- 📖 Geeky Medics OSCE Book
- ⚡ Geeky Medics Bundles
- ✨ 1300+ OSCE Stations
- ✅ OSCE Checklist PDF Booklet
- 🧠 UKMLA AKT Question Bank
- 💊 PSA Question Bank
- 💉 Clinical Skills App
- 🗂️ Flashcard Collections | OSCE, Medicine, Surgery, Anatomy
- 💬 SCA Cases for MRCGP
To be the first to know about our latest videos subscribe to our YouTube channel 🙌
Introduction
The carotid body is a small group of cells, including chemoreceptors, located at the bifurcation of the common carotid artery. The carotid body’s function is to detect changes in the composition of arterial blood flow including the partial pressure of oxygen/carbon dioxide, pH and temperature. This information is relayed to the cardiorespiratory centres in the medulla oblongata via the glossopharyngeal nerve.
Carotid body tumours (a.k.a. carotid paragangliomas or CBTs) can sometimes develop within the carotid body causing compression of local structures as well as systemic symptoms (if secretory).1
Risk factors
CBTs are mostly solitary, however, there are few associations:
- Familial CBTs: these account for 10% of cases.2 Mutations in succinate dehydrogenase (SDH) gene subunits have been identified with this hereditary form of CBTs. The SDHD mutation is the most common inherited abnormality in familial CBT.
- MEN1 and MEN2 (phaeochromocytoma)
- Neurofibromatosis 2
- Von-Hippel Lindau syndrome
- Carney triad: a rare syndrome consisting of a gastrointestinal stromal tumour, pulmonary chondroma and extra-adrenal paraganglioma
All patients with a family history of CBTs/phaeochromocytoma should be offered genetic testing.
Clinical features
History
Typical symptoms of CBTs include:
- Slow growing, painless, lateral cervical mass
- Odynophagia
- Dysphagia
- Hoarseness
- Ptosis
Other symptoms may include:
- Syncope, as a result of carotid sinus syndrome (triggered by palpation of the carotid artery or sudden neck movements)3
- Palpitations, sweating and headache (in the context of secretory tumours)
Clinical examination
Typical clinical findings in the context of a CBT include a painless mass located in the carotid triangle at the bifurcation of the carotid arteries.
Palpation of a CBT, as part of a neck lump examination, may reveal:
- Variable consistency (soft or firm)
- Partial mobility (able to move laterally, but not superior/inferiorly due to fixation to the carotid artery)
- Pulsatility (due to the underlying carotid artery)
- Bruit on auscultation (due to turbulent blood flow in the context of local carotid artery compression by the tumour)
Cranial nerve examination may reveal features of Horner’s syndrome on the affected side, including:
- Partial ptosis
- Miosis
- Anhidrosis
Other clinical features may include:
- Hoarseness
- Tachycardia and sweating (in the context of secretory tumours which only account for 5% of cases)4
- Bilateral CBTs (10-18% of cases)5
Differential diagnoses
Possible differential diagnoses for a suspected CBT include:
- Lymphadenopathy
- Peripheral nerve neoplasms
- Salivary gland neoplasm
- Branchial cleft anomaly
Investigations
Laboratory investigations
Urine sample
A 24-hour urine sample can be used to identify catecholamines produced by secretory CBTs including:
- Metanephrine
- Norepinephrine
- Epinephrine
- Dopamine
Abnormally elevated catecholamine levels should prompt further imaging to rule out synchronous paragangliomas and phaeochromocytoma.
Imaging
Various imaging modalities are utilised in the workup of CBTs including CT, MRI and radionuclide scans.
CT neck with contrast
Typical findings on CT neck with contrast:
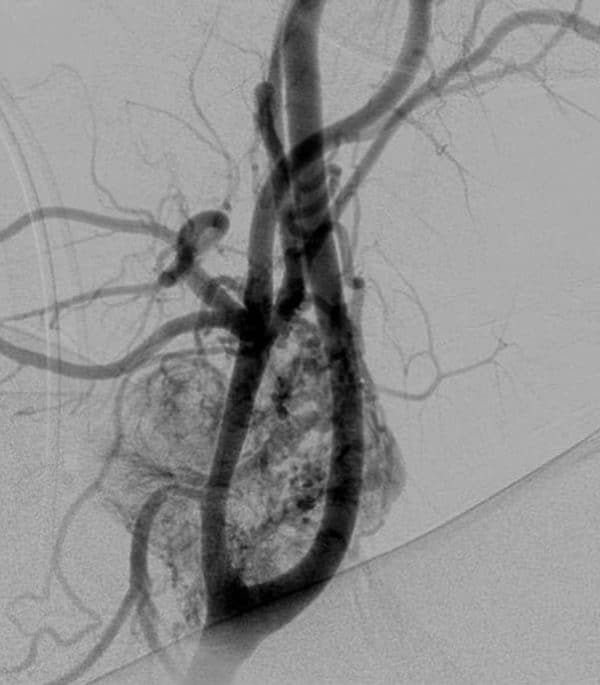
- Hypervascular mass with avid contrast enhancement at the level of the carotid bifurcation, splaying the internal and external branches (often described as the ‘Lyre sign’ – Figure 1)
MRI with gadolinium
Typical findings on MRI:
- T2-weighted images demonstrate flow voids, characteristic of vascular structures
Radionuclide techniques
An MIBG scan is a nuclear medicine imaging test. It combines a small amount of radioactive material with a substance called metaiodobenzylguanidine (MIBG) to find certain types of tumours in the body.
