hypertensive conditions such as HELLP or pre-eclampsia
- Clotting profile
- Kleihauer test
- Group and save
- Crossmatch
Relevant imaging investigations include:
- Ultrasound scan
Cardiotocography (CTG) is used to monitor the fetus.
Differential diagnoses
Differential diagnoses to consider for placenta praevia include:
- Placental abruption
- Vasa praevia
- Uterine rupture
- Local causes: polyps, carcinoma, cervical ectropion, infection
Management
Placenta praevia is typically identified at the 16-20 week scan. If placenta praevia is identified the mother is rescanned at 32 weeks and if it is still present, again at 36 weeks.2
If placenta praevia is still present at 36 weeks gestation, delivery via caesarean section is recommended, due to the significant risk of spontaneous labour and associated haemorrhage.
Complications
The main complication of placenta praevia is major haemorrhage.
Methods that may be used to stop the bleeding include emergency caesarean section, uterine artery ligation or embolisation, intrauterine balloon tamponade or emergency hysterectomy.
Key points
- Placenta praevia occurs when the placenta lies in the lower uterine segment.
- The placenta may be low lying, partially covering the internal os or completely covering the internal os.
- Placenta praevia presents as painless vaginal bleeding.
- If detected on the 16-20 week scan, patients are rescanned at 32 and 36 weeks. If the placenta is still low lying, a caesarean section is planned to reduce the risk of bleeding during delivery.
Placental abruption
Introduction
Placental abruption is the complete or partial detachment of the placenta before delivery.
Complete abruption accounts for 7% of cases whilst partial abruption is more common, accounting for 93% of cases.
Overall placental abruption accounts for around a quarter of all cases of APH. It is a large cause of perinatal mortality accounting for 10-20% of all perinatal deaths.
Aetiology
The cause of placental abruption is often unknown. It may occur due to trauma or injury to the abdomen.
Risk factors
Risk factors for placental abruption include:2
- Maternal age greater than 35
- Multiparity
- Current pre-eclampsia, HELLP
- History of hypertension
- History of previous abruptions
- History of anti-phospholipid syndrome
- History of thrombophilia
- Smoking during pregnancy
- Use of cocaine during pregnancy
- Trauma
Clinical features
History
Typical symptoms of placental abruption include:1
- Abdominal pain (most common) – posterior placental abruptions may present with back pain
- Vaginal bleeding
- Uterine contractions
- Dizziness and/or loss of consciousness
Revealed vs concealed placental abruption
The amount of blood loss often correlates poorly with the degree of abruption.
Abruption may be ‘revealed’ where blood tracks between membranes and out of the vagina. It can however be ‘concealed’ where the blood accumulates with no obvious external bleeding.
Clinical examination
Typical clinical findings in placental abruption include:
- Woody, tense uterus
- Fetal heart: absent or distressed
Investigations
Relevant bedside investigations include:
- Vital signs: respiratory rate, BP, oxygen saturations, pulse and temperature
Relevant laboratory investigations include:
- Full blood count, urea and electrolytes and LFTs: helps to exclude hypertensive conditions such as HELLP or pre-eclampsia
- Clotting profile
- Kleihauer test
- Group and save
- Crossmatch
Relevant imaging investigations include:
- Ultrasound scan: if placental abruption is suspected an ultrasound scan is performed to identify the location of the bleed.
Cardiotocography (CTG) is used to monitor the fetus.
Differential diagnosis
Differential diagnoses for placental abruption include:
- Placenta praevia
- Vasa praevia
- Marginal placental bleed: partial abruption
- Uterine rupture
- Local causes: polyps, carcinoma, cervical ectropion, infection
Management
Table 1. An overview of the management of placental abruption.
| Fetus | Under 36 weeks | Over 36 weeks | |
|
Fetus alive |
No signs of fetal distress |
Observe closely |
Induce and deliver vaginally |
|
Signs of fetal distress
|
Immediate caesarean section
|
||
|
Fetus dead |
Induce vaginal delivery (unless mother haemodynamically compromised and/or ongoing massive haemorrhage, delivery then expedited by caesarean section to arrest bleeding) |
||
Complications
Complications of placental abruption for the mother include:
- Major haemorrhage: if suspected, the major haemorrhage protocol should be activated
- Shock: can result in Sheehan syndrome
- Compression of uterine muscles prevents good contraction of muscles during labour
- Release of thromboplastin from placental haematoma: can lead to disseminated intravascular coagulation (DIC)
- Post-partum haemorrhage
Complications of placental abruption for the fetus include:
- Placental insufficiency: results in hypoxia and intrauterine growth restriction (IUGR) due to lack of nutrients
- Premature birth
- Stillbirth
Key points
- Placental abruption is the complete or partial detachment of the placenta before delivery.
- It presents as painful vaginal bleeding with a woody, tender uterus.
- If suspected, the major haemorrhage protocol should be activated.
- If there are any signs of fetal distress, an immediate caesarean section should be carried out.
