- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Ambulatory ECG monitoring is a common investigation request. This article provides a concise overview of what an ambulatory ECG is, the length of time commonly requested, clinical indications and how to order and fit an ambulatory ECG device.
What is ambulatory ECG monitoring?
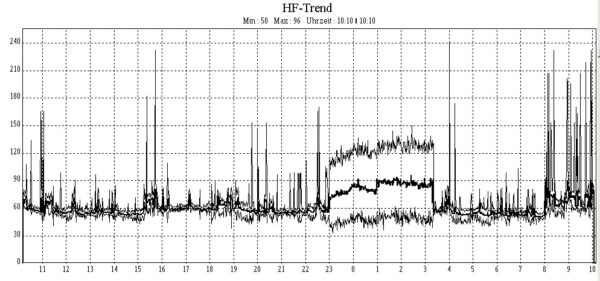
Ambulatory ECG monitoring is a specialist cardiovascular investigation. It allows for a patient’s electrical heart activity, such as rate and rhythm, to be monitored for a prolonged period while the patient is completing normal activities, including resting and sleeping.
This is unlike a resting ECG, which records a patient’s electrical heart activity for around 10 seconds at rest.
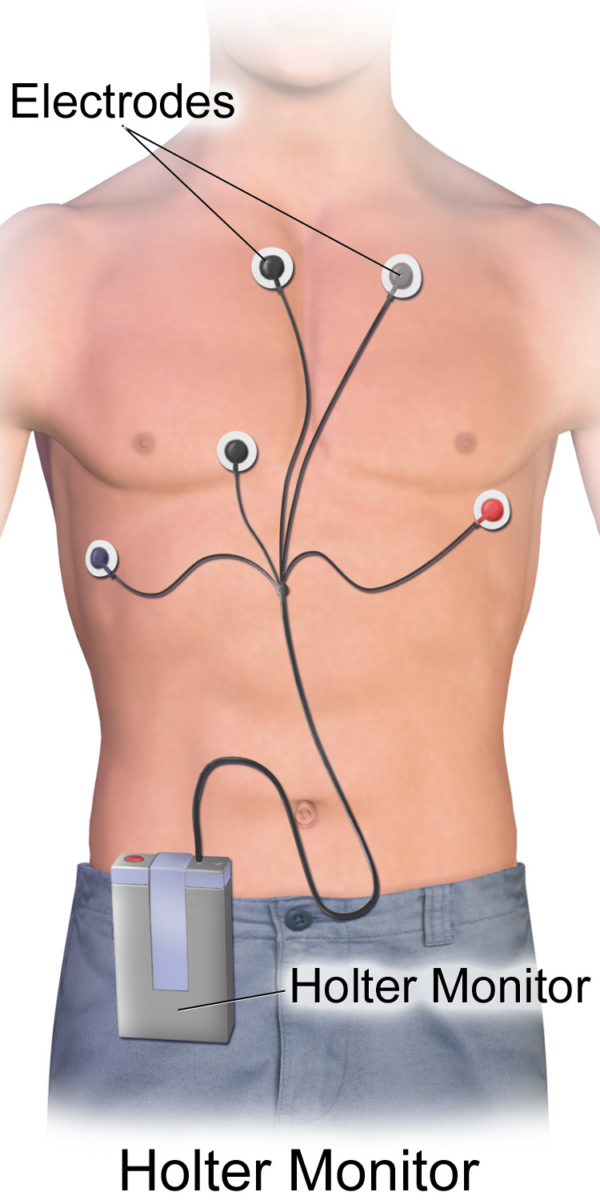
Monitoring uses a small battery-powered wearable device that records the heart’s rhythm. The device is often attached to two or three leads in direct contact with the skin, though some devices use up to 12 leads. This device is sometimes referred to as a Holter monitor.
Study duration types
Monitoring can occur for periods as short as 24 hours and can be extended up to 14 days if necessary. The most commonly requested durations are 24, hours, 72 hours, and 7 days. The longer the duration of the study, the greater the chance of detecting arrhythmic episodes.
The different study types are also often called 24-hour, 72-hour and 7-day ‘tapes’.
Clinical indication
Ambulatory ECG monitoring is useful for evaluating patients with intermittent symptoms, and that are not observed in a resting ECG report.