Carotid body tumours and phaeochromocytomas both demonstrate increased uptake of MIBG allowing primary lesions and metastases to be identified.7
Classification
The most widely recognised classification system for CBTs is the Shamblin classification, based on the degree of encasement of the carotid arteries. This, in turn, reflects the difficulty of resection.8
Management
Surgery
Open surgical excision remains the mainstay of treatment for CBTs. Vascular control is key to success in this operation and requires early control of the common carotid artery and its branches. The structures at highest risk during this procedure are the hypoglossal nerve and the superior laryngeal nerve.
Embolization
Preoperative embolization is increasingly being utilised, primarily to reduce intra-operative blood loss. Surgery should be scheduled within 24-48 hours of embolization to prevent revascularisation and local inflammation.
Radiation therapy (RT)
Radiation therapy (RT) is used to arrest the growth of CBTs.
RT is reserved for the following situations:
- Surgery is contraindicated due to poor performance status or locally advanced tumours
- Adjuvant therapy following surgery for malignant CBTs
Observation
A wait-and-scan policy may be adopted in some situations including:
- Those patients not amenable to surgery or RT due to poor performance status
- Patient preference, following an informed discussion of treatment options
- Malignant CBT with distant metastasis
Complications
Complications of the surgical management of CBTs include:
- Bleeding (arising from injury to the carotid arteries)
- Stroke (4%)9
- Injury to cranial nerves: hypoglossal or vagus (17%)9
- Local recurrence
- Death
Key points
- The carotid body is a small group of cells, including chemoreceptors, located at the bifurcation of the common carotid artery.
- CBTs can sometimes develop within the carotid body causing compression of local structures as well as systemic symptoms (if secretory).
- Imaging studies including CT neck with contrast, MRI and radionuclide techniques are used to diagnose CBTs.
- Surgical excision, with or without pre-operative embolization, is the preferred method of management.
- Complications of CBT surgery include cranial nerve palsy (hypoglossal, superior laryngeal) and embolic stroke.
References
- Katabi N, Lewis JS. Update from the 4th edition of the World Health Organization classification of head and neck tumours: what is new in the 2017 WHO blue book for tumours and tumour-like lesions of the neck and lymph nodes. Published in 2017. Available from: [LINK]
- Martin TP, Irving RM, Maher ER. The genetics of paragangliomas: a review. Published in 2007. Available from: [LINK]
- Rosenkranz L, Schell AR. Carotid body tumour as a reversible cause of recurrent syncope. Published in 1984. Available from: [LINK]
- Else T, Greenberg S, Fishbein L. Hereditary Paraganglioma-Pheochromocytoma Syndromes. Published in 2008. Available from: [LINK]
- Sajid MS, Hamilton G, Baker DM. A multicenter review of carotid body tumour management. Published in 2007. Available from: [LINK]
- JN Rutledge. Carotid Body tumour. License: [CC BY-SA 4.0]. Available from: [LINK]
- Taïeb D, Timmers HJ, Hindié E, Guillet BA, Neumann HP, Walz MK, Opocher G, De Herder WW, Boedeker CC, De Krijger RR, Chiti A. EANM 2012 guidelines for radionuclide imaging of phaeochromocytoma and paraganglioma. Published in 2012. Available from: [LINK]
- Shamblin WR, ReMine WH, Sheps SG, Harrison EG. Carotid body tumour (chemodectoma): clinicopathologic analysis of ninety cases. Published in 1971. Available from: [LINK]
- Robertson V, Poli F, Hobson B, Saratzis A, Naylor AR. A systematic review and meta-analysis of the presentation and surgical management of patients with carotid body tumours. Published in 2019. Available from: [LINK]
Reviewer
Mr Benjamin Miller
ENT Registrar




