- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Table of Contents
This guide provides a general overview of wound dressing types including the advantages and disadvantages of each. Please follow local guidelines and consult the wound management formulary in your organisation. Further advice may be obtained from the tissue viability team.
Background
Wound healing
Wound healing is a complex process that involves multiple stages. The principal stages of wound healing include:
- Haemostasis: vasoconstriction and activation of the coagulation cascade to prevent further bleeding
- Inflammation: neutrophils, macrophages and a range of other cell types enter the wound to maintain its cleanliness and attract other cell types
- Cell proliferation: granulation tissue provides a scaffold for the formation of new blood vessels (re-vascularisation)
- Epithelialisation: epithelial cells migrate from the wound edges to cover the wound defect
- Tissue remodelling: iterative breakdown and rebuilding of the wound’s extracellular matrix resulting in gradual improvement in the tensile strength of the wound
It’s important to understand the wound healing process as this can inform the choice of an appropriate dressing (e.g. a moist environment is essential for cell proliferation and epithelialisation in particular).
See our wound healing overview for more details.
Assessing a wound
Inspection of a wound can provide clues as to the current stage of healing and the presence of additional factors which may impair the healing process such as infection:
- Pink (epithelialisation phase)
- Red (granulation/proliferation phase)
- Yellow (sloughy/granulation phase)
- Black (necrotic tissue/eschar)
- Wounds with signs of infection (e.g. offensive smell, excess pus, spreading erythema)
Assessing a dressing type
There are a few things you should consider when assessing a wound dressing:
- What is the action of the dressing?
- When should it be used?
- Are there any contra-indications to its use?
- What is the method of application and removal?
- Is a secondary dressing required and if so, what type?
Characteristics of an ideal wound dressing
An ideal wound dressing:
- promotes moist wound healing
- manages excess exudate
- provides thermal insulation
- is impermeable to micro-organisms
- causes minimal trauma on removal
- is cost-effective
- is easily available
Types of wound dressing
A primary dressing refers to the dressing in direct contact with the wound surface.
A secondary dressing refers to a dressing which fixes the primary dressing in place; it may also assist with other tasks such as the absorption of wound exudate.
The use of a primary and secondary dressing together is often referred to as a combined dressing.
Simple island dressings
Simple island dressings consist of a basic absorbent wound pad with an adhesive backing.
These types of dressing are only appropriate for wounds in which the edges are closely re-approximated (i.e. close together/healing by primary intention). These dressings are typically used to cover a wound that has been closed by sutures.
Simple island dressings should not be used in the context of open wounds.
It is important to clarify if the patient has any allergies before applying a simple island dressing due to the presence of adhesive (this is true for all dressings that contain adhesive).
Advantages
- Useful for wounds in which the edges are closely re-approximated such as post-operative incisions
- Can absorb small amounts of wound exudate
- Provide a covering for the wound
Disadvantages
- Not appropriate for open wounds or those with excessive exudate
Appropriate wound types
- Closely approximated wounds (e.g. surgical incisions with sutures or skin tears) healing via primary intention
Examples
Some examples of simple island dressings include:
-
Alldress®
-
Primapore®
Non-adherent wound contact layer dressings
Non-adherent wound contact layer dressings (sometimes referred to as ‘non-adherent dressings’) are designed to minimise sticking to the drying exudate of the wound, resulting in less trauma and pain when the dressing is removed.
Non-adherent dressings are typically used to directly cover the wound bed with a secondary absorbent dressing placed over the non-adherent dressing to absorb exudate and fix the primary dressing in place.
Non-adherent dressings are most suitable for clean, granulating, lightly exuding wounds without necrosis.
Advantages
- Protect the wound bed from direct contact with secondary dressings.
Disadvantages
-
Limited ability to absorb exudate and require a secondary dressing
Appropriate wound types
- Superficial wounds healing by secondary intention
- Burns
- Leg ulcers
Examples
Some examples of low-adherence dressings include:
-
Mepitel®
-
Atrauman®
Films & membranes
Film and membrane dressings allow the passage of water vapour and oxygen through them, which can help reduce the risk of maceration of tissue due to excessive moisture and provide oxygen to assist with the wound healing process.