Common indications include transient loss of consciousness (syncope) and symptoms of chest pain, palpitations, dizziness, and shortness of breath. Other indications include the evaluation of previously diagnosed heart arrhythmias and pacemaker devices in situ.
Atrial fibrillation is a heart arrhythmia that commonly requires ambulatory ECG monitoring as part of the diagnostic stage.1 This is because atrial fibrillation can be paroxysmal in nature with episodes and, if symptomatic, symptoms such as palpitations occurring intermittently.2
An ambulatory ECG monitor may also be indicated to evaluate the effectiveness of atrial fibrillation treatments, such as catheter ablation therapy.
How to request an ambulatory ECG
Ambulatory ECG monitors are often fitted by cardiac physiologists. When you request your ambulatory ECG, it is important that you include the following:
- Patient details, including DOB, ID/Hospital number and home address
- Indication, for example, “palpitations”
- Relevant patient medical and medication history
- A recent 12-lead resting ECG from the patient
Failure to include any of the above may delay your request.
Fitting an ambulatory ECG (Holter) device
Recently, devices have evolved into smaller forms to improve patient comfort and portability. Devices can vary in appearance. Some devices may appear larger than others, depending on the manufacturer and device model. However, all are fundamentally similar in functionality.
Gather equipment
Gather the appropriate equipment:
- Ambulatory ECG device: to record the ECG. Note – ensure the device is fully charged and programmed to the correct study length.
- Self-adhesive ECG electrodes and leads: to attach the ECG device to the patient.
- Razor: to remove hair to provide adequate electrode contact with the skin (if required).
- Anti-bacterial wipe: to clean the skin’s surface (if required).
- Patient diary: to record activities and symptoms throughout the study.
Introduction
Wash your hands and don PPE if appropriate.
Introduce yourself to the patient including your name and role.
Confirm the patient’s name and date of birth.
Briefly explain what the procedure will involve using patient-friendly language: “I need to record an ambulatory ECG which is an electrical trace of the heart. The procedure will involve placing some sticky pads onto your chest. I will then connect these sticky pads to the ECG device. This device will stay in place for the period of time we agreed”
If the patient is a female, explain the need for a chaperone: “One of the female ward staff members will be present throughout the procedure, acting as a chaperone, would that be ok?”
Gain consent to proceed with fitting the ambulatory ECG device.
Ask the patient if they have any allergies, including allergies to metals.
Adequately expose the patient’s chest for the procedure (offer a blanket or examination gown to allow exposure only when required).
Ask the patient to sit on the edge of the clinical examination couch with their back up straight.
Check if the patient has any pain before continuing with the clinical procedure.
Preparation of skin
Ensure the patient’s skin is clean using an antibacterial wipe. This may be particularly important if the skin is oily or visibly soiled.
If necessary, use a razor to shave the relevant sections of the chest. Chest hair can make it difficult to achieve adequate skin contact.
Electrode placement and commencing the study
An ambulatory ECG device often uses one or two leads attached to electrodes across the chest, though some devices use up to 12 leads.
Always connect the device to the electrodes exactly per device instructions. Some ambulatory ECG devices must be turned on manually before or after fitting, whilst others will automatically turn on when in contact with the patient’s skin.
Always read and familiarise yourself with the device’s manual before fitting and commencing the study.
To complete the procedure…
Once the device has been fitted, explain to the patient that the procedure is complete.
Advise the patient to return the device alongside their patient diary after the study been has completed.
Inform the patient that they should keep the monitor away from other electrical devices and away from water (if applicable for the device).
Ensure adequate safety netting, by informing the patient to contact relevant emergency services if they experience any red flag symptoms, such as chest pain.
Thank the patient for their time.
Dispose of PPE appropriately and wash your hands.
Document the start time of the study and device ID/serial number in the patient notes so that the device can be correctly identified when returned.
Reviewer
Dr Richard Jabbour
Consultant Cardiologist
References
- NICE. Diagnosis of atrial fibrillation. Published December 2023. Available from: [LINK]
- NICE. Atrial fibrillation. Published December 2023. Available from: [LINK]
- J. Heuser. Holter Atrial fibrillation. License: [CC BY-SA 3.0]
- Bruce Blaus. Holter Monitor. License: [CC BY-SA 4.0]