- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Strabismus (a.k.a. squint) is an ophthalmic condition in which the eyes do not properly align with each other when focusing to look at an object (i.e. poor fusion). The misalignment may be present occasionally or constantly, commonly with onset from childhood or, less commonly, from adulthood. Strabismus can be subtle, particularly those that are latent (phorias). A patient may present with slight angulation of the head on the visually weaker side to compensate for strabismus.
Strabismus can cause permanent functional disability, psychosocial distress and significantly interfere with social and psychological development, particularly if persistent throughout childhood. This functional disability may manifest as (strabismic) amblyopia, or lazy eye, in which the brain is unable to process inputs from one eye and over time favours the other eye, causing structural changes in the visual pathway and cortex. This ultimately results in decreased or complete loss of vision in an eye that otherwise appears normal.1,2
Early detection and management of strabismus are essential to reduce the risk of functional disability and mitigate the amblyogenic burden.3 This requires all medical practitioners, particularly those working with children, to be competent in recognising potential strabismus so early referral to an ophthalmologist is possible. Treatment options can include observation, optical correction, overminus therapy, prisms, occlusion therapy, vision therapy and surgery.
Table 1. Nomenclature of strabismus
| Term | Meaning |
| amblyopia | 2-line difference from best-corrected visual acuity in a structurally healthy eye |
| tropia / -tropia | Manifest (i.e. always present) disorder of ocular alignment; from Greek, ‘place’ |
| phoria / -phoria | Latent disorder of ocular alignment when binocular fusion is suspended or interrupted; from Greek, ‘to bear’ |
| ortho- | Right; correct; straight |
| hetero- | Other; different |
| heterotropia | Same as ‘tropia’ |
| eso- | Inwards (i.e. nasal horizontal) deviating; |
| exo- | Outwards (i.e. temporal horizontally) deviating; |
| hyper- | Upwards-deviating |
| hypo- | Downwards-deviating |
| cyclo- | Tilted or torsed about an eye’s visual axis |
| comitant | Ocular deviation present in all directions of gaze |
| incomitant | Ocular deviation only present in specific directions of gaze |
Aetiology and epidemiology of strabismus
Aetiology
Common aetiologies of strabismus are described below in Table 2.
Table 2. Aetiologies of strabismus.
| Primary aetiologies of strabismus | Secondary aetiologies of strabismus |
|
|
Interestingly, although amblyopia is a known sequela of long-standing, established strabismus, it itself can be a cause of strabismus. Lower visual experience (sensation, cognition and processing and perception) in an eye can result in that eye drifting out of correct alignment.13
Note that pseudostrabismus (i.e. false strabismus), where an eye may appear turned, often in children, may be due to structural causes that generally resolve with time, as the individual grows. These causes include a broad, flat nose; ocular hypo- or hypertelorism (i.e. abnormally reduced or abnormally increased distance between the eyes) or extraneous skin that covers the medial canthus.
Triggers for intermittent strabismus can include fatigue and stress.
Risk factors
Risk factors for primary strabismus include a family history of strabismus4, low birth weight5,6, premature birth7 and maternal smoking.7,8
Clinical features of strabismus
History-taking
Red flags
- Recent trauma
- Symptoms of raised intracranial pressure (e.g. morning headaches, vomiting)
- New strabismus in a school-age child
History of presenting complaint
- Onset (e.g. dependent on the direction of gaze or time of day)
- Reduced visual acuity
- Diplopia
- Asthenopia (i.e. eye strain, fatigue or pain), particularly in the afternoon or at the end of the day
- Decreased academic and/or work performance
- Decreased socialisation
- Behavioural problems
- Maladjustment at home or school
- Walking difficulties (i.e. bumping into objects, tripping over)
Other important topics
- Obstetric and developmental history
- Previous medical history, including any history of head or ophthalmic trauma, autoimmune or neoplastic conditions, toxin exposure
- Previous visual acuity or ophthalmic testing results
Clinical examination
The physical examination of potential strabismus requires a penlight or other light source and an occluder. The basic physical examination involves the light reflex as well as the cover and cover–uncover tests. Other tests such as the Brückner screening test as well as the prism cover and alternate prism cover tests are also described below. Others such as the Parks–Bielschowski 3-step test can be found in other literature. Factors affecting the performance of the test, such as abnormal head posture, should be noted.
The following elements should be described when characterising a tropia:
- direction;
- laterality (unilateral or alternating, specifying the deviating eye);
- frequency (constant or intermittent);
- comitant or noncomitant (i.e. whether or not the amount of deviation varies according to the direction of the tropia and reflects the normal or defective insertion or function of an extraocular eye muscle/s)
Light reflex test (a.k.a. corneal light reflex test or Hirschberg test)
1. Ask the patient to focus on a target approximately half a metre away whilst you shine a pen torch towards both eyes.
2. Inspect the corneal light reflex on each eye:
- If the ocular alignment is normal, the light reflex will be positioned centrally and symmetrically in each pupil.
