- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Testicular cancer is the most common malignancy in men aged 15-45 years.1
Overall, it is a rare malignancy and represents about 1% of adult cancers. If diagnosed early, testicular cancer has a 95% overall relative 5-year survival rate.2
However, testicular cancer rates are increasing globally, emphasising the crucial importance of early detection and effective treatment.1
Aetiology
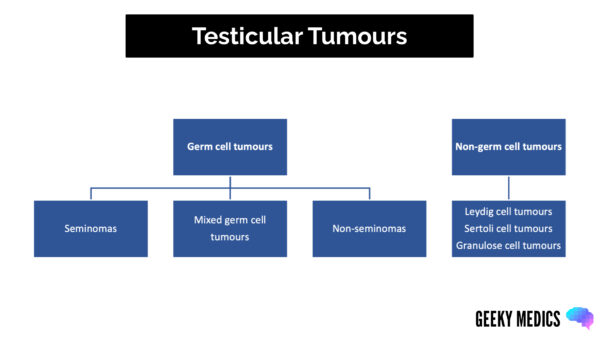
Classification of testicular tumours
Primary testicular tumours can be categorised depending on the histopathological analysis of the tumour, illustrated in Figure 1.3
Risk factors
The most common risk factors for testicular cancer include:4.5
- Cryptorchidism (unilateral: 4x increased risk, bilateral: 10x increased risk)
- Prior history of testicular cancer (contralateral germ cell tumour: 8x increased risk)
- Family history (1st degree male relative: 6x increased risk)
- Subfertility
- Klinefelter syndrome
- Kallman syndrome
- Prenatal oestrogen exposure
Clinical features
History
Testicular cancer usually presents as a unilateral painless testicular lump as an incidental finding. It can also present with dull or acute testicular pain.
Patients with metastases may present with additional symptoms, including:
- Unintentional weight loss
- Back pain (due to skeletal metastasis)
- Dyspnoea (due to lung metastases)
Clinical examination
Typical characteristics of testicular cancer on testicular examination include:6
- Unilateral painless testicular lump
- Irregular, firm and fixed
- Does not transilluminate
Occasionally, the testicle cannot be completely palpated due to a hydrocele.7
Evidence of metastases may present with a history of unintentional weight loss, back pain or dyspnoea.
Assessing testicular lumps
Assessment of a testicular lump should include the 6 Ss:
- Site
- Size
- Shape
- Symmetry
- Skin change
- Scars
Differential diagnoses
A hard testicular mass is diagnostic of testicular cancer until proven otherwise. However, other differential diagnoses should be considered when evaluating a testicular lump.
Table 1. Differential diagnoses to consider for a testicular lump.7
| Differential diagnosis | Clinical summary |
| Epididymo-orchitis | Inflammation of both the epididymis and ipsilateral testes |
| Hydrocele | Abnormal collection of fluid between the parietal and visceral layers of the tunica vaginalis, which surrounds the testes and spermatic cord |
| Varicocele | Dilated tortuous veins of the pampiniform plexus that drain the testicles |
| Inguinal hernia | Hernia (protrusion) of abdominal contents through the inguinal canal |
Investigations
Tumour markers
Tumour markers can be diagnostic and prognostic. Half-life decline is useful following orchidectomy when assessing for residual disease:8,9
- Beta HCG (half-life: 36 hours) is elevated in 30-50% of non-germ cell tumours and 5-10% of seminomas
- AFP (half-life: 5 days) can be raised in non-germ cell tumours but not in seminomas
- LDH can also be a surrogate marker for tumour volume and necrosis and can also be used to assess tumour response to oncological treatment
Imaging
Relevant imaging investigations include:
- Trans-scrotal ultrasound: used for the initial investigation of scrotal lumps and has over 90% sensitivity in diagnosis
- Computed tomography (CT) with contrast of the chest, abdomen, and pelvis: to stage the disease
Management
Every patient diagnosed with testicular cancer should be discussed in a specialist MDT, and the mainstays of treatment include surgery, active surveillance or chemotherapy.