Vasa praevia
Introduction
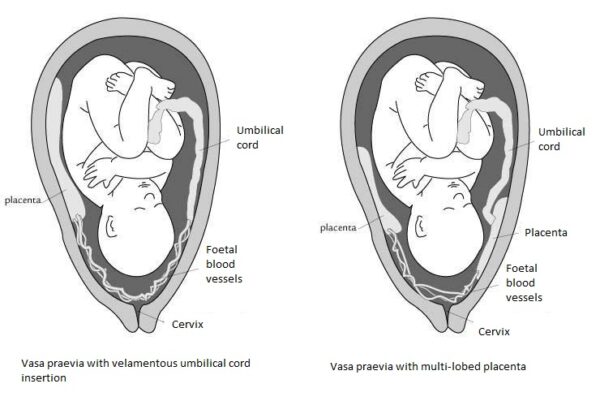
Vasa praevia occurs when fetal blood vessels (the two umbilical arteries and single umbilical vein) are within the fetal membranes and run across the internal cervical os.
Aetiology
Normally, the fetal vessels are protected within the umbilical cord or placenta.
In vasa praevia, the vessels are exposed which increases the risk of the vessels rupturing following rupture of the supporting membranes.2
Types of vasa praevia include:
- Vasa praevia with velamentous umbilical cord insertion: the fetal vessels insert into the membranes and travel round to the placenta, rather than inserting directly into the placenta.
- Vasa previa with multi-lobed placenta: the fetal vessels are exposed as they travel to an accessory placental lobe.
Risk factors
Risk factors for vasa praevia include:2
- IVF pregnancy
- Multiple pregnancy
- Low lying placenta
Clinical features
History
Typical symptoms of vasa praevia include:1
- Painless vaginal bleeding
- Rupture of membranes
- Fetal bradycardia
Clinical examination
Typical clinical findings in vasa praevia include:
- Soft, non-tender uterus
- Fetal bradycardia
Differential diagnosis
Differential diagnoses for vasa praevia include:
- Placenta praevia
- Placental abruption
- Uterine rupture
- Local causes: polyps, carcinoma, cervical ectropion, infection
Investigations
Relevant bedside investigations include:
- Vital signs: respiratory rate, BP, oxygen saturations, pulse and temperature
Relevant laboratory investigations include:
- Full blood count, urea and electrolytes and LFTs: helps to exclude hypertensive conditions such as HELLP or pre-eclampsia
- Clotting profile
- Kleihauer test
- Group and save
- Crossmatch
Relevant imaging investigations include:
- Ultrasound scan
Cardiotocography (CTG) is used to monitor the fetus.
Management
If a woman is found to have vasa praevia on ultrasound, an elective caesarean section at 34-36 weeks is recommended.
In addition to this, corticosteroids are given from 32 weeks gestation to promote fetal lung maturity.2
In the event of APH, an emergency caesarean section is required to deliver the fetus.
Complications
The main complication for vasa praevia is major haemorrhage.
Key points
- Vasa praevia occurs when fetal blood vessels (the two umbilical arteries and single umbilical vein) are within the fetal membranes and run across the internal cervical os.
- Vasa praevia presents with painless vaginal bleeding and can also coincide with the rupture of membranes.
- There are two types of vasa praevia: vasa praevia with velamentous umbilical cord insertion and vasa praevia with multi-lobed placenta.
- If detected on ultrasound scanning, an elective caesarean section is recommended at 34-36 weeks.
Other causes of APH
Other uterine sources of APH include:
- Circumvallate placenta
- Placental sinuses
Other lower genital tract sources of APH include:
- Cervical polyps
- Cervical erosions and carcinoma
- Cervicitis
- Vaginitis
- Vulval varicosities
Summary
Table 2. An overview of the clinical features of placenta praevia, placental abruption and vasa praevia.
|
Placenta praevia |
Placental abruption |
Vasa praevia |
|
Features of haemodynamic shock in keeping with visible blood loss |
Features of haemodynamic shock not in keeping with visible blood loss |
Features of haemodynamic shock in keeping with visible blood loss |
|
No pain |
Pain |
No pain |
|
Non-tender uterus |
Tender uterus |
Non-tender uterus |
|
Abnormal lie and/or presentation |
Normal lie and presentation |
Normal lie and presentation |
|
Fetal heart normal |
Fetal heart absent/distressed |
Fetal bradycardia |
|
Coagulation problems rare |
Coagulation problems present |
Coagulation problems rare |
Reviewer
Dr Joanna Smith
ST7 Obstetrics & Gynaecology
Editor
Dr Chris Jefferies
References
- Royal College of Obstetricians and Gynaecologists. Antepartum Haemorrhage. Green-top Guideline No. 63. London: RCOG; 2011.
- Royal College of Obstetricians and Gynaecologists. Placenta Praevia, Placenta Praevia Accreta and Vasa Praevia: Diagnosis and Management. Green-top Guideline No. 27. London: RCOG; 2011.
- Sigrid de Rooij. Vasa praevia. License: [CC BY-SA]