- Deflection of the corneal light reflex in one eye suggests a misalignment.
Brückner test
The Brückner test is useful for identifying the presence of small-angle strabismus. At approximately 50 cm away from the patient, the examiner uses a direct ophthalmoscope (DO) with the largest diameter of light to view both of the patient’s red reflexes simultaneously, with the patient’s fixating at a target adjacent to the DO. The lenses on the DO are adjusted until the skin around the eyes is in focus. Asymmetry of the red reflexes — in size, shape, colour and brightness — may suggest an ocular disorder, including strabismus, anisometropia (i.e. imbalance of refractive error) or media opacity that is obstructing the visual axis (e.g. cataract, anterior-chamber or vitreous disorder, coloboma, retinal tumour).
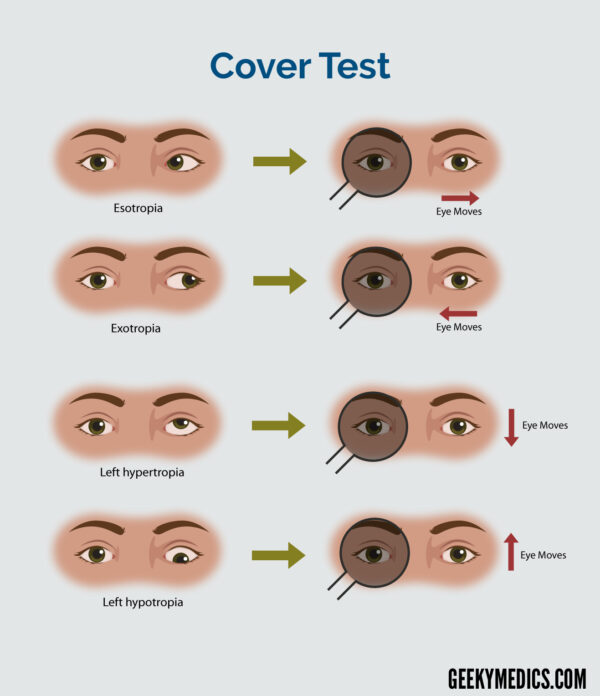
Cover test (a.k.a. single-cover test)
The cover test is used to determine if a heterotropia (i.e. manifest strabismus) is present.
1. Ask the patient to fixate on a target (e.g. light switch).
2. Occlude one of the patient’s eyes and observe the contralateral eye for a shift in fixation:
- If there is no shift in fixation in the contralateral eye, while covering either eye, the patient is orthotropic (i.e. normal alignment).
- If there is a shift in fixation in the contralateral eye, while covering the other eye, the patient has a heterotropia.
3. Repeat the cover test on the other eye.
The direction of the shift in fixation determines the type of tropia; the table below describes the appropriate interpretation.
Table 3. Interpretation of direction at rest and directions of shifts in fixation
| Direction of eye at rest | The direction of shift in fixation of the unoccluded eye when the opposite eye is occluded | Type of tropia present |
| Temporally (i.e. laterally or outwards) | Nasally (i.e. medially or inwards) | Exotropia |
| Nasally (i.e. medially or inwards) | Temporally (i.e. laterally or outwards) | Esotropia |
| Superiorly (i.e. upwards) | Inferiorly (i.e. downwards) | Hypertropia |
| Inferiorly (i.e. downwards) | Superiorly (i.e. upwards) | Hypotropia |
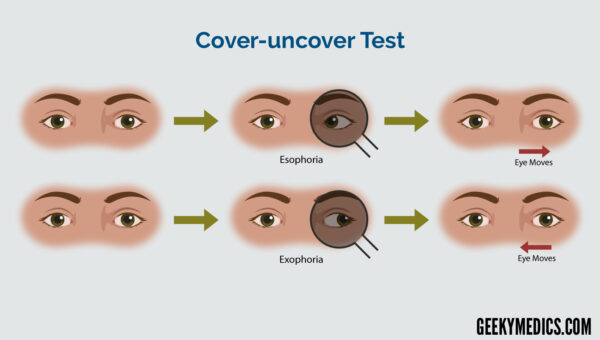
Cover–uncover test (a.k.a. alternate cover test)
The cover–uncover test is used to differentiate if a misalignment is either a tropia or a phoria; that is, if the above cover test demonstrates no tropia, it is used to determine if a phoria (i.e. latent strabismus) is present. Large ones can be associated with asthenopia (i.e. eye strain) and diplopia. Note, small, subtly perceptible phorias are common and non-pathological.
The examiner occludes one eye for approximately 1-2 seconds, then quickly removes the occluder to restore binocular vision. The eye that was previously occluded is observed (rather than the unoccluded eye, as in the cover test) for refixation movement. If a phoria is present, this eye will shift back to being orthotropic (i.e. straight-looking) to re-establish sensory fusion with the other eye.