When a diagnosis of testicular cancer is suspected based on physical examination, ultrasound findings and tumour markers, radical inguinal orchidectomy is the initial management option.10 This involves the removal of the testicle, epididymis and spermatic cord up to the level of the internal inguinal ring. Before this procedure, patients should be counselled on sperm banking and cryopreservation as well as testicular prostheses.11
Tumour staging and histopathological results guide further management with options including active surveillance, chemotherapy, retroperitoneal lymph node dissection and radiation therapy.12
Complications
Complications due to testicular malignancy can be due to the disease itself or from treatment.
Disease-related complications include:13
- Metastases
- Psychosocial impact
Treatment-related complications include:14
- Hypogonadism and infertility
- Secondary malignancies (from radiotherapy/chemotherapy)
- Peripheral neuropathy
- Surgical complications (e.g. bleeding, infection)
The histology, extent of tumour spread and elevation of tumour markers largely determine prognosis.
Key points
- Testicular cancer is one of the most common malignancies in men aged 15 to 45
- Complex environmental and genetic factors can contribute to the development of testicular cancer, commonly including cryptorchidism, family history and prior history of testicular cancer
- Initial assessment of a patient includes taking a history, physical examination, tumour marker levels and trans-scrotal ultrasound
- Radical inguinal orchidectomy is performed for both diagnostic and therapeutic purposes
- Tumour type and staging guide further management following surgery
Reviewer
Mr Chaitya Desai
Urology Registrar
Editor
Dr Chris Jefferies
References
- Park, J.S., et al., Recent global trends in testicular cancer incidence and mortality. Medicine (Baltimore), 2018. 97(37): p. e12390.
- Rovito, M.J., et al., A Cross-Sectional Analysis of Testicular Cancer Symptom Recognition and Stage of Diagnosis. Am J Mens Health, 2022. 16(3): p. 15579883221104900.
- Berney, D.M., et al., An introduction to the WHO 5th edition 2022 classification of testicular tumours. Histopathology, 2022. 81(4): p. 459-466.
- Cheng, L., et al., Testicular cancer. Nat Rev Dis Primers, 2018. 4(1): p. 29.
- Yazici, S., et al., Risk Factors for Testicular Cancer: Environment, Genes and Infections-Is It All? Medicina (Kaunas), 2023. 59(4).
- Stephenson, A., et al., Diagnosis and Treatment of Early Stage Testicular Cancer: AUA Guideline. J Urol, 2019. 202(2): p. 272-281.
- Baird, D.C., G.J. Meyers, and J.S. Hu, Testicular Cancer: Diagnosis and Treatment. Am Fam Physician, 2018. 97(4): p. 261-268.
- Milose, J.C., et al., Role of biochemical markers in testicular cancer: diagnosis, staging, and surveillance. Open Access J Urol, 2011. 4: p. 1-8.
- Dieckmann, K.P., et al., Serum Tumour Markers in Testicular Germ Cell Tumours: Frequencies of Elevated Levels and Extents of Marker Elevation Are Significantly Associated with Clinical Parameters and with Response to Treatment. Biomed Res Int, 2019. 2019: p. 5030349.
- Patrikidou, A., et al., European Association of Urology Guidelines on Testicular Cancer: 2023 Update. Eur Urol, 2023. 84(3): p. 289-301.
- Williams, D.H., Sperm banking and the cancer patient. Ther Adv Urol, 2010. 2(1): p. 19-34.
- Albers, P., et al., Guidelines on Testicular Cancer: 2015 Update. Eur Urol, 2015. 68(6): p. 1054-68.
- Mykletun, A., et al., Side effects and cancer-related stress determine quality of life in long-term survivors of testicular cancer. J Clin Oncol, 2005. 23(13): p. 3061-8.
- Fung, C. and D.J. Vaughn, Complications associated with chemotherapy in testicular cancer management. Nat Rev Urol, 2011. 8(4): p. 213-22.