- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Subcutaneous (SC) injections pierce the epidermis and dermis of the skin to deliver medication to the subcutaneous layer. It is a common route of delivery for medications such as insulin and low molecular weight heparin (LMWH). This subcutaneous injection guide provides a step-by-step approach to performing a subcutaneous injection in an OSCE setting, with an included video demonstration. This should not be used as a guide to administering injections to actual patients without first consulting your local medical school or hospital guidelines and undertaking the necessary training.
Gather equipment
Gather the appropriate equipment:
- Non-sterile gloves
- Apron
- Equipment tray
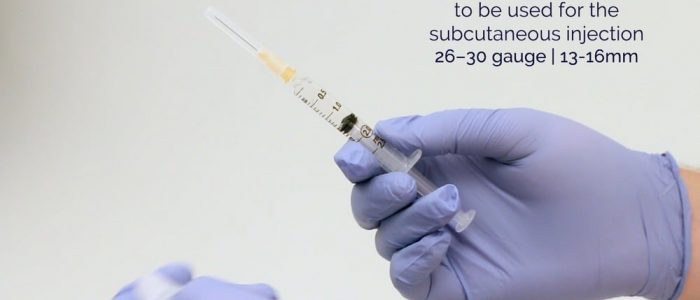
- Syringe (the smallest syringe that will accommodate the medication volume)
- Injecting needle (26–30 gauge): a standard length is 13-16mm. ¹
- Drawing-up needle (also known as a blunt filter needle): filters out sub-visible particles of glass, rubber and other residues when drawing up medications from ampoules.
- Gauze or cotton swab
- Sharps container
- The medication to be administered
- The patient’s prescription
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the procedure will involve using patient-friendly language: “Today I need to administer some medication, this will involve an injection under the skin. You may briefly experience a sharp scratch as the needle is inserted. The procedure does involve some risks which include bleeding, bruising, a persistent lump at the injection site and a small chance of infection or serious allergic reaction.”
Check the patient’s understanding of the medication being administered and explain the indication for the treatment.
Gain consent to proceed with the subcutaneous injection.
Check if the patient has any allergies.
Ask if the patient has a preferred injection site. If the patient is receiving regular subcutaneous injections, ensure that the injection sites are rotated.
Adequately expose the planned injection site for the procedure.
Position the patient so that they are sitting comfortably.
Ask the patient if they have any pain before continuing with the clinical procedure.
Final checks
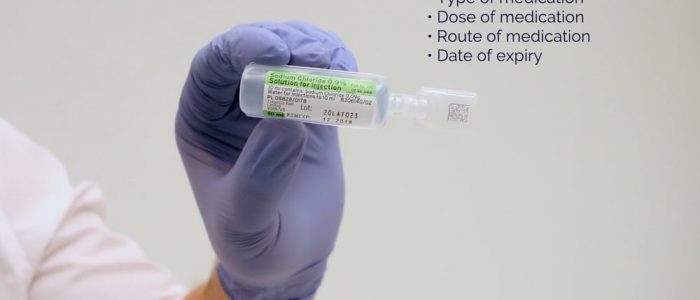
Before proceeding, check the seven rights of medication administration.
1. Right person: ask the patient to confirm their details and then compare this to the patient’s wrist band (if present) and the prescription. You should use at least two identifiers.
2. Right drug: check the labelled drug against the prescription and ensure the medication hasn’t expired.
3. Right dose: check the drug dose against the prescription to ensure it is correct.
4. Right time: confirm the appropriate time to be administering the medication and check when the patient received a previous dose if relevant.
5. Right route: check that the planned route is appropriate for the medication you are administering.
6. Right to refuse: ensure that valid consent has been gained prior to medication administration.
7. Right documentation of the prescription and allergies: ensure that the prescription is valid and check the patient isn’t allergic to the medication you are going to administer.
Once all of the above have been confirmed prepare the medication.
