- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
Cellulitis and erysipelas are common bacterial infections of the skin. It affects 1 in 40 people per year. Cellulitis typically affects older adults, and around 15% of patients will have an episode of cellulitis in their lifetime.
Aetiology
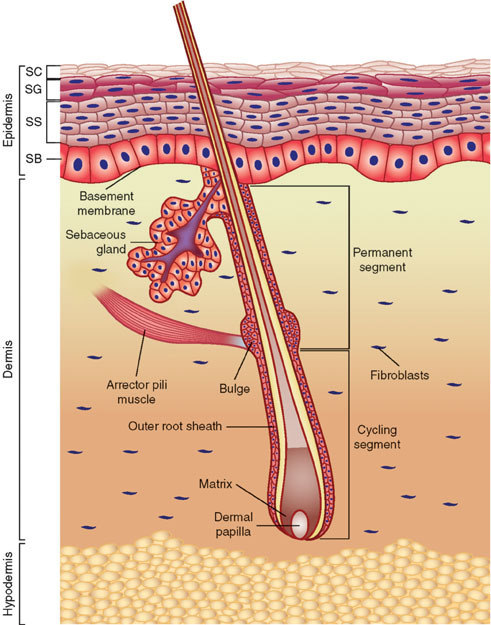
Skin anatomy
Cellulitis affects the deeper layers of the dermis and subcutaneous tissues, usually in the lower limbs. Erysipelas is more superficial and commonly affects the face.
Causative organisms
Common causative organisms include Streptococcus pyogenes and Staphylococcus aureus.
Children or immunocompromised patients, such as those with diabetes, are at risk of infections caused by Strep pneumoniae, H.influenzae and anaerobic bacteria. Clostridium perfringens is an anaerobe and is linked to cases of necrotising fasciitis after surgery (commonly known as gas gangrene).
Risk factors
Risk factors for cellulitis include:
- Trauma: bites, scratches or burns
- Ulcers
- Skin barrier dysfunction: conditions such as eczema or psoriasis
- Peripheral oedema
- Peripheral venous disease
- Peripheral neuropathy
- Immunosuppression: diabetes, neutropenia or immunosuppressant medication
Clinical features
Cellulitis is usually unilateral and most commonly affects the lower limbs.
History
Typical symptoms of cellulitis include:
- Erythema
- Tender skin
- Warmth
- Swelling
- Fevers
Other important areas to cover in the history include:
- Recent trauma to the skin
- Past medical and drug history: immunosuppression
Clinical examination
Typical clinical signs of cellulitis include:
- Erythematous rash: the border may be diffuse or well-demarcated
- Hot and tender to touch
- Oedematous
- Blisters
- Ulcers

Eron classification of cellulitis
- Class 1: Systemically well with no co-morbidities
- Class 2: Systemically unwell or well with poorly controlled co-morbidities
- Class 3: Large SIRS response or very poorly controlled co-morbidities
- Class 4: Septic shock or life-threatening infection
Differential diagnoses
Cellulitis usually presents with a unilateral red and swollen limb, which can be difficult to distinguish from other conditions, such as deep thrombosis (DVT).
Differential diagnoses to consider include:
- Deep vein thrombosis (DVT): unilateral presentation similar to cellulitis but without systemic upset; check for risk factors and use Well’s score to aid diagnosis.
- Venous insufficiency: typically bilateral distribution with venous eczema present
- Lipodermatosclerosis: can be tender and bright red; no systemic features are present. Usually bilateral.
- Septic arthritis: if erythema is overlying joints and reduced range of movement
- Vasculitis: non-blanching rash with palpable petechial/purpuric presentation
- Thrombophlebitis: linear tracking along the path of the affected vein
- Compartment syndrome: swollen, tense and pain to light touch
Bilateral lower limb cellulitis
Bilateral cellulitis is incredibly rare. Patients with bilateral lower limb erythema and swelling are far more likely to have venous insufficiency, lipodermatosclerosis or another underlying cause instead of cellulitis.