The speed and smoothness of refixation indicates the strength of fusion.14
Table 4. Interpretation of directions of refixation movements
| The direction of the refixation movement of the occluded eye when occluded and then unoccluded | Type of phoria present |
| Nasally (i.e. medially or inwards) | Exophoria |
| Temporally (i.e. laterally or outwards) | Esophoria |
| Inferiorly (i.e. downwards) | Hyperphoria |
| Superiorly (i.e. upwards) | Hypophoria |
Prism cover test (a.k.a. simultaneous prism cover test)
The prism cover test is used to measure the angle of deviation of a small-angle tropia. The magnitude of the tropia is estimated from the cover and cover–uncover test. A prism (by itself or in a prism bar) underestimating the magnitude is selected.
This prism is placed over the non-fixating eye and is oriented in the same direction as the deviation:
- for an exo- deviation, the prism should be base-in or temporally
- for an eso- deviation, the prism should be base-out or nasally
- for an hypo- deviation, the prism should be base-up
- for a hyper- deviation, the prism should be base-down
Simultaneously, this prism should occlude the fixating eye. The strength of the prism should be increased or decreased until there is no shift in fixation and the deviation is completely reduced. The cover test performed must be brief to avoid suspending binocular fusion, which can make the deviation of a tropia larger due to any imposition of the effect of any phoria.
Alternate prism cover test
An alternate prism cover test is the alternate cover test performed with the prism placed as above. This is used to measure the angle of deviation of a phoria. The prism should decrease the magnitude of refixation movement, as compared with when no prism is used. The strength of the prism is increased until no refixation movement is observed; at this point, the magnitude of the phoria is equal to the strength of the prism.
To confirm the result of the alternate prism cover test, the strength of the prism can be increased such that the direction of the refixation movement is reversed and the strength of the prism is decreased to the previous strength of the prism where there is no refixation movement again.

Further examination
Further examination should include stereopsis, which is the perception of depth and 3-dimensional structure from visual information obtained from both eyes simultaneously. However, as a basic screen by a medic, this usually requires special images called random-dot stereograms and is seldom performed.
References
- Adams GGW, Sloper JJ. Update on squaint and amblyopia. J R Soc Med. 2003;96(1):3-6.
- Niechwiej-Szwedo E, Goltz HC, Chandrakumar M, Wong AMF. Effects of Strabismic Amblyopia and Strabimus Without Amblyopia on Visuomotor Behavior: III. Temporal Eye–Hand Coordination During Reaching. Investigative Ophthalmology & Visual Science. 2014;55:7831-7838.
- Webber AL, Camuglia JE. A pragmatic approach to amblyopia diagnosis: evidence into practice. Clinical and Experimental Optometry. 2018;101(4):451-459.
- Maconachie GDE, Gottlob I, McLean RJ. Risk Factors and Genetics in Common Comitant Strabismus: A Systemic Review of the Literature. JAMA Ophthalmology. 2013;131(9):1179-1186.
- O’Connor AR, Stephenson TJ, Johnson A, Tobin MJ, Ratib S, Fielder AR. Strabismus in Children of Birth Weight Less Than 1701 g. Arch Ophthalmol. 2002;120(6):767–773.
- Gulati S, Andrews CA, Apkarian AO, Musch DC, Lee PP, Stein JD. Effect of Gestational Age and Birth Weight on the Risk of Strabismus Among Premature Infants. JAMA Pediatr. 2014;168(9):850–856.
- Cotter SA, Varma R, Tarczy-Hornoch K, et al. Risk factors associated with childhood strabismus: the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology. 2011;118(11):2251–2261.
- Hakim RB, Tielsch JM. Maternal Cigarette Smoking During Pregnancy: A Risk Factor for Childhood Strabismus. Arch Ophthalmol. 1992;110(10):1459–1462.
- Matsuo T, Yamane T, Ohtsuki H. Heredity Versus Abnormalities in Pregnancy and Delivery as Risk Factors for Different Types of Comitant Strabismus. Journal of Pediatric Ophthalmology and Strabimus. 2001;38(2):78-82.
- Berk AT, Oner FH, Saatci AO. Underlying pathologies in secondary strabimus. Strabismus. 2009;8(2):69-75.
- Capó H, Roth E, Johnson T, Muñoz M, Siatkowski RM. Vertical strabimus after cataract surgery. Ophthalmology. 1996;103(6):918-21.
- Xia Q, Huang Z, Shen DA, Dai H. [Clinical analysis of the diplpia and strabismus after ophthalmic surgeries]. [Zhonghua yan ke za Zhi] Chinese Journal of Ophthalmology, 2003;39(12):727-730.
- Quah BL, Tay MTH, Chew SJ, Lee LKH. A study amblyopia in 18–19 year old males. Singapore Med J. 1991;32:126-129.
- Kanski JJ. Clinical Ophthalmology: A systemic approach. 6th ed. Edinburgh: Elsevier Butterworth–Heinemann; 2007.
- TeamE PFR. Prism bar and fixation stick. Licence: CC BY-SA. Available from: [LINK].