These types of dressings also provide visibility of the wound, without the need to remove the dressing, which can be useful for monitoring the healing process and early recognition of problems such as infection.
Their ability to absorb exudate is typically limited, and removal can result in tissue damage due to adherence.
Advantages
- Allow passage of water vapour reducing the risk of maceration
- Allow passage of oxygen to facilitate the healing process
- Provide visibility of the wound
Disadvantages
- Limited ability to absorb exudate
Appropriate wound types
- Epithelialising wounds
- Superficial wounds with small amounts of exudate
Examples
Some examples of film and membrane dressings include:
-
Mepore® Film
-
Hydrofilm®
-
Tegaderm®
Moist dressings
Moist dressings work by either preventing the loss of moisture from the wound or donating moisture to the area directly.
The two primary subtypes of moist dressings are:
- Hydrocolloid dressings
- Hydrogel dressings
Both hydrocolloid and hydrogel dressings work by stimulating autolytic debridement which involves the breakdown of damaged proteins, fibrin, collagen and cells within the wound by the immune system (e.g. neutrophils, macrophages – see our guide).
Hydrocolloid dressings
When a hydrocolloid dressing comes into contact with wound exudate, the hydrocolloid component of the dressing becomes a gel. This gel then creates a waterproof seal that prevents moisture loss from the wound through evaporation.
Dressings should be large enough to fully cover the wound with some additional margin (at least 2cm) to ensure an adequate seal is established.
Hydrocolloid dressings can be left in place for up to 7 days.
Advantages
- Maintain wound hydration by preventing the loss of moisture
- Create an optimum healing environment (warm and moist)
Disadvantages
- Can lead to skin maceration due to excessive moisture
Appropriate wound types
- Superficial wounds with low to medium levels of exudate
Examples
Some examples of hydrocolloid dressings include:
-
Granuflex®
-
Tegaderm Hydrocolloid®
Hydrogel dressings
Hydrogel dressings contain water in a gel form.
The amount of water contained within the dressing varies but is typically 60-70%.
Hydrogel dressings are ideal for wounds that contain necrotic tissue, as this is often desiccated. The water from the hydrogel is absorbed by the necrotic tissue which then softens and is easier for the body to break down through the previously described process of autolytic debridement.
A hydrogel dressing should be large enough to cover the wound with a minimum of a 3cm margin.
A secondary dressing such as a film or hydrocolloid dressing should be used to hold the hydrogel dressing close to the wound bed.
Hydrogel dressings need to be changed every 2-3 days on average.
Advantages
- Facilitate the breakdown of necrotic tissue through rehydration and subsequent softening.
Disadvantages
- Excessive use of hydrogel dressings can cause skin maceration.
Appropriate wound types
- Wounds with desiccated necrotic tissue (if the aim is to debride)
Examples
Some examples of hydrogel dressings include:
-
Kerralite Cool®
-
Intrasite Gel®
Absorbent dressings
Absorbent dressings function to absorb and contain wound exudate.
If wound exudate is not managed appropriately, it can result in skin maceration, poor dressing adherence and leaking.
There is a wide range of absorbent dressings available which vary in shape, size and absorbancy.
Absorbent dressings should be applied to a dry wound bed, meaning excess exudate should ideally be cleaned away prior to the application where appropriate.
Hydrofiber dressings
Hydrofiber dressings are comprised entirely of sodium carboxymethylcellulose fibres (known as Hydrofiber®). Hydrofiber dressings are an evolution of the hydrocolloid dressings mentioned above, with the difference being that they are made entirely of hydrocolloid and thus have a much greater ability to absorb wound exudate.
When Hydrofiber absorbs wound exudate it transforms into a gel-like sheet.
Hydrofiber dressings are typically used on moderate to heavily exuding wounds and must be changed once fully saturated.
Hydrofiber dressings are commonly used to pack cavity wounds, as they are absorbent, a secondary dressing is required.