Investigations
Bedside investigations
Relevant bedside investigations may include:
- Basic observations (vital signs): to ensure haemodynamic stability
- Wound swab
Laboratory investigations
Relevant laboratory investigations may include:
- Full blood count: raised white cells indicate inflammation
- Urea and electrolytes: as a baseline, renal function may be impaired due to infection
- CRP: raised with inflammation
- Blood cultures
- Venous blood gas: to assess pH and lactate
Imaging
Most cases of cellulitis are managed without imaging. However, an ultrasound of the affected area may be useful to exclude an underlying abscess or deep vein thrombosis (DVT).
X-ray or MRI can be used to investigate for underlying osteomyelitis. X-ray changes can lag behind disease progression. Therefore, definitive imaging should be an MRI.
Management
Most cases of cellulitis are managed in the community; however, it is important to be aware of reasons to arrange hospital admission. These may include:
- Signs of haemodynamic instability
- Rapidly worsening cellulitis
- Facial or orbital cellulitis
- Extremes of age
- Immunocompromised individuals
Patients should always be managed according to how they present clinically. Patients with cellulitis can be acutely unwell and always consider the possibility of sepsis.
Supportive management
All areas of erythema should be outlined to monitor its spread.
Encourage patients to drink plenty of fluids. Ibuprofen and paracetamol can be bought over the counter to manage pain and temperatures.
Patients who are suitable for outpatient management should be reviewed after 48 hours to ensure they respond to oral treatment. If they are not responding, referral to secondary care should occur.
Patients should be safety-netted with advice to seek medical attention if they become systemically unwell, spreading erythema or if they are unable to take their antibiotics.
Medical management
Antibiotics should be prescribed according to severity and allergy status. Flucloxacillin or doxycycline (for those with a penicillin allergy) for 5 – 7 days are standard first-line options but always check local antimicrobial guidelines.
Intravenous antibiotics should be used for severe infections (Eron class 3 or 4) or those that do not respond to oral options.
Outpatient parenteral antimicrobial therapy (OPAT) may be considered for those who require IV antibiotics but are clinically stable (Class 2).
IV fluids can be used if a patient is dehydrated with poor oral fluid intake.
Prophylaxis
Specialists may consider prophylactic antibiotics if there have been two separate episodes of cellulitis within the last 12 months. The first choice of antibiotic would be low-dose penicillin (erythromycin in penicillin-allergic patients).
Complications
Complications of cellulitis include:
- Sepsis
- Abscess formation
- Recurrence of infection
- Ulceration
- Post-streptococcal nephritis
- Osteomyelitis
- Compartment syndrome
- Necrotising fasciitis
Necrotising fasciitis
Necrotising fasciitis is a severe complication of cellulitis which needs to be excluded.
It typically presents with rapidly progressive erythema, crepitus, disproportional pain to stimuli and necrotic lesions. The mainstay of treatment is urgent surgical debridement and IV antibiotics.
Key points
- Cellulitis is caused by bacterial infection of the dermis and subcutaneous tissues
- Typical symptoms include erythema, fevers and pain
- Typical clinical signs include tender leg, warmth to touch and oedema
- Management typically can be as an outpatient using oral antibiotics
- Hospital admission is required for patients who are systemically unwell or in at-risk groups
- Common complications include recurrent infections, sepsis and abscesses
- Necrotising fasciitis is a rare but severe complication of cellulitis that presents with rapidly progressive erythema, pain, and necrotic lesions.
Reviewer
Dr Ehi Okpe
Consultant in Acute Internal Medicine
Editor
Dr Chris Jefferies
References
- NICE CKS. Cellulitis. Published in 2023. Available from: [LINK]
- Patient UK. Cellulitis and Erysipelas. Published in 2020. Available from: [LINK]
- Diagnosis and management of cellulitis. Published in 2018. Available from: [LINK]
- Santer, M et al. Management of cellulitis: current practice and research questions. Published in 2018. Available from: [LINK]
- DermNet. Cellulitis mimics. Published in 2018. Available from: [LINK]
Image references
- Figure 1. Wong, D.J. and Chang, H.Y.Anatomy of the skin. License: [CC BY]
- Figure 2. Campbell. Cellulitis left leg. Licence: [Public domain]




