- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The visual pathway is the route by which retinal stimuli are transferred to the occipital cortex of the brain. It encompasses the retina, optic nerve, optic chiasm, optic radiations and the visual centre of the occipital lobe.
Understanding the anatomy of the optic nerve and visual pathways is key to appreciating how various focal lesions of the brain cause characteristic visual field defects.
Visual fields
When discussing vision, it is important to understand the visual field and how it differs from the image presented to the retina.
The visual field is the entire area that can be seen by a patient without movement of their head and with their eyes fixed on one point.
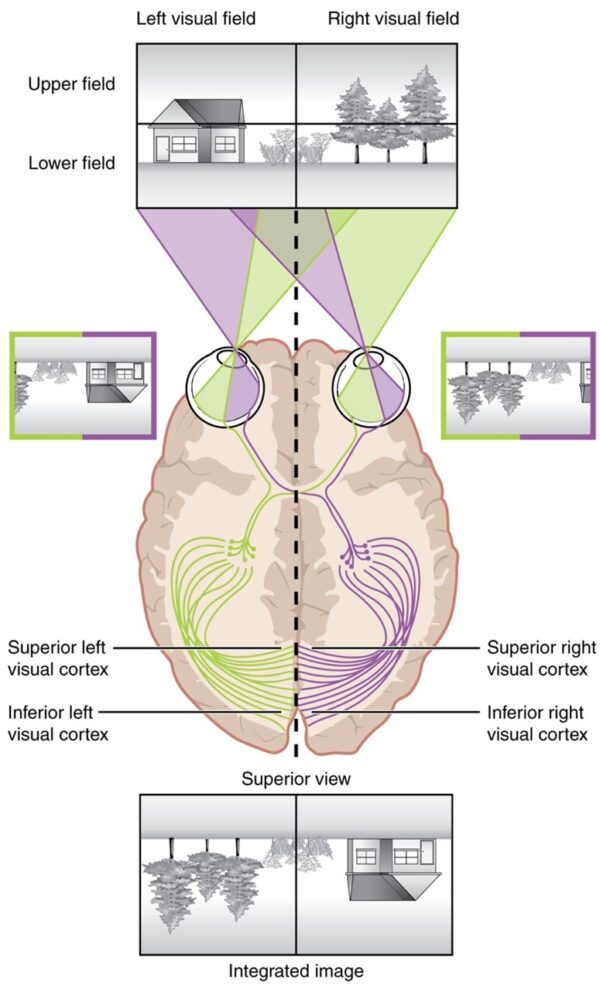
The image of an object in the visual field is inverted upside-down and flipped left-to-right on the retina, as illustrated in figure 1.
Confrontational assessment of the visual field is an important part of the cranial nerve examination. It can be more accurately assessed using perimetry studies.
Visual pathway
The photoreceptors (rods and cones) in the retina are stimulated by photons of light entering the eye. Light-sensitive surface membrane proteins (e.g. rhodopsin) of these cells are stimulated to propagate second messenger responses which convert light energy into electrical signals. The photoreceptors synapse with retinal bipolar cells, which in turn transmit these signals to retinal ganglion cells.
The retinal ganglion cells converge at the optic disc, forming the optic nerve. The optic nerve then exits the eye, travelling through a defect in the lamina cribrosa of the sclera.
The optic nerve is the second cranial nerve, responsible for transmitting the special sensory information for vision. It may be considered an extension of the forebrain as it is covered by the meninges of the central nervous system, rather than by epi/peri/endoneurium like other peripheral nerves.
The optic nerve travels through the bony orbit and enters the middle cranial fossa through the optic canal, a defect in the lesser wing of the sphenoid.
Once inside the skull, the optic nerve travels along the floor of the middle cranial fossa, through the medial aspect of the cavernous sinus. Left and right optic nerves then converge at the optic chiasm.
The optic chiasm is located directly above the sella turcica of the sphenoid bone. The pituitary gland projects down immediately behind the chiasm.
At the chiasm, fibres from the nasal aspect of each retina cross over (or decussate) to the contralateral optic tract, while fibres from the temporal retina remain on their respective sides, as illustrated in figure 2.
In this way, left-sided post-chiasmal fibres pertain to the right side of the visual field, and vice versa.
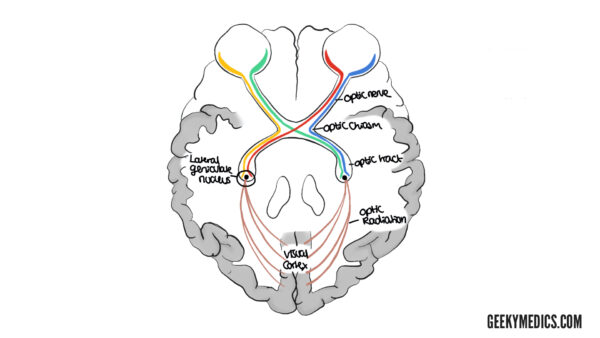
The optic tracts extend from the chiasm to the thalamus. Here, afferent sensory nerves from the eye synapse with the second-order sensory neurones at the lateral geniculate nucleus in the thalamus. From here, the sensory nerves radiate dorsally to the calcarine sulcus of the occipital lobe.
Optic radiations loop either through the parietal lobe or through the temporal lobe (Meyer’s loop).
As illustrated in figure 3, radiations travelling through the parietal lobe correspond to the upper half of the retina/lower visual field, while the radiations travelling through Meyer’s loop in the temporal lobe correspond to the bottom half of the retina/upper visual field.