Advantages
- Effective for moderate to high levels of exudate
- Aids moist wound healing and autolytic debridement
- Haemostatic
- Creates a warm, moist environment
Disadvantages
- Can sometimes stick to the edges of a wound causing tissue damage on removal if used inappropriately
Appropriate wound types
- Wounds with medium to high levels of exudate
- Dehisced surgical wounds
- Abscess cavities
Examples
Some examples of Hydrofiber dressings include:
-
Aquacel®
Alginate dressings
Alginic acid, also called algin, is a naturally occurring polysaccharide that is refined from brown seaweeds.
Alginate dressings absorb wound exudate and form a gel-like covering over the wound to facilitate the healing process, similar to Hydrofiber dressings.
There are a variety of alginate dressing subtypes, some of which form a gel layer which can later be removed in one piece and others that disintegrate and need to be irrigated to remove them from the wound.
Alginate dressings need to be used in combination with a secondary dressing to hold the alginate dressing close to the wound bed.
Advantages
- Helps to debride wound via stimulation of macrophages
- Absorbs and retains fluid effectively
- Easy to apply and remove
- Haemostatic
Disadvantages
- Can dry out the wound
- Fibres can stick to the wound bed
- Can result in skin maceration
- May sting on contact with the wound
- Has an odour when it becomes wet
Appropriate wound types
- Pressure ulcers
- Venous ulcers
- Bleeding wounds
- Excessively exudative wounds
Examples
Some examples of alginate dressings include:
-
Tegaderm® Alginate
-
Algisite M®
- ActivHeal® Alginate
Foam dressings
Foam dressings absorb exudate and either transform it into a gel-like foam or absorb the exudate into the core of the dressing, effectively removing it from the wound bed. Foam dressings can be adhesive or non-adhesive.
Foam dressings need to be changed when they become saturated or show up to 75% strikethrough.
Advantages
- Do not stick to the wound surface
- Manage excess exudate effectively whilst avoiding excessive drying
- Creates a warm, moist environment
Disadvantages
- Do not hold large amounts of exudate
- May cause odour when wet
- Adhesive dressing can cause skin stripping to fragile skin
Appropriate wound types
- Wounds with medium to high levels of exudate
Examples
Some examples of foam dressings include:
-
ActivHeal® Foam Adhesive
-
PolyMem®
- Allevyn gentle®
Antimicrobial dressings
For local wound infection, a topical antimicrobial dressing can be used to reduce the level of bacteria at the wound surface but will not eliminate a spreading infection.
Some dressings are designed to release the antimicrobial into the wound, others act upon the bacteria after absorption from the wound.
The amount of exudate present and the level of infection should be taken into account when selecting an antimicrobial dressing.
Medical-grade honey has antimicrobial and anti-inflammatory properties. Dressings impregnated with iodine can be used to treat clinically infected wounds. Dressings containing silver should be used only when clinical signs or symptoms of infection are present.
Silver, honey and iodine may come impregnated in hydrocolloids, hydrofibers, alginates and foams (as above). They vary in absorbency. Antimicrobials should only be used in the short term (up to 2 weeks) and be regularly reviewed.
Advantages
- Inhibit bacterial growth and kill surface bacteria
- Can reduce odours if caused by bacteria
Disadvantages
- Risk of an allergic reaction
- Potential for antimicrobial resistance developing
- Limited ability to absorb exudate
Appropriate wound types
- Wounds with local infection/bacterial colonisation
Examples
Some examples of antimicrobial dressings include:
-
Inadine®
-
Activon Tulle®
- Aquacel Ag®
Odour absorbent dressings
Odour absorbent dressings, as the name suggests, are typically used in cases where wound odour is causing significant distress to the patient. They are more effective at reducing smells emanating from the wound, and they can be applied to the outside of secondary dressings.
These types of dressings typically stop functioning if they become wet.