Performing the subcutaneous injection
1. Wash your hands and don some gloves (if not already done).
2. Draw-up the appropriate medication into the syringe using a drawing-up needle.
3. Remove the drawing-up needle and immediately dispose of it into a sharps bin, then attach the needle to be used for performing the injection.
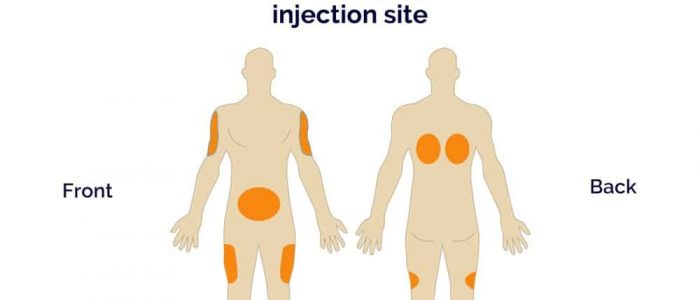
4. Choose an appropriate site for the injection: ¹
- Abdomen: avoid injecting within a 2-inch radius around the umbilicus (this is the preferred site if administering low molecular weight heparin).
- Upper outer aspect of the arm
- Outer aspect of the upper thigh
- Upper buttock
- Do NOT use a site that is scarred, inflamed, irritated or bruised.
If multiple injections need to be administered, use different sites for each subsequent injection. If frequent injections are administered, rotate injection sites.
5. Position the patient to provide optimal access to your chosen site.
6. Cleaning the site:
- WHO does not recommend the routine use of alcohol-based cleansing wipes prior to administration of subcutaneous medication as this can predispose an individual to develop hardened skin at the injection site. ²,³
- If the skin is visibly soiled it should be cleaned with soap and water.
- Routine cleaning is not usually required prior to subcutaneous injection.
- In older patients and those who are immunocompromised, skin preparation using an alcohol-impregnated swab (70% isopropyl alcohol) may be recommended. 4
7. Pinch a 5cm fold of skin between the thumb and index finger, using your non-dominant hand (pinching the skin increases the depth of the subcutaneous tissue available).
8. Warn the patient of a sharp scratch.
9. Pierce the skin at a 45-90° angle, aiming to remain in the subcutaneous tissue layer. Insert the needle quickly and firmly, with the bevel facing upwards.
10. Inject the contents of the syringe whilst holding the barrel firmly. Aspiration is not recommended for subcutaneous injections, as there are no major blood vessels in the subcutaneous tissue and the risk of inadvertent intravenous administration is minimal.5 You should, however, always follow your local guidelines.
11. Remove the needle and immediately dispose of it into a sharps container.
12. Apply gentle pressure over the injection site with a cotton swab or gauze and avoid rubbing the site.
13. Replace the gauze with a plaster.
14. Dispose of your equipment into an appropriate clinical waste bin.
To complete the procedure…
Explain to the patient that the procedure is now complete.
Thank the patient for their time.
Discuss post-injection care:
- Warn the patient that it is normal for the injection site to be sore for one or two days. Advise that if they experience worsening pain after 48 hours they should seek medical review.
- Reiterate the potential complications of subcutaneous injections including haematoma formation, persistent nodules, local irritation and rarely anaphylaxis.
Dispose of PPE appropriately and wash your hands.
Document the details of the procedure and the medication administered.
Reviewer
Graham Bone
Senior Clinical Lecturer in Medical Education
References
- BD. Subcutaneous Injection Guidelines for Needle Length and Gauge Selection. Published in 2012. Retrieved from: [LINK].
- World Health Organisation – WHO Best Practices for Injections and Related Procedures Toolkit. Retrieved from: [LINK].
- Best infection control practices for intradermal, subcutaneous, and intramuscular needle injections. Yvan Hutin et al. 2003. Retrieved from: [LINK].
- Dougherty L, Lister S (2015) The Royal Marsden Manual of Clinical Nursing Procedures. Oxford: Wiley-Blackwell.
- Public Health England (2013) Immunisation Procedures: The Green Book, Chapter 4. Retrieved from: [LINK].