The optic radiations terminate in the calcarine sulcus of the occipital lobe, where the cortical visual centre is situated.
The calcarine sulcus is responsible for retinal image processing. Here, images from both eyes are finally collated and a final image is formed. This image is inverted, as represented in figure 1. As a consequence of this, the brain has to re-invert the image so that information is correctly oriented in space.
From the occipital visual centre, signals are sent to the frontal, parietal and temporal lobes to further make sense of the input information (e.g. reading/facial recognition).
Blood supply
The blood supply of the visual pathway is outlined in table 1.
Table 1. Blood supply of the visual pathway.
| Locus of the visual pathway | Blood supply |
|
Optic nerve |
Ophthalmic artery |
|
Optic chiasm |
Branches from:
|
|
Optic tract |
Middle cerebral artery (MCA) |
|
Lateral geniculate nucleus |
Anterior choroidal branches of the MCA
Thalamogeniculate branches of the posterior cerebral artery (PCA) |
|
Optic radiations |
MCA |
|
Calcarine sulcus |
Mostly by the PCA. The MCA also helps supply the anterior portion, which corresponds to the macula. |
Visual field defects
As described above, components of the visual pathway carry information corresponding to specific regions of the visual field. Destructive lesions of the visual pathway, therefore, result in characteristic visual field defects.
As a rule, pre-chiasmal lesions will result in an ipsilateral monocular visual field defect. Post-chiasmal lesions will result in homonymous visual field defects of the contralateral side.
Lesions of the chiasm most commonly result in bitemporal hemianopia, as demonstrated in figure 4.
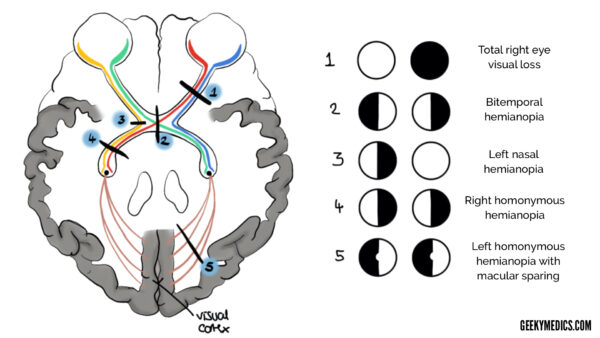
At the optic chiasm, fibres from the nasal half of the retina, corresponding to the temporal visual field, decussate. Lesions compressing the chiasm, such as pituitary adenomas, therefore cause bitemporal hemianopia.
Lesions to optic radiations result in homonymous contralateral quadrantanopia. Those affecting Meyers loop in the temporal lobe result in a homonymous upper quadrantanopia (“pie in the sky”), while those affecting the parietal lobe cause a lower quadrantanopia (“pie on the floor”).
Lesions affecting the calcarine sulcus of the occipital lobe tend to cause homonymous hemianopia with sparing of the macula. Macular vision is spared given the dual blood supply to the anterior portion of the visual centre (PCA and MCA).
Table 2 describes the typical visual field defects associated with lesions along the visual pathway.
Table 2. Lesions of the visual pathway and their respective visual field defects.
| Site of lesion/pressure | Field defect | Typical lesions |
|
Optic nerve |
Ipsilateral monocular blindness |
Optic neuritis Amaurosis fugax Optic atrophy Retrobulbar optic neuropathy Trauma |
|
Optic chiasm (central) |
Bitemporal hemianopia |
Pituitary adenoma Suprasellar aneurysm |
|
Optic chiasm (lateral) |
Ipsilateral monocular nasal hemianopia |
Distension of the 3rd ventricle Internal carotid/posterior communicating artery atheroma |
|
Optic tract |
Contralateral homonymous hemianopia |
MCA stroke Tumours |
|
Optic radiation |
Contralateral homonymous quadrantanopia |
MCA stroke Tumour Trauma |
|
Occipital cortex |
Contralateral homonymous hemianopia with macular sparing |
PCA stroke Trauma |
Key points
- The visual pathway comprises the retina, optic nerve, optic chiasm, optic radiations, and the visual centre in the occipital lobe.
- Optic nerve lesions tend to cause ipsilateral monocular blindness.
- At the optic chiasm, fibres from the nasal half of the retina, corresponding to the temporal visual field, decussate. Lesions compressing the chiasm, such as pituitary adenomas, therefore cause bitemporal hemianopia.
- Lesions to the optic radiations result in contralateral quadrantanopia. Those affecting Meyer’s loop result in upper quadrantinopia (“pie in the sky”), while those affecting radiations through the parietal lobe result in lower quadrantinopia (“pie on the floor”).
- Lesions affecting the calcarine sulcus of the occipital lobe tend to cause homonymous hemianopia with sparing of the macula.
Reviewer
Neurology registrar
Editor
Dr Chris Jefferies
References
- OpenStax College. Topographical Image on Retina. License: [CC-BY]. Available from: [LINK]
- Ratznium. ERP – optic cabling. License: [CC BY-SA]. Available from: [LINK]
- Snell R. S., Lemp M.A. (2016). Clinical Anatomy of the Eye, 2nd Edition. Wiley Blackwell.
- Batterbury M. Murphy C. (2019). Ophthalmology 4th Edition. Elsevier.
- Forrester. (2015). The Eye: Basic Sciences in Practice 4th Edition. Elsevier.