Advantages
- Can reduce wound odours
Disadvantages
- Stop functioning when they become wet
Appropriate wound types
- Severely malodorous wounds
Examples
Some examples of odour absorbent dressings include:
-
CarboFLEX®
-
CliniSorb® Odour Control Dressings
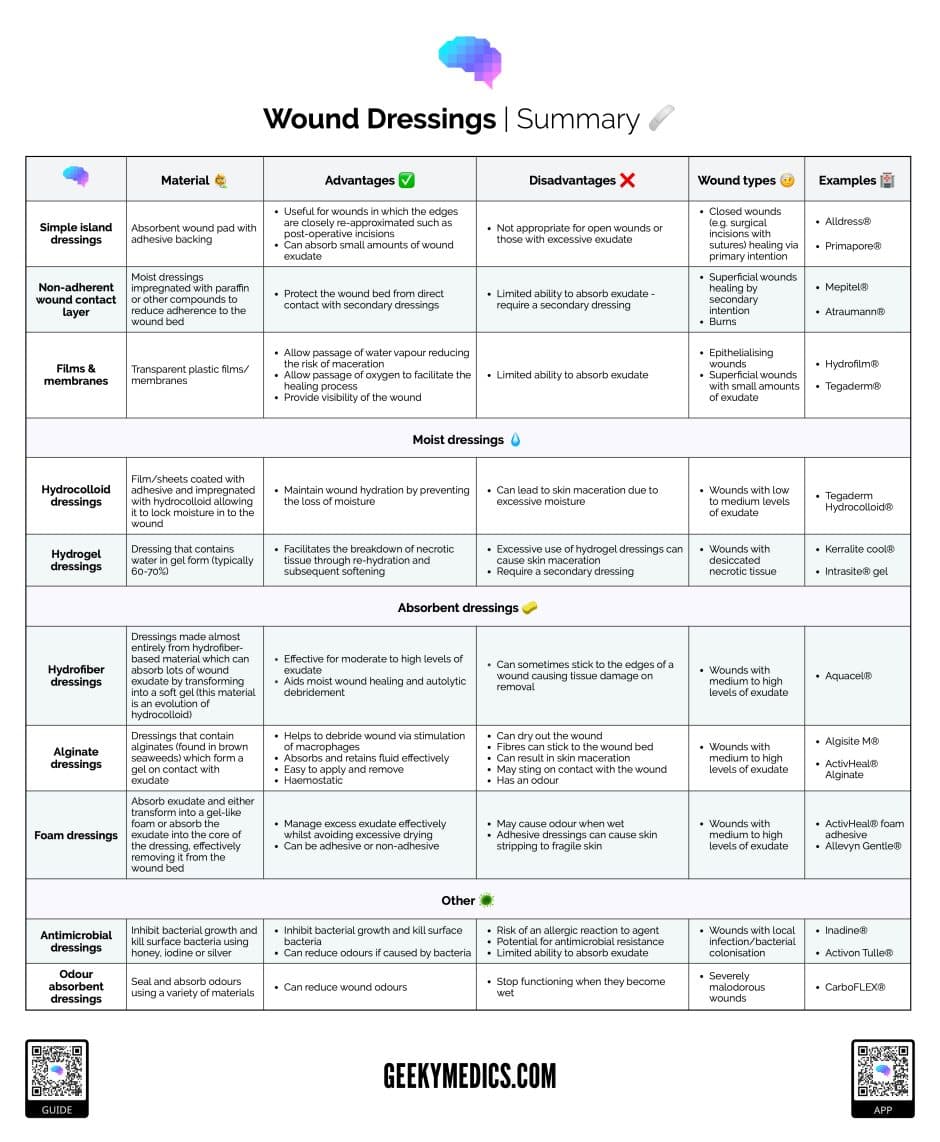
Summary table of dressing types
References
- British National Formulary (BNF). Wound Management. Available from: [LINK].
- Jones V, Grey JE, Harding KG. Wound dressings. BMJ. 2006 Apr 1;332(7544):777-80. DOI: 10.1136/bmj.332.7544.777.
- Pauline Beldon (Tissue Viability Nurse Consultant). How To Choose The Appropriate Dressing for Each Wound Type. Wound Essentials Volume 5. Published 2010.




